No products in the cart.
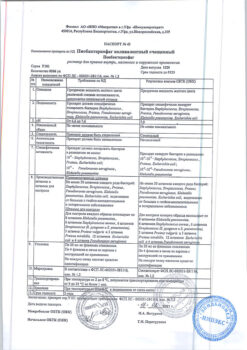
Ecoral, 100 mg/ml 50 ml
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group
Immunosuppressive agent
Pharmacodynamics:
Ecoral® (cyclosporine A) is a cyclic polypeptide consisting of 11 amino acids and is a powerful immunosuppressive agent.
At the cellular level, cyclosporine inhibits the formation and release of lymphokines including interleukin-2 (T-lymphocyte growth factor). Cyclosporine blocks resting lymphocytes in the G0 or G1 phase of the cell cycle and inhibits antigen-dependent release of lymphokines by activated T lymphocytes. All these data indicate that cyclosporine acts on lymphocytes specifically and reversibly.
Cyclosporine does not inhibit hematopoiesis and does not affect the function of phagocytic cells.
Pharmacokinetics:
After oral administration of cyclosporine, its maximum concentration in the blood is observed between 1 and 6 hours, with bioavailability averaging 30% (20 to 50%) and increasing with increasing dose and duration of treatment. Absorption decreases after liver transplantation in liver disease or gastrointestinal pathology (diarrhea vomiting ileus).
It is intensively bound to proteins and blood cells (concentration in whole blood is 2-9 times higher than in plasma). Protein binding is 90% (mainly with lipoproteins). It is distributed mainly outside the bloodstream; it is present in plasma – 33-47%; lymphocytes – 4-9% in granulocytes – 5-12% in erythrocytes – 41-58%. Time of reaching maximum concentration (TSmax) in plasma is 15-35 hours after oral administration. Metabolized by the liver by P450 3A enzyme and to a lesser extent by the gastrointestinal system by the kidneys. Excreted with the bile; by the kidneys – 6% of the administered oral dose. Excreted with breast milk. Cyclosporine is extensively metabolized to form 15 identified metabolites.
The T½ (half-life) is 19 hours in adults and 7 hours in children regardless of dose or route of administration.
Indications
Indications
Transplantation
Solid organ transplantation: prevention of graft rejection after allogeneic transplantation of a kidney, liver, heart, lung, pancreas, heart-lung complex. Treatment of transplant rejection in patients previously treated with other immunosuppressive drugs.
Bone marrow transplantation: prevention of graft rejection after bone marrow transplantation; prevention and treatment of graft-versus-host disease (GVHD).
Indications not related to transplantation
Endogenous uveitis (active sight-threatening uveitis of the middle and posterior part of the eye of non-infectious etiology if conventional therapy does not produce results or leads to severe adverse reactions); Behcet’s uveitis (with recurrent attacks of inflammation affecting the retina).
Nephrotic syndrome: steroid-dependent and steroid-resistant nephrotic syndrome caused by glomerular pathology such as minimal change nephropathy, focal and segmental glomerulosclerosis or membranous glomerulonephritis (in order to achieve and maintain remission, as well as to support remission caused by glucocorticosteroids, which will allow the abolition of glucocorticosteroid therapy).
Rheumatoid arthritis: severe forms of highly active rheumatoid arthritis when traditional slow-acting antirheumatic drugs are ineffective or cannot be used.
Psoriasis: severe forms of psoriasis when traditional therapy is ineffective or impossible.
Atopic dermatitis: severe forms of atopic dermatitis when traditional therapy is ineffective or impossible.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Immunosuppressant
Pharmacodynamics:
Ecoral® (cyclosporine A) is a cyclic polypeptide consisting of 11 amino acids and is a powerful immunosuppressive agent.
At the cellular level, cyclosporine inhibits the formation and release of lymphokines including interleukin-2 (T-lymphocyte growth factor). Cyclosporine blocks quiescent lymphocytes in the G0 or G1 phase of the cell cycle and inhibits the antigen-dependent release of lymphokines by activated T lymphocytes. All data obtained indicate that cyclosporine acts specifically and reversibly on lymphocytes.
Cyclosporine does not inhibit hematopoiesis and does not affect the function of phagocytic cells.
