No products in the cart.
Diprometa, 7 mg/ml suspension 1 ml
€21528.00 €17.94
Description
Pharmacotherapeutic group: Glucocorticosteroid (GCS)
ATX code: H02AB01
Pharmacological properties
Pharmacodynamics
p> Betamethasone is a synthetic GCS with high glucocorticosteroid and minor mineralocorticoid activity. Betamethasone has anti-inflammatory, anti-allergic and immunosuppressive effects, and also has a pronounced and diverse effect on various types of metabolism.
It interacts with specific cytoplasmic receptors to form a complex which penetrates the cell nucleus and stimulates synthesis of matrix ribonucleic acid, the latter induces formation of proteins, including lipocortin, which mediate cellular effects. Lipokortin inhibits phospholipase A2, suppresses the release of arachidonic acid and inhibits the synthesis of endoperoxides, prostaglandins, leukotrienes that contribute to the processes of inflammation, allergy, etc. Protein metabolism: reduces the amount of protein in the blood plasma (at the expense of globulins) with increased albumin/globulin ratio, increases the synthesis of albumin in the liver and kidneys, increases protein catabolism in muscle tissue.
Lipid metabolism: increases the synthesis of higher fatty acids and triglycerides, redistributes fat (fat accumulation mainly in the shoulder girdle, face, abdomen), leads to hypercholesterolemia.
Carbohydrate metabolism: increases absorption of carbohydrates from the gastrointestinal tract (GIT), increases the activity of glucose-6-phosphatase, leading to increased glucose flow from the liver into the blood, increases the activity of phosphoenolpyruvate carboxylase and aminotransferase synthesis, leading to activation of gluconeogenesis.
Water-electrolyte metabolism: it retains sodium ions and water in the body, stimulates the excretion of potassium ions (mineralocorticoid activity), reduces absorption of calcium from the GI tract, “washes” calcium ions from the bones and increases their excretion by the kidneys.
The anti-inflammatory action is associated with inhibition of release of inflammatory mediators by eosinophils, induction of lipocortin formation and reduction of the number of mast cells producing hyaluronic acid, reduction of capillary permeability, stabilization of cell membranes and organelle membranes (especially lysosomal).
The anti-allergic effect results from suppression of synthesis and secretion of allergy mediators, inhibition of release of histamine and other bioactive substances from sensitized mast cells and basophils, inhibition of maturation and differentiation of T- and B-lymphocytes and mast cells, decrease of sensitivity of effector cells to allergy mediators, suppression of antibody formation, changes in immune response.
It increases sensitivity of beta-adrenoreceptors of small and medium caliber bronchi to endogenous catecholamines and exogenous sympathomimetics, decreases viscosity of bronchial mucosal secretion due to suppression or reduction of its production.
The immunosuppressive action is caused by inhibition of cytokine release (interleukin-1, interleukin-2, gamma-interferon) from lymphocytes and macrophages. It suppresses the synthesis and secretion of ACTH and secondary to the synthesis of endogenous GCS.
Inhibits secretion of thyroid hormone (TSH) and follicle stimulating hormone (FSH).
Suppresses the release of beta-lipotropin, but does not decrease circulating beta-endorphin.
Inhibits connective tissue reactions during the inflammatory process and reduces the possibility of scar tissue formation.
Betamethasone sodium phosphate is a readily soluble compound that is well absorbed after parenteral administration into the tissues and provides a rapid effect. Betamethasone dipropionate has slower absorption. Combining these betamethasone salts can create a drug with both short-term (but fast) and long-term action. Depending on the route of administration (intramuscular (I/M), intraarticular, periarticular, intradermal (I/D)) a general or local effect is achieved.
Pharmacokinetics
Betamethasone sodium phosphate is highly soluble in water and after intramuscular administration is rapidly hydrolyzed and almost immediately absorbed from the injection site, allowing rapid onset of therapeutic action. It is almost completely eliminated within one day after administration.
Betamethasone dipropionate is slowly absorbed from the depot, is metabolized gradually, which leads to the long-term action of the drug, and is eliminated within more than 10 days.
Betamethasone binds well to plasma proteins (62.5%). It is metabolized in the liver to form mostly inactive metabolites. It is excreted mainly by the kidneys.
