No products in the cart.
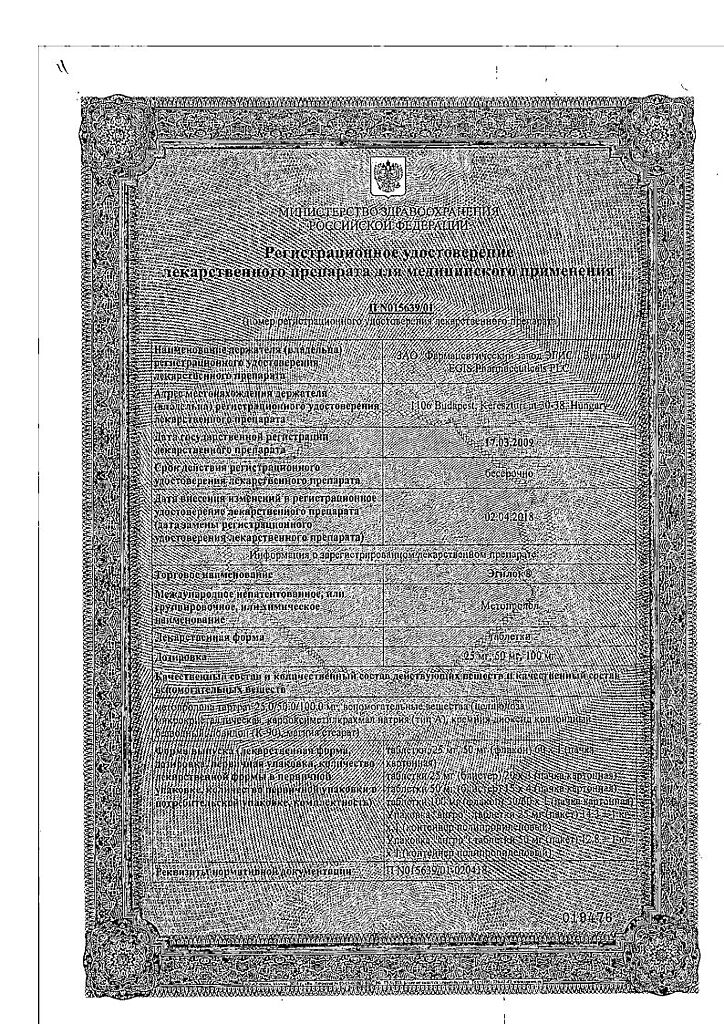
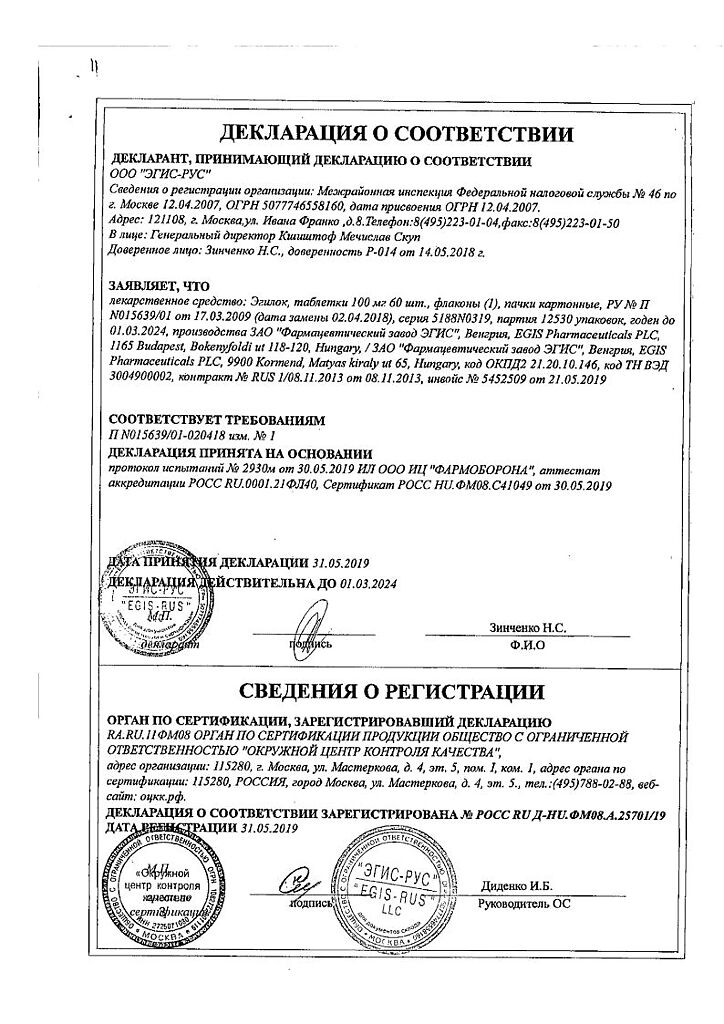
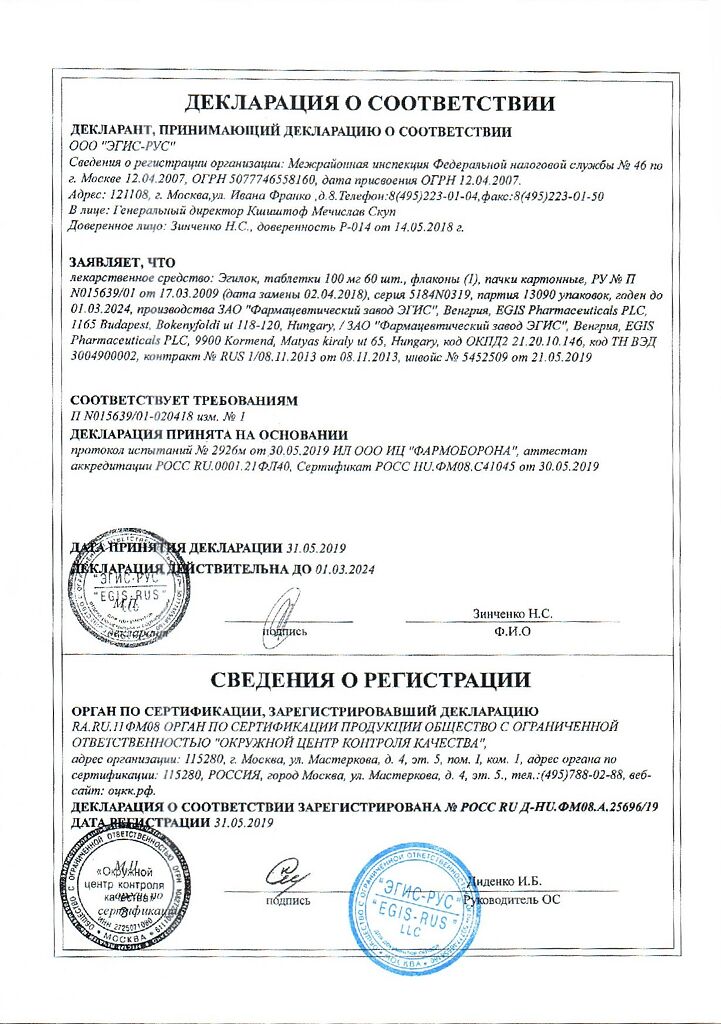
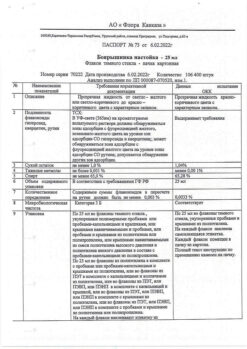
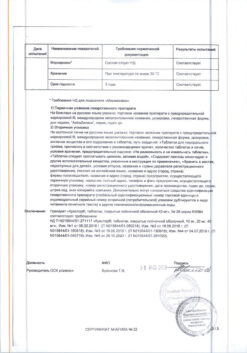
Egilok, tablets 100 mg 60 pcs
€6.12 €5.44
Description
Pharmgroup:
A beta1-adrenoblocker selective.
Pharmic action:
Egilok is a cardioselective β-adrenoreceptor blocker with no intrinsic sympathomimetic and membrane-stabilizing activity. It has antihypertensive, antianginal and antiarrhythmic action.
Blocking in low doses of cardiac β1-adrenoceptors, reduces catecholamine-stimulated formation of cAMP from ATP, decreases intracellular Ca2+ flow, produces negative chrono-, dromo-, batmo- and inotropic action (decreases HR, inhibits conduction and excitability, reduces myocardial contractility).
The HRPS at the beginning of drug administration (within the first 24 hours after oral administration) increases, after 1-3 days of use it returns to the baseline level, and with further use it decreases.