Pharmacokinetics:
After taking cyclosporine orally, its maximum concentration in the blood is observed in the range from 1 to 6 hours, and its bioavailability averages 30% (from 20 to 50%) and increases with increasing dose and duration of treatment. Absorption decreases after liver transplantation for liver disease or gastrointestinal pathology (diarrhea, vomiting, ileus).
Intensively binds to proteins and formed elements of blood (concentration in whole blood is 2-9 times higher than in plasma). Protein binding – 90% (mainly with lipoproteins). Distributed mainly outside the bloodstream; present in plasma 33-47%; lymphocytes – 4-9% in granulocytes 5-12% in erythrocytes – 41-58%. The time to reach maximum concentration (TCmax) in plasma is 15-35 hours after oral administration. Metabolized by the liver by the enzyme P450 3A and to a lesser extent by the gastrointestinal system by the kidneys. Excreted in bile; kidneys – 6% of the administered oral dose. Excreted in breast milk. Cyclosporine is extensively metabolized to form 15 identified metabolites.
T½ (half-life) is 19 hours in adults and 7 hours in children, regardless of dose or route of administration.
Special instructions
Special instructions
The drug Ecoral® can only be used by a doctor who has experience in immunosuppressive therapy and has the ability to organize appropriate monitoring of the patient, including a regular full physical examination, measuring blood pressure and monitoring the concentration of creatinine in the blood serum. Monitoring of transplant patients receiving the drug should be carried out only in those institutions that are provided with trained medical personnel and appropriate laboratory resources.
It should be borne in mind that when using cyclosporine, as well as other immunosuppressive drugs, the risk of developing lymphomas and other malignant neoplasms, especially of the skin, increases. The increased risk of developing these complications depends more on the degree and duration of immunosuppression than on the specific drug. Therefore, caution should be exercised when using combined immunosuppressive therapy regimens, keeping in mind the likelihood of developing lymphoproliferative diseases and solid malignancies, sometimes leading to death.
Given the potential risk of developing skin malignancies, patients treated with cyclosporine should avoid excessive exposure to direct sunlight and exposure to ultraviolet radiation (ultraviolet B (UVB)) PUVA therapy (photochemotherapy).
The use of cyclosporine, like other immunosuppressive drugs, predisposes to the development of various bacterial, fungal, parasitic and viral infections, often involving opportunistic pathogens. Reactivation of polyomavirus from latency can lead to the development of PVAN or PMLEP. Such conditions are often associated with a high degree of immunosuppression and should be considered in the differential diagnosis of the causes of renal and nervous system dysfunction in patients receiving immunosuppressive therapy. Considering the potential danger of these infections for the patient’s life, an effective system of preventive and therapeutic measures should be used, especially in cases of long-term use of combined immunosuppressive treatment.
During the first few weeks of therapy with Ecoral®, a frequent and potentially dangerous complication may occur – an increase in the concentration of creatinine and urea in the blood serum. These functional changes are reversible and dose-dependent, usually normalizing with dose reduction. With long-term treatment, some patients may develop structural changes in the kidneys (for example, interstitial fibrosis), which in patients with renal transplants should be differentiated from changes due to chronic rejection. The drug Ecoral® can also cause a dose-dependent, reversible increase in bilirubin concentration and rarely an increase in the activity of liver transaminases. During clinical practice, reports of cyclosporine hepatotoxicity were received, which was manifested by the development of cholestasis, hepatic jaundice and liver failure. In most cases, the patients’ condition was aggravated by concomitant diseases and other aggravating factors (infectious complications and simultaneous use of drugs with hepatotoxic effects). In these cases, careful monitoring of renal and liver function parameters is required. If these indicators deviate from the norm, a reduction in the dose of cyclosporine may be necessary.
In elderly patients, renal function should be especially carefully monitored.
When using the drug Ecoral® in patients after transplantation, it is necessary to determine the concentration of cyclosporine in the blood plasma.
To monitor cyclosporine blood concentrations, it is preferable to use specific monoclonal antibodies (measurement of the amount of unchanged drug). High-performance liquid chromatography can be used, which also measures the concentration of unchanged substance. If plasma or serum is used, standard separation techniques (time and temperature) should be followed. For initial determination of cyclosporine concentrations in patients with liver transplants, specific monoclonal antibodies should be used. It is also possible to conduct parallel determinations using specific and nonspecific monoclonal antibodies to achieve a dose that provides adequate immunosuppression.