Indications
Indications
Treatment of conditions and diseases in which GCS therapy can achieve the required clinical effect (it must be borne in mind that for some diseases GCS therapy is additional and does not replace standard therapy):
Diseases of the musculoskeletal system and soft tissues, incl. rheumatoid arthritis, osteoarthritis, bursitis, ankylosing spondylitis, epicondylitis, coccydynia, torticollis, ganglion cyst, fasciitis.
Allergic diseases, incl. bronchial asthma, hay fever (hay fever), allergic bronchitis, seasonal or year-round rhinitis, drug allergies, serum sickness, reactions to insect bites.
Dermatological diseases, incl. atopic dermatitis, coin-shaped eczema, neurodermatitis, contact dermatitis, severe photodermatitis, urticaria, lichen planus, alopecia areata, discoid lupus erythematosus, psoriasis, keloid scars, pemphigus vulgaris, cystic acne.
Systemic connective tissue diseases, including systemic lupus erythematosus, scleroderma, dermatomyositis, periarteritis nodosa.
Hemoblastoses (palliative therapy of leukemia and lymphomas in adults; acute leukemia in children).
Primary or secondary insufficiency of the adrenal cortex (with mandatory simultaneous use of mineralocorticoids).
Other diseases and pathological conditions requiring systemic therapy with corticosteroids (adrenogenital syndrome, regional ileitis, pathological changes in the blood if the use of corticosteroids is necessary).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Glucocorticosteroid (GCS)
ATX code: H02AB01
Pharmacological properties
Pharmacodynamics
Betamethasone is a synthetic corticosteroid with high glucocorticosteroid and low mineralocorticoid activity. Betamethasone has anti-inflammatory, antiallergic and immunosuppressive effects, and also has a pronounced and varied effect on various types of metabolism.
Interacts with specific cytoplasmic receptors to form a complex that penetrates the cell nucleus and stimulates the synthesis of matrix ribonucleic acid, the latter induces the formation of proteins, incl. lipocortin, mediating cellular effects. Lipocortin inhibits phospholipase A2, suppresses the release of arachidonic acid and suppresses the synthesis of endoperoxides, prostaglandins, leukotrienes, which contribute to inflammation, allergies, etc. Protein metabolism: reduces the amount of protein in the blood plasma (due to globulins) with an increase in the albumin/globulin ratio, increases the synthesis of albumins in the liver and kidneys, increases protein catabolism in muscle tissue.
Lipid metabolism: increases the synthesis of higher fatty acids and triglycerides, redistributes fat (accumulation of fat mainly in the shoulder girdle, face, abdomen), leads to the development of hypercholesterolemia.
Carbohydrate metabolism: increases the absorption of carbohydrates from the gastrointestinal tract (GIT), increases the activity of glucose-6-phosphatase, leading to an increase in the flow of glucose from the liver into the blood, increases the activity of phosphoenolpyruvate carboxylase and the synthesis of aminotransferases, leading to the activation of gluconeogenesis.
Water-electrolyte metabolism: retains sodium ions and water in the body, stimulates the excretion of potassium ions (mineralocorticoid activity), reduces the absorption of calcium from the gastrointestinal tract, “washes out” calcium ions from the bones and increases their excretion by the kidneys.
The anti-inflammatory effect is associated with inhibition of the release of inflammatory mediators by eosinophils; inducing the formation of lipocortin and reducing the number of mast cells that produce hyaluronic acid; decreased capillary permeability; stabilization of cell membranes and organelle membranes (especially lysosomal ones).
The antiallergic effect develops as a result of suppression of the synthesis and secretion of allergy mediators, inhibition of the release of histamine and other biologically active substances from sensitized mast cells and basophils, inhibition of the maturation and differentiation of T- and B-lymphocytes and mast cells, decreased sensitivity of effector cells to allergy mediators, inhibition of antibody formation, and changes in the body’s immune response.
Increases the sensitivity of beta-adrenergic receptors of small and medium caliber bronchi to endogenous catecholamines and exogenous sympathomimetics, reduces the viscosity of the secretion of the bronchial mucosa due to inhibition or reduction of its production.
The immunosuppressive effect is due to inhibition of the release of cytokines (interleukin-1, interleukin-2, interferon gamma) from lymphocytes and macrophages. Suppresses the synthesis and secretion of ACTH and, secondarily, the synthesis of endogenous corticosteroids.
Inhibits the secretion of thyroid-stimulating hormone (TSH) and follicle-stimulating hormone (FSH).