The antihypertensive effect is caused by the decrease of cardiac output and renin synthesis, inhibition of the activity of renin-angiotensin system and CNS, restoration of sensitivity of aortic arch baroreceptors (there is no increase of their activity in response to a decrease of BP) and as a result, a decrease of peripheral sympathetic effects. Reduces elevated BP at rest, under physical stress and strain.
The BP decreases in 15 min, maximum in 2 h; action lasts for 6 h. Stable decrease is observed after several weeks of regular use.
The antianginal effect is determined by decrease of myocardial oxygen demand as a result of decrease of HR (prolongation of diastole and improvement of myocardial perfusion) and contractility and decrease of myocardial sensitivity to sympathetic innervation. It reduces the frequency and severity of angina attacks and increases exercise tolerance.
The antiarrhythmic effect is caused by the removal of arrhythmogenic factors (tachycardia, increased activity of the sympathetic nervous system, increase of cAMP, arterial hypertension), decrease of spontaneous excitation rate of sinus and ectopic pacemakers and slowing of AV conduction (mainly in the antegrade and, to a lesser degree, in the retrograde direction through the AV node) and through additional pathways.
In supraventricular tachycardia, atrial fibrillation, sinus tachycardia in functional heart disease and hyperthyroidism, it slows the HR and may even lead to restoration of sinus rhythm.
Prevent the development of migraine.
Long-term use reduces blood cholesterol.
In medium therapeutic doses, it has less effect on the organs containing β2-adrenoreceptors (pancreas, skeletal muscles, smooth muscles of peripheral arteries, bronchi, uterus) and on carbohydrate metabolism.
When used in high doses (more than 100 mg/day) it has a blocking effect on both subtypes of β-adrenoreceptors.
Pharmacokinetics:
Absorption
It is rapidly and completely (95%) absorbed from the GI tract. Cmax in plasma is reached 1.5-2 hours after oral administration. Bioavailability is 50%. During treatment the bioavailability increases to 70%. Food intake increases bioavailability by 20-40%.
Distribution
Vd is 5.6 l/kg. Binding with blood plasma proteins is 12%. It penetrates through the HEB and the placental barrier. It is excreted with breast milk in small amounts.
Metabolism
Metoprolol is biotransformed in the liver. Metabolites have no pharmacological activity.
Elimation
T1/2 averages 3.5-7 h. Metoprolol is almost completely excreted in the urine in 72 hours. About 5% of the dose is excreted unchanged.
Pharmacokinetics in special clinical cases
The bioavailability and T1/2 of metoprololol increase with marked hepatic impairment, which may require adjustment of the drug dose.
In impaired renal function, the T1/2 and systemic clearance of metoprololol do not change significantly.
Indications
Indications
– arterial hypertension (in monotherapy or in combination with other antihypertensive drugs);
– chronic heart failure in the compensation stage (in addition to standard therapy with diuretics, ACE inhibitors, cardiac glycosides);
– IHD (secondary prevention of myocardial infarction, prevention of angina attacks);
– heart rhythm disturbances (supraventricular arrhythmias, ventricular extrasystole);
– hyperkinetic cardiac syndrome;
– hyperthyroidism (as part of complex therapy);
– prevention of migraine attacks.
Pharmacological effect
Pharmacological effect
Pharmaceutical group:
selective beta1-blocker.
Pharmaceutical action:
Egilok is a cardioselective β-adrenergic receptor blocker that does not have internal sympathomimetic and membrane-stabilizing activity. Has antihypertensive, antianginal and antiarrhythmic effects.
By blocking β1-adrenergic receptors of the heart in low doses, it reduces the catecholamine-stimulated formation of cAMP from ATP, reduces the intracellular Ca2+ current, has a negative chrono-, dromo-, bathmo- and inotropic effect (reduces heart rate, inhibits conductivity and excitability, reduces myocardial contractility).
At the beginning of the drug’s use (in the first 24 hours after oral administration), the OPSS increases, after 1-3 days of use it returns to the initial level, and with further use it decreases.
The antihypertensive effect is due to a decrease in cardiac output and renin synthesis, inhibition of the activity of the renin-angiotensin system and the central nervous system, restoration of the sensitivity of the baroreceptors of the aortic arch (there is no increase in their activity in response to a decrease in blood pressure) and, ultimately, a decrease in peripheral sympathetic influences. Reduces high blood pressure at rest, during physical exertion and stress.
Blood pressure decreases after 15 minutes, maximum after 2 hours; the effect lasts for 6 hours. A stable decrease is observed after several weeks of regular use.