It should be remembered that the concentration of cyclosporine in the blood plasma or serum is only one of many factors characterizing the patient’s clinical condition. The results of determining the concentration of cyclosporine are only one of the factors determining the dosage regimen and are considered in conjunction with various clinical and laboratory indicators.
During treatment with Ecoral®, blood pressure must be regularly monitored. If blood pressure increases, adequate antihypertensive therapy should be used. Preference should be given to antihypertensive drugs that do not affect the pharmacokinetics of cyclosporine.
Since in rare cases the drug Ecoral® causes minor reversible hyperlipidemia, it is recommended to determine the concentration of lipids in the blood plasma before treatment and one month after the start of therapy. If lipid concentrations increase, you should consider limiting dietary fat intake and, if necessary, reducing the dose of Ecoral®. The use of Ecoral® may increase the risk of hyperkalemia, especially in patients with impaired renal function. Caution should also be exercised when simultaneous use of cyclosporine with potassium-sparing diuretics, ACE inhibitors, angiotensin II receptor antagonists and potassium-containing drugs, as well as in cases of using a potassium-enriched diet. In these cases, monitoring the concentration of potassium in the blood plasma is recommended.
Cyclosporine increases the excretion of magnesium from the body, which can lead to clinically significant hypomagnesemia, especially in the peritransplantation period. In this regard, in the peritransplantation period it is recommended to monitor the concentration of magnesium in the blood plasma, especially when neurological symptoms appear. If necessary, use magnesium supplements. It is recommended to monitor serum uric acid concentrations, especially in patients with pre-existing hyperuricemia.
To prevent anaphylactoid reactions, you can administer antihistamines (H1-histamine receptor blocker) before using Ecoral®.
Additional precautions for non-transplant indications
Cyclosporine should not be used in patients with impaired renal function (with the exception of patients with nephrotic syndrome and an acceptable degree of these disorders), uncontrolled arterial hypertension, infectious diseases that cannot be adequately treated, malignant neoplasms.
Since the drug Ecoral® can cause renal dysfunction, a reliable initial concentration of creatinine in the blood serum should be established in at least 2 measurements prior to treatment. Creatinine concentrations should be monitored at 2-week intervals during the first 3 months of therapy and monthly thereafter. After 6 months of therapy, creatinine concentrations should be determined every 4-8 weeks depending on the stability of the underlying disease, type of concomitant therapy and concomitant diseases. More frequent monitoring is necessary when increasing the dose of Ecoral® when adding concomitant NSAID therapy or increasing their dose. Additional precautions for endogenous uveitis
If the serum creatinine concentration remains elevated by more than 30% compared to the initial concentration (before treatment with Ecoral®) in more than one dimension, a dose reduction of 25-50% is required. These recommendations should be followed even if the creatinine concentration remains within the laboratory normal range.
Experience with the use of Ecoral® in children with endogenous uveitis is limited.
Additional precautions for nephrotic syndrome
If the creatinine concentration remains elevated by more than 30% compared to the initial concentration (before treatment with Ecoral®) in more than one dimension, a dose reduction of 25-50% is required. In patients with initially impaired renal function, the initial dose should be 25 mg/kg/day. It is necessary to ensure careful monitoring of the condition of these patients.
Because of the changes in kidney function caused by nephrotic syndrome, it may be difficult to detect renal dysfunction caused by immunosuppressive drugs in some patients. This explains the fact that in some cases, structural changes in the kidneys associated with taking an immunosuppressive drug were not accompanied by an increase in creatinine concentration. Kidney biopsy is indicated for patients with steroid-dependent minimal change nephropathy who have received maintenance therapy with Ecoral® for more than 1 year. In rare cases, the appearance of malignant neoplasms, including Hodgkin’s lymphoma, has been observed in patients with nephrotic syndrome treated with immunosuppressive drugs.
