No products in the cart.
Dufaston, 10 mg 112 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group
Sex hormones. Progestagens. Pregnadine derivatives. Dydrogesterone.
ATC code G03DB01
Pharmacological properties
Pharmacokinetics
Absorption. After oral administration, didrogesterone is rapidly absorbed from the gastrointestinal tract. Time of reaching maximum concentration (Tmax) is from 0.5 to 2.5 hours. The absolute bioavailability of didrogesterone at a dose of 20 mg orally (compared with 7.8 mg intravenously) is 28%.
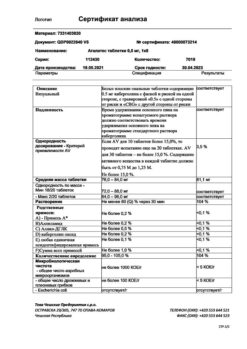
The table shows the mean pharmacokinetic parameters of didrogesterone (D) and dihydrodihydrogesterone (DDH) after multiple oral doses of 10 mg of didrogesterone.
Didrogesterone 10 mg
D | DDD | |
Cmax(ng/mL) | 2.1 | 53.0 |
AUCinf (ng*h/mL) | 7.7 | 322.0 |
*: based on AUC (0-tau)/24
Distribution. With a stable concentration of didrogesterone when administered intravenously, the volume of distribution is about 1400L. Didrogesterone and DDH bind to plasma proteins by more than 90%.
Metabolism. After oral administration, didrogesterone is rapidly metabolized to DDH. The concentration of the main metabolite 20-α-dihydrodihydrogesterone (DDH) peaks about 1.5 hours after a dose. Plasma concentrations of DDH are significantly higher than those of didrogesterone. The AUC (area under the curve) and Cmax (maximum concentration) ratios of DDH and didrogesterone are approximately 40 and 25, respectively. The half-lives of didrogesterone and DDH are on average 5-7 hours and 14-17 hours, respectively. The main feature of all didrogesterone metabolites is the presence of the 4,6-dien-3-1 configuration of the parent compound and the absence of 17-α-hydroxylation. This explains the absence of estrogenic and androgenic effects of didrogesterone.
Excretion. After oral administration of labeled didrogesterone, on average 63% of the dose is excreted with the urine. Total plasma clearance is 6.4 l/min. Complete excretion of didrogesterone occurs after 72 hours. DDH is excreted with urine mainly in the form of glucuronic acid conjugate.
Dose and time dependence. Pharmacokinetics are linear for both single and multiple doses between 2.5 and 10 mg. A comparison of the kinetics of single and multiple doses shows that the pharmacokinetic parameters of D and DD do not change as a result of repeated dosing. Stable concentration is reached after 3 days of treatment.
Pharmacodynamics
Dydrogesterone is a synthesized analogue of progesterone that is active when taken orally. Dufaston® causes complete endometrial secretory transformation in the estrogen-sensitized uterus, thereby protecting the endometrium from hyperplasia and/or cancer, the risk of which is increased with estrogen intake. Dydrogesterone has no estrogenic, androgenic, anabolic or corticoid activity.
Dufaston® does not suppress ovulation. As a consequence, it remains possible to conceive in women of reproductive age who take Dufaston®.
In postmenopausal women with a non-removed uterus, estrogen-based ZGT increases the risk of endometrial hyperplasia and cancer. The addition of progestagen prevents an increase in this risk.
Indications
Indications
– menstrual irregularities
– endometriosis
– dysmenorrhea
– infertility due to luteal insufficiency
– threatened abortion due to progesterone deficiency
– recurrent miscarriage due to progesterone deficiency
– premenstrual syndrome
During estrogen therapy in women with an intact uterus, it can be used in a cyclic mode for the following conditions:
– to prevent endometrial hyperplasia during postmenopause
– dysfunctional uterine bleeding
– secondary amenorrhea
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Sex hormones. Progestogens. Pregnadiene derivatives. Dydrogesterone.