The antianginal effect is determined by a decrease in myocardial oxygen demand as a result of a decrease in heart rate (prolongation of diastole and improvement of myocardial perfusion) and contractility, as well as a decrease in the sensitivity of the myocardium to the effects of sympathetic innervation. Reduces the frequency and severity of angina attacks and increases exercise tolerance.
The antiarrhythmic effect is due to the elimination of arrhythmogenic factors (tachycardia, increased activity of the sympathetic nervous system, increased cAMP content, arterial hypertension), a decrease in the rate of spontaneous excitation of sinus and ectopic pacemakers and a slowdown of AV conduction (mainly in the antegrade and, to a lesser extent, in the retrograde directions through the AV node) and along additional pathways.
With supraventricular tachycardia, atrial fibrillation, sinus tachycardia in functional heart diseases and hyperthyroidism, it slows down the heart rate and can even lead to the restoration of sinus rhythm.
Prevents the development of migraine.
When taken for many years, it reduces cholesterol levels in the blood.
When used in average therapeutic doses, it has a less pronounced effect on organs containing β2-adrenergic receptors (pancreas, skeletal muscles, smooth muscles of peripheral arteries, bronchi, uterus) and on carbohydrate metabolism.
When used in high doses (more than 100 mg/day), it has a blocking effect on both subtypes of β-adrenergic receptors.
Pharmacokinetics:
Suction
Quickly and completely (95%) absorbed from the gastrointestinal tract. Cmax in plasma is achieved 1.5-2 hours after oral administration. Bioavailability is 50%. During treatment, bioavailability increases to 70%. Eating increases bioavailability by 20-40%.
Distribution
Vd is 5.6 l/kg. Plasma protein binding – 12%. Penetrates the BBB and placental barrier. Excreted in breast milk in small quantities.
Metabolism
Metoprolol is biotransformed in the liver. Metabolites do not have pharmacological activity.
Removal
T1/2 averages 3.5-7 hours. Metoprolol is almost completely excreted in the urine within 72 hours. About 5% of the dose is excreted unchanged.
Pharmacokinetics in special clinical situations
With severe liver dysfunction, the bioavailability and T1/2 of metoprolol increases, which may require dose adjustment of the drug.
If renal function is impaired, T1/2 and systemic clearance of metoprolol do not change significantly.
Special instructions
Special instructions
When prescribing Egilok, heart rate and blood pressure should be regularly monitored. The patient should be warned that if the heart rate is less than 50 beats/min, a doctor’s consultation is necessary.
In patients with diabetes mellitus, blood glucose levels should be regularly monitored and, if necessary, the dose of insulin or oral hypoglycemic drugs should be adjusted.
Prescribing Egilok to patients with chronic heart failure is possible only after reaching the compensation stage.
In patients taking Egilok, the severity of hypersensitivity reactions may increase (against the background of a burdened allergic history) and there may be no effect from the administration of usual doses of epinephrine (adrenaline).
The use of Egilok may worsen the symptoms of peripheral circulatory disorders.
Egilok should be discontinued gradually, gradually reducing its dose over 10 days. If treatment is abruptly stopped, withdrawal syndrome may occur (increased angina attacks, increased blood pressure). During drug withdrawal, patients with angina pectoris should be under close medical supervision.
For exertional angina, the selected dose of the drug should ensure the heart rate at rest within the range of 55-60 beats/min, and during exercise – no more than 110 beats/min.
Patients who use contact lenses should take into account that during treatment with beta-blockers, there may be a decrease in the production of tear fluid.
Metoprolol may mask some clinical manifestations of hyperthyroidism (tachycardia). Abrupt withdrawal in patients with thyrotoxicosis is contraindicated because it can increase symptoms.
In case of diabetes mellitus, taking Egilok can mask the symptoms of hypoglycemia (tachycardia, sweating, increased blood pressure).
When prescribing metoprolol to patients with bronchial asthma, simultaneous use of beta2-adrenergic agonists is necessary.
In patients with pheochromocytoma, Egilok should be used in combination with alpha-blockers.
Before performing any surgical intervention, it is necessary to inform the anesthesiologist about the therapy being carried out with Egilok (choosing a drug for general anesthesia with minimal negative inotropic effect); discontinuation of the drug is not required.
When prescribing the drug to elderly patients, liver function should be regularly monitored. Correction of the dosage regimen is required only if increasing bradycardia, a pronounced decrease in blood pressure, AV blockade, bronchospasm, ventricular arrhythmias, and severe liver dysfunction appear in elderly patients. Sometimes it is necessary to stop treatment.