Additional precautions for rheumatoid arthritis
If the creatinine concentration remains elevated by more than 30% of the initial value and in more than one dimension, then the dose should be reduced. If the creatinine concentration increases by more than 50%, then the dose must be reduced by 50%. These recommendations should be followed even if the creatinine concentration remains within the laboratory normal range. If the dose reduction does not lead to a decrease in creatinine concentration within 1 month, then treatment with Ecoral® should be discontinued.
Discontinuation of treatment is also necessary if uncontrolled arterial hypertension occurs during treatment with Ecoral®.
As with other long-term immunosuppressive treatment, the increased risk of lymphoproliferative disorders should be remembered. Particular caution should be observed when using Ecoral® in combination with methotrexate.
Additional precautions for psoriasis
If the creatinine concentration increases and remains elevated by more than 30% of the initial values and in more than one dimension, then the dose should be reduced by 25-50%. These recommendations should be followed even if creatinine concentrations continue to remain within the laboratory normal range. If dose reduction does not lead to a decrease in creatinine concentration within 1 month, treatment with Ecoral® should be discontinued.
Discontinuation of treatment is also necessary if uncontrolled arterial hypertension occurs during treatment with Ecoral®.
The use of Ecoral® in elderly patients is possible only in cases of disabling psoriasis, and careful monitoring of renal function is necessary.
Experience with the use of Ecoral® in children with psoriasis is limited.
It is known that in patients with psoriasis treated with cyclosporine, as with other conventional immunosuppressive treatments, the development of malignant neoplasms, especially of the skin, is possible. If skin lesions are not typical for psoriasis and if a malignant or precancerous disease is suspected, a biopsy should be performed before starting treatment with Ecoral®. Treatment of patients with malignant or precancerous lesions with Ecoral® is possible only after appropriate treatment of these diseases and in the absence of alternative effective therapy. Patients with psoriasis treated with cyclosporine may develop lymphoproliferative diseases. In these cases, the drug must be discontinued immediately. Patients treated with Ecoral® should not simultaneously receive ultraviolet B radiation or PUVA therapy.
Additional precautions for atopic dermatitis
If the creatinine concentration increases and remains elevated by more than 30% of baseline values in more than one dimension, then the dose should be reduced by 25-50%. These recommendations should be followed even if the creatinine concentration remains within the laboratory normal range. If dose reduction does not lead to a decrease in creatinine concentration within one month, treatment with Ecoral® should be discontinued.
Discontinuation of treatment is also necessary if uncontrolled arterial hypertension occurs during treatment with Ecoral®.
Since the experience with the use of Ecoral® in children with atopic dermatitis is currently still limited, the use of the drug in this category of patients is not recommended.
The use of Ecoral® in elderly patients is possible only in cases of a disabling course of the disease, and careful monitoring of renal function is necessary.
Benign lymphadenopathy is usually associated with sudden exacerbations of atopic dermatitis. It goes away either independently or against the background of a general improvement in the course of the disease. Lymphadenopathy that appears during treatment with cyclosporine should be regularly monitored.
Lymphadenopathy that persists despite decreased disease activity should be biopsied to rule out lymphoma.
Cases of herpes simplex in the acute period should be cured before starting treatment with Ecoral®, but the appearance of herpes simplex is not a reason to discontinue the drug if treatment has already been started, except in severe cases.
Skin infectious diseases caused by Staphylococcus aureus are not an absolute contraindication for therapy with Ecoral® but must be controlled by the use of appropriate antibacterial drugs.
Due to the potential risk of skin malignancy during treatment with Ecoral®, patients should be warned to avoid direct exposure to sunlight and ultraviolet B radiation or PUVA therapy.
Impact on the ability to drive vehicles. Wed and fur.:
Care should be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions, taking into account the possibility of developing adverse reactions from the nervous system such as confusion, disorientation, lethargy, visual impairment.
Active ingredient
Active ingredient
Cyclosporine
Composition
Composition
One ml of 10% solution contains:
Active substance: Cyclosporine 100 mg;
Excipients: Ethyl alcohol 120 mg, Polyglyceryl (3) oleate 310 mg, Polyglyceryl (10) oleate 190 mg, Macrogol glyceryl hydroxystearate 280 mg.