Suppresses the release of beta-lipotropin, but does not reduce the content of circulating beta-endorphin.
Inhibits connective tissue reactions during the inflammatory process and reduces the possibility of scar tissue formation.
Betamethasone sodium phosphate is a readily soluble compound that is well absorbed after parenteral administration into tissues and provides a rapid effect. Betamethasone dipropionate has a slower absorption. By combining these betamethasone salts it is possible to create a drug with both short-term (but fast) and long-term action. Depending on the method of application (intramuscular (IM), intra-articular, periarticular, intradermal (IV)) a general or local effect is achieved.
Pharmacokinetics
Betamethasone sodium phosphate is highly soluble in water and, after intramuscular administration, quickly undergoes hydrolysis and is almost immediately absorbed from the injection site, which ensures a rapid onset of therapeutic action. Almost completely eliminated within one day after administration.
Betamethasone dipropionate is slowly absorbed from the depot, metabolized gradually, which determines the long-term effect of the drug, and is eliminated over more than 10 days.
Betamethasone binds well to plasma proteins (62.5%). Metabolized in the liver to form predominantly inactive metabolites. It is excreted primarily by the kidneys.
Special instructions
Special instructions
Severe nervous system complications (including death) have been reported with epidural and intrathecal administration of corticosteroids (with or without fluoroscopic guidance), including, but not limited to, spinal cord infarction, paraplegia, quadriplegia, cortical blindness, and stroke. Since the safety and effectiveness of epidural administration of GCS have not been established, this route of administration is not indicated for this group of drugs.
Recommended routes of administration are listed in the “Method of administration and dosage” section.
Intravascular administration of the drug must be avoided.
Due to the lack of data regarding the risk of calcification, injection of the drug into the intervertebral space is contraindicated.
Rare cases of anaphylactoid/anaphylactic reactions (up to the development of anaphylactic shock) have been reported with parenteral administration of GCS. The necessary precautions should be taken before administering the drug, especially if the patient has a history of allergic reactions to GCS.
The dosage regimen and route of administration are determined individually, depending on the indications, severity of the disease and patient response.
The dose should be as small as possible and the period of use as short as possible. The initial dose is adjusted until the desired therapeutic effect is achieved. Then gradually reduce the dose of Dipromet to the minimum effective maintenance dose. If there is no effect from the therapy or if it is used for a long time, the drug is discontinued in the same way, gradually reducing the dose.
If a stressful situation (not related to the disease) occurs or threatens to occur, it may be necessary to increase the dose of Dipromet.
The patient’s condition is monitored for at least one year after completion of long-term therapy or use in high doses.
Administration of the drug into soft tissues, into the lesion and intra-articularly can, with a pronounced local effect, simultaneously lead to a systemic effect.
The drug Dipromet contains two active ingredients – betamethasone derivatives, one of which – betamethasone sodium phosphate – quickly penetrates the systemic bloodstream, and therefore its possible systemic effect should be taken into account.
The use of Dipromet may increase the patient’s emotional instability or tendency to psychosis.
When using Dipromet in patients with diabetes mellitus, adjustment of hypoglycemic therapy may be required.
Patients receiving corticosteroids should not be vaccinated against smallpox. Other immunizations should not be carried out in patients receiving GCS (especially in high doses), due to the possibility of developing neurological complications and a low immune response (lack of antibody formation). However, immunization is possible during replacement therapy (for example, with primary adrenal insufficiency). Patients receiving Dipromet in doses that suppress the immune system should be warned to avoid contact with patients with chickenpox and measles (especially important when using the drug in children).
It is possible to suppress the reaction when performing skin tests during the use of GCS.
When using the drug Dipromet, it should be taken into account that GCS can mask the signs of an infectious disease, as well as reduce the body’s resistance to infections.
It is necessary to carefully observe the rules of asepsis and antisepsis when administering the drug.
Caution must be exercised when using the drug in patients at high risk of infection (on hemodialysis or with dentures).
The use of Dipromet for active tuberculosis is possible only in cases of fulminant or disseminated tuberculosis in combination with adequate anti-tuberculosis therapy. When using Dipromet in patients with latent tuberculosis or a positive reaction to tuberculin, careful medical supervision is necessary due to the danger of reactivation of tuberculosis. With long-term use of GCS, such patients should receive specific chemotherapy. When using rifampicin prophylactically, acceleration of the hepatic clearance of betamethasone should be taken into account (dosage adjustment may be required).