Special monitoring should be carried out in patients with a history of depressive disorders. If depression develops, Egilok should be discontinued.
Use in pediatrics
The effectiveness and safety of Egilok in children and adolescents under 18 years of age have not been determined.
Impact on the ability to drive vehicles and operate machinery
In patients whose activities require increased attention, the question of prescribing the drug on an outpatient basis should be decided only after assessing the patient’s individual response.
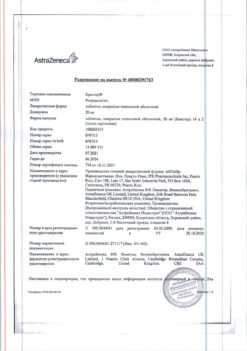
Active ingredient
Active ingredient
Metoprolol
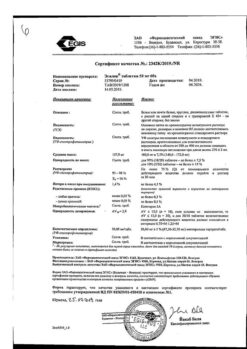
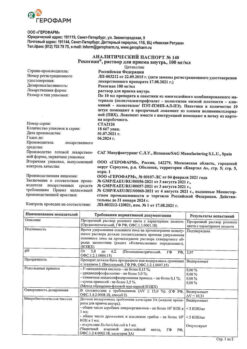
Composition
Composition
1 tablet contains metoprolol tartrate 100 mg;
excipients:
MCC;
sodium carboxymethyl starch;
anhydrous colloidal silicon dioxide;
povidone;
magnesium stearate.
Contraindications
Contraindications
– cardiogenic shock;
– AV blockade II and III degrees;
– sinoatrial blockade;
– SSSU;
– severe bradycardia (heart rate less than 50 beats/min);
– heart failure in the stage of decompensation;
– angiospastic angina (Prinzmetal angina);
– severe arterial hypotension (systolic blood pressure below 100 mm Hg);
– lactation period;
– simultaneous use of MAO inhibitors;
– simultaneous intravenous administration of verapamil;
– hypersensitivity to metoprolol and other ingredients of the drug.
The drug should be prescribed with caution for diabetes mellitus, metabolic acidosis, bronchial asthma, chronic obstructive pulmonary disease (pulmonary emphysema, chronic obstructive bronchitis), obliterating diseases of peripheral vessels (intermittent claudication, Raynaud’s syndrome), liver failure, chronic renal failure, myasthenia gravis, pheochromocytoma, AV block of the first degree, thyrotoxicosis, depression (including a history), psoriasis, as well as in children and adolescents under the age of 18 and in elderly patients.
Side Effects
Side Effects
From the central nervous system and peripheral nervous system: increased fatigue, weakness, headache, slower speed of mental and motor reactions; rarely – paresthesia in the extremities, depression, anxiety, decreased ability to concentrate, drowsiness, insomnia, nightmares, confusion or short-term memory impairment, asthenic syndrome, muscle weakness.
From the senses: rarely – decreased vision, decreased secretion of tear fluid, xerophthalmos, conjunctivitis, tinnitus.
From the cardiovascular system: sinus bradycardia, palpitations, decreased blood pressure, orthostatic hypotension; rarely – decreased myocardial contractility, temporary worsening of symptoms of chronic heart failure, arrhythmias, increased peripheral circulatory disorders (coldness of the lower extremities, Raynaud’s syndrome), myocardial conduction disorders; in isolated cases – AV block, cardialgia.
From the digestive system: nausea, vomiting, abdominal pain, diarrhea, constipation, dry mouth, change in taste; increased activity of liver transaminases; rarely – hyperbilirubinemia.
Dermatological reactions: urticaria, skin itching, rash, exacerbation of psoriasis, psoriasis-like skin changes, skin hyperemia, exanthema, photodermatosis, increased sweating, reversible alopecia.
From the respiratory system: nasal congestion, difficulty exhaling (bronchospasm when prescribed in high doses or in predisposed patients), shortness of breath.
From the endocrine system: hypoglycemia (in patients receiving insulin); rarely – hyperglycemia.
From the hematopoietic system: thrombocytopenia, agranulocytosis, leukopenia.
Other: back or joint pain, slight weight gain, decreased libido and/or potency.