ATX code G03DB01
Pharmacological properties
Pharmacokinetics
Absorption. After oral administration, dydrogesterone is rapidly absorbed from the gastrointestinal tract. Time to reach maximum concentration (Tmax) from 0.5 to 2.5 hours. The absolute bioavailability of dydrogesterone at a dose of 20 mg orally (compared with 7.8 mg intravenously) is 28%.
The table shows the average values of the pharmacokinetic parameters of dydrogesterone (D) and dihydrodydrogesterone (DHD) after repeated oral administration of dydrogesterone at a dose of 10 mg.
Dydrogesterone 10 mg
D
DGD
Cmax(ng/ml)
2.1
53.0
AUCinf (ng*h/ml)
7.7
322.0
*: based on AUC (0-tau)/24
Distribution. At a stable concentration of dydrogesterone when administered intravenously, the volume of distribution is about 1400 l. Dydrogesterone and DHD are more than 90% bound to plasma proteins.
Metabolism. After oral administration, dydrogesterone is rapidly metabolized to DGD. Concentrations of the major metabolite 20-α-dihydrodydrogesterone (DHD) peak approximately 1.5 hours after dosing. The concentration of DHD in blood plasma is significantly higher than that of dydrogesterone. The AUC (area under the curve) and Cmax (maximum concentration) ratios of DHD and dydrogesterone are approximately 40 and 25, respectively. The half-lives of dydrogesterone and DHD average 5–7 hours and 14–17 hours, respectively. The main feature of all dydrogesterone metabolites is the presence of the 4,6-diene-3-1 configuration of the parent compound and the absence of 17-α-hydroxylation. This explains the lack of estrogenic and androgenic effects of dydrogesterone.
Excretion. After oral administration of labeled dydrogesterone, an average of 63% of the dose is excreted in the urine. Total plasma clearance 6.4 l/min. Complete elimination of dydrogesterone occurs after 72 hours. DHD is excreted in urine primarily in the form of a glucuronic acid conjugate.
Dependence on dose and time. Pharmacokinetics are linear for both single and multiple dosing in the range from 2.5 to 10 mg. A comparison of the kinetics of single and multiple doses shows that the pharmacokinetic parameters of D and DHD do not change as a result of repeated dosing. Stable concentrations are achieved after 3 days of treatment.
Pharmacodynamics
Dydrogesterone is a synthesized analogue of progesterone that is active when taken orally. Duphaston® causes complete secretory transformation of the endometrium in the estrogen-sensitized uterus, thereby protecting the endometrium from hyperplasia and/or cancer, the risk of which increases when taking estrogens. Dydrogesterone does not have estrogenic, androgenic, anabolic or corticoid activity.
Duphaston® does not suppress ovulation. As a result, the possibility of conception remains possible in women of reproductive age taking Duphaston®.
In postmenopausal women with a non-removed uterus, HRT with estrogens increases the risk of endometrial hyperplasia and cancer. The addition of a progestogen prevents this risk from increasing.
Special instructions
Special instructions
Before starting to take Duphaston for the treatment of uterine bleeding, it is necessary to exclude the organic cause of its occurrence.
Sometimes breakthrough bleeding may occur during the first months of treatment. If breakthrough bleeding or spotting occurs after a certain period of taking the drug or continues after a course of treatment, their cause should be determined and an endometrial biopsy performed to exclude malignant changes in the endometrium.
Conditions requiring discontinuation of treatment
If one of the following conditions appears in the first days of treatment or if their severity increases, discontinuation of therapy should be considered:
– exceptionally severe headache, migraine or symptoms suggestive of cerebral ischemia
– significant increase in blood pressure
– signs of venous thromboembolism.
In case of threatened abortion or recurrent miscarriage, the progression of pregnancy and the viability of the embryo or fetus should be monitored.
Conditions requiring close monitoring
It is known that some rare conditions may be sex hormone dependent and may occur or worsen during pregnancy and use of drugs containing sex hormones. Among them: cholestatic jaundice, herpes of pregnancy, severe itching, otosclerosis and porphyria.
Patients with a history of depression require careful monitoring. If signs of depression occur, Duphaston should be discontinued.
Other states
The drug contains lactose monohydrate. Patients with rare hereditary diseases of galactose intolerance, lactase deficiency (Lappa) or glucose-galactose malabsorption syndrome should not take Duphaston®.