Pregnancy
Pregnancy
Experience with the use of cyclosporine in pregnant women is limited. Pregnant women who have undergone transplantation and are taking immunosuppressive drugs, including cyclosporine, have an increased risk of preterm birth (less than 37 weeks). There are a limited number of observations of children up to the age of 7 years whose mothers took cyclosporine during pregnancy. Renal function indicators and blood pressure in these children were within the normal range for age. However, there is no information on the effectiveness and safety of cyclosporine in pregnant women; therefore, cyclosporine should not be used during pregnancy unless the expected benefit to the mother outweighs the potential risk to the fetus.
Cyclosporine passes into breast milk. Breastfeeding should be discontinued if cyclosporine use is necessary.
Contraindications
Contraindications
hypersensitivity to the components of the drug
malignant neoplasms and precancerous skin diseases
chicken pox
Herpes Zoster (risk of generalization of the process)
severe liver failure
hyperkalemia
uncontrolled hypertension
malabsorption syndrome
infectious diseases in the acute phase.
Side Effects
Side Effects
Many side effects associated with the use of cyclosporine are dose-dependent and reversible with dose reduction. The spectrum of side effects is generally the same when used for different indications; however, the frequency and severity of side effects may vary. In transplant patients, due to the use of higher doses and longer duration of treatment, side effects are more common and usually more severe than in patients taking cyclosporine for non-transplant indications.
In patients receiving immunosuppressive treatment with cyclosporine or combination therapy including cyclosporine, the risk of developing local and generalized infections (viral bacterial fungal etiology) and parasitic infestations increases. It is also possible to exacerbate pre-existing infectious diseases and reactivate polyomavirus infection leading to the development of polyomavirus-associated nephropathy (PVAN) (especially associated with the BK virus) or progressive multifocal leukoencephalopathy (PMLEP) (associated with the JC virus). The development of severe infectious diseases has been reported in some cases with fatal outcome.
In patients receiving immunosuppressive treatment with cyclosporine or combination therapy including cyclosporine, the risk of developing lymphomas, lymphoproliferative diseases and solid malignancies, especially of the skin, increases. The incidence of malignant neoplasms increases with increasing intensity and duration of immunosuppressive therapy.
The incidence of side effects is classified in accordance with the recommendations of the World Health Organization: very often – at least 10%; often – not less than 1% but less than 10%; infrequently – not less than 01% but less than 1%; rarely – not less than 001% but less than 01%; very rarely – 001% including individual messages.
Infections: often – upper respiratory tract infection, lower respiratory tract infection including bronchiolitis, urinary tract infection, cytomegalovirus infection; infrequently – sepsis, herpetic infection, candidiasis infection.
Neoplasms: rarely – skin papilloma, basal cell carcinoma, squamous cell skin cancer, Bowen’s disease, lymphoproliferative diseases, including lymphoma; very rarely – seborrheic keratosis melanoma.
From the blood and lymphatic system: infrequently – anemia, thrombocytopenia; rarely – microangiopathic anemia, hemolytic uremic syndrome.
From the nervous system: very often – tremor, headache, including migraine; often – paresthesia; uncommon – encephalopathy convulsions confusion disorientation retardation psychomotor agitation sleep disturbance visual impairment cortical blindness coma paresis cerebellar ataxia; rarely – motor polyneuropathy; very rarely – papilledema, including papilledema secondary to benign intracranial hypertension.
From the cardiovascular system: very often – increased blood pressure (BP).
From the digestive system: often – anorexia nausea vomiting abdominal pain diarrhea gum hyperplasia; infrequently – impaired liver function (increased activity of liver transaminases and bilirubin concentration in the blood serum); rarely – pancreatitis.
From the skin and subcutaneous tissue: often – hypertrichosis; uncommon – allergic skin rash.
From the musculoskeletal and connective tissue side: often – muscle spasms, myalgia; rarely – muscle weakness myopathy.
From the urinary system: very often – impaired renal function.
From the genitourinary system: rarely – dysmenorrhea, gynecomastia.
Laboratory indicators: very often – hyperlipidemia; often – hypercholesterolemia, hyperuricemia, hyperkalemia, hypomagnesemia; rarely – hyperglycemia.
Other: often – fatigue; infrequently – weight gain, edema.
Interaction
Interaction
Listed below are drugs for which interaction with cyclosporine is confirmed and clinically significant.