Interaction
Interaction
With simultaneous use of Egilok with MAO inhibitors, a significant increase in the hypotensive effect is possible. The break between taking MAO inhibitors and Egilok should be at least 14 days.
Simultaneous intravenous administration of verapamil can provoke cardiac arrest; simultaneous administration of nifedipine leads to a significant decrease in blood pressure.
Inhalation anesthetics (hydrocarbon derivatives) when used simultaneously with Egilok increase the risk of inhibition of myocardial contractile function and the development of arterial hypotension.
When used simultaneously, beta-agonists, theophylline, cocaine, estrogens, indomethacin and other NSAIDs reduce the hypotensive effect of Egilok.
With the simultaneous use of Egilok and ethanol, an increased inhibitory effect on the central nervous system is observed.
When Egilok is used simultaneously with ergot alkaloids, the risk of peripheral circulatory disorders increases.
When used simultaneously, Egilok increases the effect of oral hypoglycemic drugs and insulin and increases the risk of developing hypoglycemia.
When Egilok is used simultaneously with antihypertensive drugs, diuretics, nitrates, and calcium channel blockers, the risk of developing arterial hypotension increases.
With simultaneous use of Egilok with verapamil, diltiazem, antiarrhythmic drugs (amiodarone), reserpine, methyldopa, clonidine, guanfacine, agents for general anesthesia and cardiac glycosides, an increase in the severity of the decrease in heart rate and inhibition of AV conduction may be observed.
Inducers of microsomal liver enzymes (rifampicin, barbiturates) accelerate the metabolism of metoprolol, which leads to a decrease in the concentration of metoprolol in the blood plasma and a decrease in the effect of Egilok.
Inhibitors of microsomal liver enzymes (cimetidine, oral contraceptives, phenothiazines) increase the concentration of metoprolol in the blood plasma.
Allergens used for immunotherapy or allergen extracts for skin testing when used together with Egilok increase the risk of systemic allergic reactions or anaphylaxis.
Iodine-containing radiopaque agents for intravenous administration when used simultaneously with Egilok increase the risk of developing anaphylactic reactions.
Egilok, when used simultaneously, reduces the clearance of xanthines, especially in patients with initially increased clearance of theophylline under the influence of smoking.
When used simultaneously with Egilok, the clearance of lidocaine decreases and the concentration of lidocaine in plasma increases.
With simultaneous use, Egilok enhances and prolongs the effect of non-depolarizing muscle relaxants; prolongs the effect of indirect anticoagulants.
When used together with ethanol, the risk of a pronounced decrease in blood pressure increases.
Overdose
Overdose
Symptoms: severe sinus bradycardia, dizziness, nausea, vomiting, cyanosis, arterial hypotension, arrhythmia, ventricular extrasystole, bronchospasm, fainting; in case of acute overdose – cardiogenic shock, loss of consciousness, coma, AV blockade up to the development of complete transverse block and cardiac arrest, cardialgia.
The first signs of overdose appear 20 minutes to 2 hours after administration.
Treatment: gastric lavage, administration of adsorbents, symptomatic therapy: in case of a pronounced decrease in blood pressure – Trendelenburg position, in case of acute arterial hypotension, bradycardia and threatening heart failure – intravenous (with an interval of 2-5 minutes) administration of beta-adrenergic stimulants or intravenous administration of 0.5-2 mg of atropine sulfate, in the absence of a positive effect – dopamine, dobutamine or norepinephrine.
As subsequent measures, it is possible to prescribe 1-10 mg of glucagon and install a transvenous intracardial pacemaker. For bronchospasm – intravenous administration of beta2-adrenergic stimulants, for convulsions – slow intravenous administration of diazepam. Metoprolol is poorly excreted by hemodialysis.
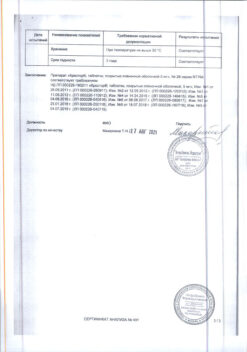
Storage conditions
Storage conditions
At 15–25 °C
Shelf life
Shelf life
5 years
Manufacturer
Manufacturer
EGIS, Hungary
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | At 15-25 °C |
| Manufacturer | EGIS, Hungary |
| Medication form | pills |
| Brand | EGIS |
Other forms…
Related products
Buy Egilok, tablets 100 mg 60 pcs with delivery to USA, UK, Europe and over 120 other countries.