If there is fluid in the joint cavity, a septic process should be excluded. A noticeable increase in pain, swelling, increased temperature of the surrounding tissues and further limitation of joint mobility indicate septic arthritis. It is necessary to conduct a study of aspirated joint fluid. Once the diagnosis is confirmed, appropriate antibacterial therapy must be prescribed. The use of Dipromet in septic arthritis is contraindicated.
Repeated injections into a joint for osteoarthritis may increase the risk of joint destruction. The introduction of GCS into the tendon tissue gradually leads to tendon rupture.
After successful intra-articular therapy, the patient should avoid overloading the joint.
Long-term use of corticosteroids can lead to posterior subcapsular cataracts (especially in children), glaucoma with possible damage to the optic nerve, and may contribute to the development of secondary eye infections (fungal or viral). It is necessary to periodically conduct an ophthalmological examination, especially in patients receiving Dipromet for more than 6 months.
The use of medium and high doses of corticosteroids can lead to increased blood pressure, sodium and fluid retention in the body, and increased excretion of potassium from the body (these phenomena are less likely when taking synthetic corticosteroids, unless they are used in high doses). In this case, the need to prescribe potassium-containing drugs and a diet with limited salt should be considered. All corticosteroids enhance calcium excretion.
With the simultaneous use of Dipromet and cardiac glycosides or drugs that affect the electrolyte composition of plasma, monitoring of the water-electrolyte balance is required.
Acetylsalicylic acid is used with caution in combination with betamethasone for hypoprothrombinemia.
The effect of GCS is enhanced in patients with hypothyroidism and liver cirrhosis.
The development of secondary adrenal insufficiency due to too rapid withdrawal of GCS is possible within several months after the end of therapy. If a stressful situation occurs or is threatened during this period, therapy with Dipromet should be resumed and a mineralocorticoid should be prescribed at the same time (due to a possible disruption of mineralocorticoid secretion). Gradual withdrawal of GCS can reduce the risk of developing secondary adrenal insufficiency.
With the use of GCS, changes in sperm motility and number are possible.
During long-term therapy with GCS, it is advisable to consider the possibility of switching from parenteral to oral use of GCS, taking into account the assessment of the benefit/risk ratio.
Caution must be exercised when using GCS in elderly patients; in patients with ulcerative colitis with threat of perforation, with an abscess or other purulent infections, diverticulitis, with the presence of recently created intestinal anastomoses, active or latent peptic ulcer of the stomach and/or intestines, renal or hepatic failure, arterial hypertension, osteoporosis, myasthenia, confirmed or suspected parasitic infections (for example, strongyloidiasis).
With systemic and local (including intranasal, inhalation and intraocular) use of GCS, visual impairment may occur. If a patient experiences symptoms such as blurred vision or other visual disturbances, referral to an ophthalmologist should be considered to identify possible causes, including cataracts, glaucoma, or rare diseases such as central serous chorioretinopathy (CSC), which have been observed in some cases with systemic or topical use of corticosteroids.
Use in pediatrics
Children undergoing therapy with Dipromet (especially long-term therapy) should be under close medical supervision for possible growth retardation and the development of secondary adrenal insufficiency.
Use in athletes
Patients participating in competitions under the control of the World Anti-Doping Agency (WADA) should familiarize themselves with the WADA rules before starting treatment with the drug, since the use of betamethasone may affect the results of doping control.
Impact on the ability to drive vehicles and machinery
There are no data on the effect of betamethasone on the ability to drive vehicles and machines. However, if undesirable reactions (blurred vision, dizziness, insomnia) occur during long-term treatment, you should refrain from driving vehicles and machinery.
Active ingredient
Active ingredient
Betamethasone
Composition
Composition
1 ml (one pre-filled syringe) contains:
active ingredients:
betamethasone dipropionate – 6.43 mg in terms of betamethasone – 5.00 mg;
betamethasone sodium phosphate – 2.63 mg in terms of betamethasone – 2.00 mg;
excipients: methyl parahydroxybenzoate – 1.30 mg; propyl parahydroxybenzoate – 0.20 mg; benzyl alcohol – 9.00 mg; macrogol-4000 – 20.00 mg; carmellose sodium – 5.00 mg; sodium hydrogen phosphate dodecahydrate – 5.04 mg; disodium edetate – 0.10 mg; sodium chloride – 5.00 mg; polysorbate 80 – 0.625 mg; hydrochloric acid solution 1 M – up to pH = 7.4 ± 0.1; water for injection – up to 1.00 ml (1.0127 g).