If Duphaston is prescribed in combination with estrogens (for example, for HRT), you should carefully read the contraindications and warnings associated with the use of estrogens.
Special instructions when using Duphaston to prevent endometrial hyperplasia during the postmenopausal period
Safety information for products containing estrogen should be considered.
For the treatment of menopausal symptoms, Duphaston® is used as hormone replacement therapy (HRT) only when menopausal symptoms significantly worsen a woman’s quality of life. Periodically, at least once a year, it is necessary to evaluate the risks and benefits of HRT and continue treatment when the benefits outweigh the risks.
Medical examination and observation. A complete medical and family history should be obtained before starting or resuming HRT. A medical examination (including examination of the mammary glands and pelvic organs) is carried out to identify possible contraindications and conditions requiring precautions. During treatment with Duphaston®, dynamic monitoring is recommended (the frequency and nature of studies are determined individually). Patients should know that they should immediately report any changes in the mammary glands to their doctor. Regular breast examination, including mammography, is carried out in accordance with accepted screening standards, taking into account clinical indications.
Endometrial hyperplasia. The risk of endometrial hyperplasia and cancer increases with long-term estrogen use in women with a non-removed uterus. Depending on the duration of treatment and dose of estrogen, the risk may be 2 to 12 times higher compared to women not taking estrogen. After stopping estrogen use, the risk may remain for at least 10 years. This excess risk can be prevented by adding progestogens for at least 12 consecutive days within a 28-day cycle/month.
Breakthrough bleeding may occur during the first months of treatment. If breakthrough bleeding occurs a significant time after the start of treatment or after its cessation, it is necessary to examine the woman, including performing an endometrial biopsy, to exclude malignancy.
Breast cancer
According to current data from clinical and epidemiological studies, women taking combined estrogen-progestogen drugs and possibly monoestrogens for HRT have an increased risk of breast cancer (BC), and this depends on the duration of treatment.
The randomized, placebo-controlled WHI (Women’s Health Initiative study) study, as well as epidemiological studies, confirm an increased risk of breast cancer in women taking estrogens in combination with progestogens for HRT, which becomes significant after 3 years of treatment. After stopping treatment, the risk remains elevated for a maximum of 5 years. With HRT, especially combined drugs, the density of the mammographic image increases, which can adversely affect the results of radiological diagnosis of breast cancer.
Ovarian cancer
Ovarian cancer is much less common than breast cancer. Epidemiological data from a large meta-analysis have shown a slightly increased risk in women using estrogen alone or estrogen plus progestogen for HRT, which occurs within 5 years of use and decreases with time after discontinuation of use. Several other studies, including the WHI, suggest that combination HRT may be associated with the same or slightly lower risk.
Venous thromboembolism. HRT is associated with an increase in the relative risk of developing venous thromboembolism (VTE), that is, deep vein thrombosis and pulmonary thromboembolism, by 1.3-3 times. The likelihood of such a complication is higher in the first year of treatment than in a later period.
Patients with a history of VTE or diagnosed thrombophilic conditions have an increased risk of VTE, and HRT may increase this risk. Therefore, HRT is contraindicated in this group of patients.
Typically, risk factors for VTE include the use of estrogens, older age, major surgery, prolonged immobilization, severe obesity (BMI more than 30 kg/m2), pregnancy and the postpartum period, systemic lupus erythematosus and diagnosed malignant neoplasms. Currently, there is no consensus on the relationship between varicose veins and VTE risk factors.
It is necessary to take preventive measures to prevent VTE in patients in the postoperative period. When long-term immobilization is expected after surgery, especially on abdominal or orthopedic surgery of the lower extremities, HRT should be stopped, if possible, 4-6 weeks before surgery. Resumption of treatment is possible only after the woman has fully recovered her motor ability.
Patients with no history of VTE, but who have a first-degree relative with a history of thrombosis at a young age, may be offered screening for congenital coagulation factor defects after careful routine evaluation (screening can only detect a certain range of thrombophilic abnormalities). If a thrombophilic defect is identified that causes cases of thrombosis in family members, or if the identified defect is serious (such as antithrombin, protein S or protein C deficiency or a combination of these defects), HRT is contraindicated.