Various drugs can increase or decrease the concentrations of cyclosporine in plasma or whole blood, usually due to the inhibition or induction of enzymes involved in the metabolism of cyclosporine, in particular the CYP3A4 isoenzyme of the cytochrome P450 system. Since cyclosporine is an inhibitor of the CYP3A4 isoenzyme and the membrane transporter of P-glycoprotein molecules, when used simultaneously with cyclosporine, it is possible to increase the concentration of drugs that are substrates of the CYP3A4 isoenzyme and/or the membrane transporter of P-glycoprotein.
Drugs that reduce the concentration of cyclosporine in the blood plasma by inhibiting the CYP3A4 isoenzyme
Barbiturates carbamazepine oxcarbazepine phenytoin nafcillin sulfadimidine for intravenous administration rifampicin octreotide probucol orlistat preparations containing St. John’s wort (Hypericum perforatum) ticlopidine sulfinpyrazone terbinafine bosentan.
Drugs that increase the concentration of cyclosporine in the blood plasma by inhibiting the CYP3A4 isoenzyme
Macrolide antibiotics (mainly erythromycin azithromycin and clarithromycin) ketoconazole fluconazole itraconazole voriconazole diltiazem nicardipine verapamil metoclopramide oral contraceptives danazol methylprednisolone (high doses) allopurinol amiodarone cholic acid and its derivatives HIV protease inhibitors imatinib colchicine nefazodone.
Other drug interactions
Caution should be exercised when used simultaneously with drugs that increase the risk of nephrotoxicity, including aminoglycosides (gentamicin tobramycin), amphotericin B, ciprofloxacin, vancomycin, trimethoprim (+ sulfamethoxazole), nonsteroidal anti-inflammatory drugs (NSAIDs) (diclofenac, naproxen sulindac), melphalan H2- histamine receptor blockers (cimetidine ranitidine) methotrexate.
Concomitant use with tacrolimus should be avoided due to an increased risk of nephrotoxicity.
In case of simultaneous use with drugs that have nephrotoxic effects, it is necessary to carefully monitor kidney function indicators (in particular, regularly determine the concentration of creatinine in the blood serum). If significant renal impairment is detected, the dose of this drug should be reduced or alternative treatment considered.
There are isolated reports of the development of significant but reversible renal dysfunction (with a corresponding increase in creatinine concentration) in transplant patients with simultaneous use of cyclosporine with fibric acid derivatives (for example, bezafibrate, fenofibrate). Therefore, it is necessary to monitor renal function in this category of patients. If severe renal dysfunction develops, the simultaneous use of the above drugs should be discontinued.
Concomitant use with nifedipine may lead to more pronounced gingival hyperplasia than with cyclosporine monotherapy. In patients with gingival hyperplasia during treatment with cyclosporine, concomitant use of nifedipine should be avoided.
When used simultaneously with lercanidipine, there is an increase in the area under the concentration-time curve (AUC) of lercanidipine by 3 times and the AUC of cyclosporine by 21%. Caution should be exercised when used concomitantly with lercanidipine.
Cyclosporine is a highly active P-glycoprotein inhibitor and may increase plasma concentrations of drugs that are P-glycoprotein substrates such as aliskiren. After simultaneous use of cyclosporine and aliskiren, the maximum concentration of aliskiren increases approximately 25 times and the AUC increases by 5 times. However, the pharmacokinetic profile of cyclosporine does not change significantly. It has been found that simultaneous use with diclofenac can significantly increase the bioavailability of diclofenac with the possible development of reversible renal dysfunction. The increase in the bioavailability of diclofenac is most likely due to a decrease in its metabolism during the “first pass” through the liver. When used simultaneously with NSAIDs with a less pronounced first-pass effect (for example, acetylsalicylic acid), an increase in their bioavailability is not expected. NSAIDs with a pronounced first-pass effect through the liver (including diclofenac) should be used in lower doses than in patients not receiving cyclosporine.