Pregnancy
Pregnancy
Pregnancy
Due to the lack of controlled studies of the safety of betamethasone during pregnancy, the use of Dipromet during pregnancy or in women with preserved reproductive potential is indicated only when the expected therapeutic effect for the mother outweighs the risk of a possible negative effect of the drug on the fetus.
The condition of patients with fluid retention or gestosis in the second half of pregnancy (especially severe – preeclampsia, eclampsia) should be carefully monitored.
GCS penetrate the placental barrier and can reach high concentrations in the fetus. Newborns whose mothers received therapeutic doses of GCS during pregnancy should be under medical supervision (for early detection of signs of adrenal insufficiency).
The use of GCS in pregnant animals can cause fetal malformations, including cleft palate (“cleft palate”), intrauterine growth retardation, and affect the growth and development of the brain. There is no data on an increase in the incidence of congenital malformations, such as cleft palate/lip, in humans during the use of GCS. However, with prolonged or repeated use during pregnancy, the use of GCS may increase the risk of intrauterine growth retardation. Theoretically, after prenatal use of GCS, it is possible to develop adrenal hypofunction in newborns, which, as a rule, resolves spontaneously after birth and in rare cases is clinically significant. When using betamethasone during pregnancy, cases of myocardial hypertrophy and gastroesophageal reflux have been reported in newborns.
When used systemically in pregnant women, betamethasone can lead to a transient decrease in heart rate (HR) and inhibition of fetal biophysical activity, which are widely used to assess the condition of the fetus. These characteristics may include decreased respiratory rate, fetal motility, and fetal heart rate.
Breastfeeding period
If it is necessary to use betamethasone during breastfeeding, given the importance of GCS therapy for the mother and the possibility of developing undesirable effects in the child, breastfeeding should be stopped.
Contraindications
Contraindications
hypersensitivity to betamethasone or any of the excipients of the drug, or other corticosteroids;
systemic mycoses;
intravenous, subcutaneous, epidural, intrathecal administration;
injection directly into muscle tendons;
with intra-articular injection: unstable joint, infectious arthritis;
injection into infected cavities and intervertebral space;
children under 3 years of age (contains benzyl alcohol);
coagulation disorders (including treatment with anticoagulants);
breastfeeding period;
simultaneous administration of immunosuppressive doses of the drug with live and attenuated vaccines;
thrombocytopenic purpura (intramuscular administration of the drug);
swelling of the brain due to traumatic brain injury.
With caution
Parasitic and infectious diseases of a viral, fungal or bacterial nature (currently or recently suffered, including recent contact with a patient) – herpes simplex, herpes zoster (viremic phase), chicken pox, measles; amebiasis, strongyloidiasis (established or suspected); active and latent tuberculosis. Use for severe infectious diseases is permissible only against the background of specific antimicrobial therapy.
Post-vaccination period (a period of 8 weeks before and 2 weeks after vaccination), lymphadenitis after BCG vaccination.
Immunodeficiency conditions (including AIDS or HIV infection).
Diseases of the gastrointestinal tract (GIT): peptic ulcer of the stomach and duodenum, esophagitis, gastritis, acute or latent peptic ulcer, recently created intestinal anastomosis, ulcerative colitis with threat of perforation or abscess formation, diverticulitis, abscess or other purulent infections.
Diseases of the cardiovascular system, incl. recent myocardial infarction (in patients with acute and subacute myocardial infarction, the necrosis focus may spread, the formation of scar tissue may slow down and, as a result, the heart muscle may rupture); decompensated chronic heart failure; arterial hypertension, hyperlipidemia.
Endocrine diseases – diabetes mellitus (including decreased glucose tolerance), thyrotoxicosis, hypothyroidism, Itsenko-Cushing’s disease.
Chronic renal and/or liver failure, nephrourolithiasis, liver cirrhosis.
Hypoalbuminemia and conditions predisposing to its occurrence.
Systemic osteoporosis, grade III-IV obesity, myasthenia gravis, acute psychosis, poliomyelitis (except for the form of bulbar encephalitis), open- and closed-angle glaucoma, eye diseases caused by Herpes simplex (due to the risk of corneal perforation), pregnancy.