Patients taking anticoagulants need to carefully re-evaluate the risk-benefit ratio of HRT.
If VTE develops during HRT, treatment should be stopped. The patient should know that when the first possible symptoms of VTE appear (painful swelling of the lower extremities, sudden chest pain, shortness of breath), she should immediately contact her doctor.
Coronary heart disease. Randomized clinical trials did not show that women with or without coronary artery disease who took HRT drugs, combined or monoestrogens, were protected from myocardial infarction.
The relative risk of coronary heart disease when using combination drugs with HRT is slightly increased. Since the initial absolute risk of CHD is very dependent on age, the number of additional cases of CHD with combined HRT among healthy women with short menopausal experience is very small, but increases with age.
Ischemic stroke. Combined and monoestrogenic HRT is accompanied by an increase in the risk of ischemic stroke up to 1.5 times. The relative risk does not change with age or menopause. However, the baseline risk of ischemic stroke is highly dependent on age, and the overall risk of stroke in women taking HRT increases with age.
Pregnancy and lactation. It is estimated that about 9 million women took Duphaston during pregnancy. To date, there is no indication that the use of Duphaston during pregnancy has harmful effects. The scientific literature describes a study that found that the use of certain progestogens is accompanied by an increased risk of hypospadias. However, since this fact has not been confirmed in other studies, a final conclusion cannot be made about the effect of progestogens on the occurrence of hypospadias.
Clinical studies in which a limited number of women took dydrogesterone in early pregnancy did not show an increased risk of hypospadias. There are no other epidemiological data available at this time. The effects observed in non-clinical studies on embryo-fetal or postnatal development are consistent with the pharmacological profile. Undesirable effects occurred only at doses that significantly exceeded the maximum human exposure dose.
Duphaston can be prescribed during pregnancy if there are clear indications.
It is not known whether dydrogesterone is excreted in breast milk. No special studies have been conducted to detect dydrogesterone in mother’s milk. Experience from studies with other progestogens shows that progestogens and their metabolites are found in small quantities in breast milk. The risk to a nursing infant is unknown. Therefore, taking Duphaston during breastfeeding is not recommended.
There are no data on the effect of dydrogesterone on fertility.
Features of the effect of the drug on the ability to drive a vehicle or potentially dangerous mechanisms
Duphaston® has a slight effect on the ability to drive a car and drive potentially dangerous machinery.
In rare cases, Duphaston® may cause drowsiness and/or dizziness, especially in the first few hours after administration. Therefore, you should be careful when driving a car or operating machinery.
Active ingredient
Active ingredient
Dydrogesterone
Composition
Composition
1 film-coated tablet contains:
Active ingredient: dydrogesterone – 10.0 mg;
Excipients: lactose monohydrate – 111.1 mg, hypromellose – 2.8 mg, corn starch – 14 mg, colloidal silicon dioxide – 1.4 mg, magnesium stearate – 0.7 mg.
Shell composition: opadry white Y-1-7000 (hypromellose, polyethylene glycol 400, titanium dioxide (E171)) – 4 mg.
Contraindications
Contraindications
– contraindications for estrogens should be taken into account when they are used in combination with progestogens such as dydrogesterone
– vaginal bleeding of unknown etiology
– serious liver dysfunction at the moment or in history before normalization of liver tests
– hypersensitivity to dydrogesterone or other components of the drug
– diagnosed or suspected progestogen- or estrogen-dependent malignant neoplasms (for example, meningioma).
Side Effects
Side Effects
The most commonly reported adverse reactions during clinical trials in patients using dydrogesterone for non-estrogen indications were metrorrhagia, breast tenderness/tenderness, and migraine/headache.
The following adverse reactions (and their frequency) were observed during clinical trials with dydrogesterone (n=3483) for non-estrogen indications and were spontaneously reported.