Cyclosporine may reduce the clearance of digoxin, colchicine, prednisolone, HMG-CoA reductase inhibitors (statins), and etoposide. Several cases of severe glycoside toxicity have been reported within a few days of starting cyclosporine treatment in patients receiving digoxin. There are also reports that cyclosporine may enhance the toxic effects of colchicine, including the development of myopathy or neuropathy, especially in patients with impaired renal function. When cyclosporine is used concomitantly with digoxin or colchicine, careful clinical monitoring is necessary to promptly identify the toxic effects of these drugs and to decide whether to reduce the dose or discontinue treatment.
The literature describes cases of muscle toxicity including muscle pain, weakness, myositis and rhabdomyolysis with simultaneous use of cyclosporine with lovastatin, simvastatin, atorvastatin, pravastatin, and in rare cases with fluvastatin, which were observed in the post-marketing period. If it is necessary to use the above drugs simultaneously with cyclosporine, it is necessary to reduce their dose. Statin therapy should be temporarily discontinued or discontinued in patients with symptoms of myopathy and in patients with predisposition factors for severe renal impairment, including renal failure secondary to rhabdomyolysis.
An increase in creatinine concentrations was observed in clinical studies in which the simultaneous use of everolimus or sirolimus with high doses of cyclosporine in the form of a microemulsion was studied. This effect is often reversible after reducing the dose of cyclosporine. Everolimus and sirolimus have little effect on the pharmacokinetic parameters of cyclosporine. The simultaneous use of cyclosporine with everolimus or sirolimus leads to a significant increase in the concentration of the latter in the blood plasma. Caution should be exercised when using cyclosporine together with potassium-sparing drugs (potassium-sparing diuretics, angiotensin converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists) or potassium drugs to prevent the possible development of severe hyperkalemia. Cyclosporine may increase repaglinide concentrations and increase the risk of hypoglycemia.
In transplant patients with simultaneous use of drugs that reduce or increase the bioavailability of cyclosporine, the concentration of cyclosporine should be regularly determined and, if necessary, the dose of cyclosporine should be adjusted, especially at the initial stage of combination treatment or during its withdrawal.
In patients without a transplant, monitoring cyclosporine concentrations is not as significant because for these patients the relationship between plasma concentrations and clinical effects has not been clearly proven. When cyclosporine is used concomitantly with drugs that increase its concentration, frequent monitoring of renal function and monitoring for side effects of cyclosporine are more important than determining the plasma concentration of cyclosporine.
Food interaction
The use of cyclosporine while drinking grapefruit juice and fatty foods may be accompanied by an increase in its bioavailability.
Vaccinations should not be administered during treatment with cyclosporine as the effectiveness of live attenuated vaccines may be reduced.
Overdose
Overdose
There are no data on acute overdose with the drug to date and there is limited experience with overdose with other cyclosporines.
Symptoms: renal dysfunction that is probably reversible and will disappear when the drug is discontinued.
Treatment: according to indications, general supportive measures should be carried out. The drug can be eliminated from the body only through nonspecific measures, including gastric lavage, since cyclosporine is practically not eliminated during hemodialysis and hemoperfusion using activated charcoal.
Storage conditions
Storage conditions
Keep out of the reach of children.
Store at temperatures between 20°C and 25°C in a dry place protected from light.
At temperatures below 20°C, the solution may have a gel-like consistency and a sediment may appear, which disappears when the temperature rises to 20°C.
However, minor amounts of flakes or light sedimentation may remain. These phenomena do not affect the effectiveness and safety of the drug and dosing using a measuring syringe remains accurate.
Shelf life
Shelf life
2 years. Do not use a drug that has expired.
The solution must be used within 3 months after opening the package.
Manufacturer
Manufacturer
Teva Czech Enterprises s.r.o., Czech Republic
Additional information
| Shelf life | 2 years. Do not use the drug with an expired shelf life. The solution must be used within 3 months after opening the package. |
|---|---|
| Conditions of storage | Keep out of reach of children. Store at 20°C to 25°C in a dry place protected from light. At temperatures below 20°C the solution may have a gel-like consistency and there may be a residue which disappears when the temperature is raised to 20°C. |
| Manufacturer | Teva Czech Enterprises s.r.o., Czech Republic |
| Medication form | oral solution |
| Brand | Teva Czech Enterprises s.r.o. |
Related products
Buy Ecoral, 100 mg/ml 50 ml with delivery to USA, UK, Europe and over 120 other countries.