In elderly patients due to increased sensitivity to GCS, especially in postmenopausal women (high risk of osteoporosis).
With convulsive syndrome.
For intra-articular administration: the general serious condition of the patient, the ineffectiveness (or short duration) of the action of 2 previous injections (taking into account the individual properties of the GCS used).
Precautionary measures are required in elderly patients due to increased sensitivity to GCS, especially in postmenopausal women (high risk of osteoporosis); with convulsive syndrome.
Side Effects
Side Effects
The frequency of development and severity of adverse reactions (AR), as with the use of other corticosteroids, depend on the size of the dose used and the duration of use of the drug. These reactions are usually reversible and can be eliminated or reduced by reducing the dose.
From the immune system: allergic or anaphylactic reactions, including anaphylactic shock, angioedema.
From the nervous system: convulsions, increased intracranial pressure with papilledema (usually at the end of therapy), dizziness, headache, neuritis, neuropathy, paresthesia, with intrathecal administration – arachnoiditis, meningitis, paresis/paralysis, sensory disturbances.
From the psyche: euphoria, mood changes, depression (with severe psychotic reactions), personality disorders, increased irritability, insomnia.
Visual disorders: posterior subcapsular cataract, increased intraocular pressure, glaucoma, exophthalmos; blurred vision; in rare cases, blindness (when the drug is administered to the face and head).
Cardiac disorders: chronic heart failure (in predisposed patients), cardiac arrhythmias, bradycardia, tachycardia, hypertrophic myopathy in premature infants, myocardial rupture after recent myocardial infarction.
Vascular disorders: decreased blood pressure, increased blood pressure, thromboembolic complications, vasculitis.
From the endocrine system: secondary adrenal insufficiency (especially during periods of stress due to illness, injury, surgery); Itsenko-Cushing syndrome; decreased glucose tolerance; “steroid” diabetes mellitus or manifestation of latent diabetes mellitus; increased need for insulin or oral hypoglycemic drugs; when used during pregnancy – disruption of intrauterine development of the fetus; delayed growth and sexual development in children; hirsutism; hypertrichosis; suppression of adrenal and pituitary function.
Metabolic and nutritional disorders: hypernatremia, increased potassium excretion, increased calcium excretion, hypokalemic alkalosis, fluid retention in tissues, negative nitrogen balance (due to protein catabolism), lipomatosis (including mediastinal and epidural lipomatosis, which can cause neurological complications), weight gain, increased appetite.
Gastrointestinal disorders: erosive and ulcerative lesions of the gastrointestinal tract with possible subsequent perforation and bleeding, pancreatitis, flatulence, hiccups, nausea.
Disorders of the liver and biliary tract: hepatomegaly, increased activity of liver enzymes (usually reversible).
Musculoskeletal and connective tissue disorders: muscle weakness, “steroid” myopathy, loss of muscle mass, increased myasthenic symptoms in pseudoparalytic myasthenia gravis, osteoporosis, vertebral compression fracture, aseptic necrosis of the femoral or humeral head, pathological fractures of tubular bones, tendon ruptures, joint instability (with repeated intra-articular injections).
Disorders of the skin and subcutaneous tissues: impaired wound healing, atrophy and thinning of the skin, petechiae, ecchymoses, increased sweating, dermatitis, “steroid” acne, stretch marks, a tendency to develop pyoderma and candidiasis, decreased response to skin tests, urticaria, rash, thinning of scalp hair, allergic dermatitis, erythema.
Disorders of the genital organs and mammary gland: menstrual irregularities, changes in motility and sperm count.
General disorders and disorders at the injection site: rarely – hyper- or hypopigmentation, subcutaneous and cutaneous atrophy, aseptic abscesses, “flush” of blood to the face after injection (or intra-articular injection), neurogenic arthropathy.
Interaction
Interaction
GCS (including betamethasone) are metabolized by the enzyme CYP3A4.
Concomitant use with strong CYP3A4 inhibitors (for example, ketoconazole, itraconazole, clarithromycin, ritonavir or drugs containing cobicistat) may lead to increased exposure to glucocorticosteroids and, consequently, an increased risk of developing systemic adverse reactions. The combined use of betamethasone and strong CYP3A4 inhibitors should be avoided if the expected benefit from GCS therapy does not outweigh the risk of developing systemic adverse reactions. If concomitant use of betamethasone with strong CYP3A4 inhibitors is necessary, patients should be carefully monitored for the risk of developing systemic adverse reactions.