– very often (≥ 1/10);
– often (from ≥ 1/100 to <1/10);
– uncommon (from ≥ 1/1000 to < 1/100);
– rare (from ≥ 1/10000 to < 1/1000)
Benign, malignant and unspecified neoplasms (including cysts and polyps): rarely – an increase in the size of progestogen-dependent neoplasms (for example, meningioma)*.
Disorders of the blood and lymphatic system: rarely – hemolytic anemia*.
Immune system disorders: rarely – hypersensitivity.
Mental disorders: infrequently – depression.
Nervous system disorders: often – migraine/headache; infrequently – dizziness; rarely – drowsiness.
Disorders of the hematopoietic and lymphatic systems – hypersensitivity.
Gastrointestinal disorders: often – nausea; infrequently – vomiting.
Disorders of the liver and biliary tract: infrequently – impaired liver function (with jaundice, asthenia or malaise, abdominal pain).
Skin and subcutaneous tissue disorders: uncommon – allergic dermatitis (for example, rash, itching, urticaria); rarely – angioedema*.
Genital and breast disorders: often – menstrual disorders (including metrorrhagia, menorrhagia, oligo/amenorrhea, dysmenorrhea and irregular menstruation). Breast tenderness/sensitivity; rarely – swelling of the mammary glands.
General disorders and disorders at the injection site: rarely – swelling.
Impact on the results of laboratory and instrumental studies: infrequently – increase in body weight.
* Adverse reactions from spontaneous reports that were not observed in clinical trials were classified as “rare” based on the fact that the upper limit of the 95% confidence interval of the incidence rate was less than 3/x, where x = 3483 (total number of subjects in clinical trials).
Undesirable side reactions that may occur during estrogen-progestagen therapy (see also the “Special Instructions” section, as well as information in the instructions for medical use of estrogen):
• breast cancer, endometrial hyperplasia, endometrial cancer, ovarian cancer;
• venous thromboembolism;
• myocardial infarction, coronary heart disease, ischemic stroke.
Interaction
Interaction
Data from in vitro studies indicate that the major metabolic pathway results in the formation of the major pharmacologically active metabolite, 20-alpha-dihydrodydrogesterone (DHD), which is catalyzed by aldoketo reductase 1C (AKR 1C) in the human cytosol. The following metabolic transformation is carried out by isoenzymes of the cytochrome P450 system (CYPs), almost exclusively by the CYP3A4 isoenzyme, leading to the formation of various minor metabolites. The main active metabolite of DHD is a substrate for metabolic transformation by the CYP3A4 isoenzyme. Therefore, the metabolism of dydrogesterone and DHD can be increased with the simultaneous use of drugs that increase the synthesis of enzymes of the cytochrome system, for example, anticonvulsants (for example, phenobarbital, phenytoin, carbamazepine), some tuberculostatics and antivirals (for example, rifampicin, rifabutin, nevirapine, efavirenz), as well as herbal preparations containing extracts of the herb St. John’s wort (Hypericum perforatum), sage or ginkgo biloba.
Ritonavir and nelfinavir, known as potent inhibitors of cytochrome enzymes, on the contrary, exhibit the properties of enzyme inducers when taken simultaneously with steroids.
The clinical significance of increased dydrogesterone metabolism is the reduction in efficacy.
In vitro studies have shown that dydrogesterone and DHD at therapeutic concentrations do not suppress or induce cytochrome enzymes.
Overdose
Overdose
Symptoms: There is limited data regarding overdose in humans. Duphaston is well tolerated when administered orally (the maximum daily dose taken by a person is 360 mg).
Treatment: There is no specific antidote; treatment should be symptomatic. This information also applies to overdose in children.
Storage conditions
Storage conditions
Store at a temperature not exceeding 30 0C.
Keep out of the reach of children!
Shelf life
Shelf life
5 years
Do not use after the date indicated on the package.
Manufacturer
Manufacturer
Veropharm LLC, Russia
Additional information
| Shelf life | 5 years Do not use later than the date on the package. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 30°C. Store out of the reach of children! |
| Manufacturer | Veropharm AO, Russia |
| Medication form | pills |
| Brand | Veropharm AO |
Related products
Buy Dufaston, 10 mg 112 pcs with delivery to USA, UK, Europe and over 120 other countries.