With the simultaneous use of phenobarbital, rifampicin, phenytoin or ephedrine, it is possible to accelerate the metabolism of betamethasone while reducing its therapeutic activity.
When using betamethasone and estrogens simultaneously, betamethasone dosage adjustment may be required (due to the risk of overdose).
When betamethasone and potassium-sparing diuretics are used together, the likelihood of developing hypokalemia increases.
The simultaneous use of corticosteroids and cardiac glycosides increases the risk of arrhythmia or digitalis intoxication (due to hypokalemia). Betamethasone may enhance potassium excretion caused by amphotericin B.
When betamethasone and oral anticoagulants are used together, changes in blood clotting are possible, requiring adjustment of the dose of anticoagulants.
With the combined use of GCS with non-steroidal anti-inflammatory drugs (NSAIDs) or with ethanol (or ethanol-containing drugs), it is possible to increase the incidence or intensity of erosive and ulcerative lesions of the gastrointestinal tract.
When used together, GCS can reduce the concentration of salicylates in the blood plasma.
Simultaneous administration of corticosteroids and somatropin may slow down the absorption of the latter (doses of betamethasone exceeding 0.3-0.45 mg/m2 of body surface per day should be avoided).
GCS may interfere with the nitrogen blue tetrazole test for bacterial infection and cause a false negative result.
Aminoglutethimide may increase or decrease the suppression of adrenal function caused by corticosteroids. Aminoglutethimide causes a decrease in adrenal cortisol secretion, followed by an increase in pituitary adrenocorticotropic hormone (ACTH) secretion, which can counteract the blockade of adrenocortical steroid synthesis by aminoglutethimide, leading to increased adrenal function. Therefore, doctors should be advised to familiarize themselves with information on the simultaneous use of Dipromet with aminoglutethimide.
GCS may reduce the effect of cholinesterase inhibitors, which can lead to the development of severe muscle weakness in patients with myasthenia gravis. If possible, cholinesterase inhibitors should be discontinued at least 24 hours before starting GCS therapy.
With the simultaneous use of GCS and isoniazid, a decrease in the concentration of isoniazid in the blood plasma is possible. Patients taking isoniazid should be carefully monitored.
The simultaneous use of cyclosporine and corticosteroids may lead to increased concentrations of cyclosporine and increased effect of corticosteroids. There is a high risk of developing seizures.
With the simultaneous use of GCS with macrolide antibiotics, a significant decrease in the elimination of GCS is possible.
When used simultaneously with colesteramine, it is possible to increase the excretion of GCS.
When using betamethasone in patients with diabetes mellitus, adjustment of hypoglycemic therapy may be required.
Overdose
Overdose
Symptoms
Acute overdose of betamethasone does not lead to life-threatening situations. Administration of high doses of GCS for several days does not lead to undesirable consequences (except for cases of very high doses or if the patient has diabetes mellitus, glaucoma, exacerbation of erosive and ulcerative lesions of the gastrointestinal tract, or with the simultaneous use of cardiac glycosides, indirect anticoagulants or potassium-sparing diuretics).
Treatment
Careful medical monitoring of the patient’s condition is necessary; Optimal fluid intake should be maintained and electrolytes in plasma and urine should be monitored (especially the ratio of sodium and potassium ions). If necessary, appropriate therapy should be carried out.
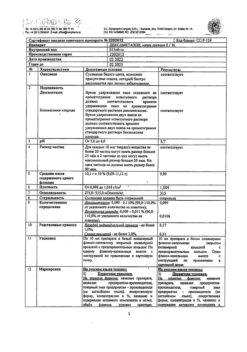
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C, in the original packaging (in a pack).
Keep out of the reach of children.
Shelf life
Shelf life
2 years.
Do not use after expiration date!
Manufacturer
Manufacturer
K.O.Rompharm Company S.R.L., Romania
Additional information
| Shelf life | 2 years. Do not use after the expiration date! |
|---|---|
| Conditions of storage | At the temperature not more than 25 °С, in the original package (in the package). Keep out of reach of children. |
| Manufacturer | C.O.Rompharm Company S.R.L., Romania |
| Medication form | suspension for injection |
| Brand | C.O.Rompharm Company S.R.L. |
Related products
Buy Diprometa, 7 mg/ml suspension 1 ml with delivery to USA, UK, Europe and over 120 other countries.