No products in the cart.
Dilaxa, capsules 100 mg 10 pcs
€12.68 €10.57
Description
Pain, Joint pain (arthralgia), Osteoarthritis, Rheumatoid arthritis, Back pain, Radiculitis, Neck pain, Sciatica, Pain after injuries and operations, Lumbago, Arthritis, Painful menstruation (algodysmenorrhea), Osteochondrosis, Arthritis
- Symptomatic treatment of osteoarthritis, rheumatoid arthritis and ankylosing spondylitis.
- Pain syndrome (back pain, musculoskeletal, postoperative and other types of pain).
- Treatment of primary dysmenorrhea.
.
Indications
Indications
Symptomatic treatment of osteoarthritis, rheumatoid arthritis and ankylosing spondylitis.
Pain syndrome (back pain, musculoskeletal, postoperative and other types of pain).
Treatment of primary dysmenorrhea.
Pharmacological effect
Pharmacological effect
non-steroidal anti-inflammatory drug (NSAID)
Special instructions
Special instructions
Diseases of the gastrointestinal tract (peptic ulcer of the stomach and duodenum, ulcerative colitis, Crohn’s disease, history of bleeding), the presence of Helicobacter pylori infection, simultaneous use with digoxin, anticoagulants (for example, warfarin), antiplatelet agents (for example, acetylsalicylic acid, clopidogrel), glucocorticosteroids (GCS) for oral administration (for example, prednisolone), diuretics, selective serotonin reuptake inhibitors (for example, citalopram, fluoxetine, paroxetine, sertraline), inhibitors of the CYP2C9 isoenzyme, in patients who are poor metabolizers or suspected of such a condition, fluid retention and edema, moderate liver dysfunction (see section “Special Instructions”), history of liver disease, hepatic porphyria, impaired renal function (CC 30-60 ml/min), significant decrease in circulating blood volume (including after surgery), diseases of the cardiovascular system, arterial hypertension (see. section “Special Instructions”), cerebrovascular diseases, dyslipidemia/hyperlipidemia, diabetes mellitus, peripheral arterial diseases, long-term use of NSAIDs, severe somatic diseases, in elderly patients (including those receiving diuretics, debilitated patients with low body weight), smoking, tuberculosis, alcoholism.
Contraindicated for persons under 18 years of age.
Elderly patients: usually no dose adjustment is required. However, in patients weighing less than 50 kg, it is better to start treatment with the minimum recommended dose.
Liver dysfunction: in patients with mild hepatic impairment (Child-Pugh class A), no dose adjustment is required. In patients with moderate hepatic impairment (Child-Pugh class B), the initial recommended dose of the drug should be reduced by half. There is no experience with the use of Dilaxa® in patients with severe liver failure (class C according to the Child-Pugh classification).
Renal impairment: No dose adjustment is required in patients with mild to moderate renal impairment. There is no experience with the use of Dilaxa® in patients with severe renal failure.
Dilaxa®, which has an antipyretic effect, can reduce the diagnostic value of fever, which makes it difficult to diagnose an infection.
Effect on the cardiovascular system
Celecoxib, like all coxibs, may increase the risk of serious cardiovascular events such as blood clots, myocardial infarction, and stroke, which can be fatal. The risk of developing these reactions increases with increasing dose, duration of drug use, and in patients with diseases of the cardiovascular system or with risk factors for developing cardiovascular diseases. In order to reduce the risk of developing these reactions, Dilaxa® should be used in the minimum effective doses and for the shortest possible short course (at the discretion of the attending physician). The attending physician and patient should consider the possibility of developing such complications even in the absence of previously known symptoms of impaired cardiovascular function. Patients should be informed of the symptoms of serious adverse cardiovascular effects and the measures to take if they occur.
When using NSAIDs (selective COX-2 inhibitors) in patients after coronary artery bypass surgery to treat pain in the first 10-14 days, an increase in the incidence of myocardial infarction and cerebrovascular accidents is possible.
Celecoxib does not have an antiplatelet effect on platelets, so they should not replace acetylsalicylic acid for the prevention of thromboembolism. Also, in this regard, antiplatelet therapy (for example, acetylsalicylic acid) should not be discontinued in patients at risk of developing thromboembolic complications.
Like all NSAIDs, celecoxib can lead to an increase in blood pressure, which can cause complications from the cardiovascular system. Like other NSAIDs, celecoxib should be used with caution in patients with hypertension. Blood pressure should be monitored at the initiation and duration of celecoxib therapy.
Effect on the digestive system
Extremely rare cases of perforation, ulceration and bleeding from the gastrointestinal tract have been observed in patients taking celecoxib. The risk of developing these complications when using NSAIDs is highest in elderly patients, patients with cardiovascular diseases, in patients simultaneously receiving acetylsalicylic acid, and in patients with gastrointestinal diseases such as ulcers, bleeding, inflammatory processes in the acute stage and in history. Other risk factors for the development of bleeding from the gastrointestinal tract are the simultaneous use of oral corticosteroids or anticoagulants, long-term NSAID therapy, smoking, and ethanol intake. Most spontaneous reports of serious and fatal adverse reactions occurred in elderly and debilitated patients.
Concomitant use with warfarin and other anticoagulants
When NSAIDs are used simultaneously with oral anticoagulants, the risk of bleeding increases. Caution is advised when using these drugs together. Oral anticoagulants include warfarin, coumarin anticoagulants, and direct oral anticoagulants (eg, apixaban, dabigatran, and rivaroxaban). Serious (some fatal) bleeding events have been reported in patients receiving warfarin or similar agents concomitantly with celecoxib. Given the presence of reports of prolongation of prothrombin time, after starting treatment with Dilaxa® or when changing its dose, blood clotting parameters should be monitored.
Fluid retention and swelling
As with other drugs that inhibit Pg synthesis, some patients taking Dilaxa may experience fluid retention and edema, so caution should be exercised when using the drug in patients with conditions predisposing or worsened by fluid retention. Patients with a history of heart failure or hypertension should be closely monitored.
Effect on kidney function
NSAIDs, including celecoxib, may have toxic effects on renal function. Celecoxib was found to be no more toxic than other NSAIDs.
Dilaxa® should be used with caution in patients with impaired renal function, heart failure, impaired liver function, in patients taking diuretics, ACE inhibitors, ARB II, and in elderly patients. Renal function should be carefully monitored in such patients. Caution should be exercised when using Dilaxa® in patients with dehydration. In such cases, it is advisable to rehydrate and then begin therapy with Dilaxa®.
Effect on liver function
Dilaxa® should not be used in patients with severe liver dysfunction (class C according to the Child-Pugh classification). In patients with moderate hepatic impairment (Child-Pugh class B), Dilaxa® should be used with caution and in the minimum effective dose. In rare cases, severe liver dysfunction has occurred, including fulminant hepatitis (sometimes fatal), liver necrosis and liver failure (sometimes fatal or requiring liver transplantation). Most of these reactions occurred 1 month after starting celecoxib.
Patients with symptoms and/or signs of liver dysfunction or those patients in whom laboratory tests have demonstrated liver dysfunction should be closely monitored for the development of more severe liver reactions during treatment with Dilaxa.
Anaphylactic reactions
Cases of anaphylactic reactions have been reported when taking Dilaxa®.
Serious skin reactions
In extremely rare cases, serious skin reactions such as exfoliative dermatitis, Stevens-Johnson syndrome and toxic epidermal necrolysis have been reported with celecoxib, some of which have been fatal. The risk of developing such reactions is higher at the beginning of therapy; in most reported cases they occurred in the first month of therapy. If a skin rash, changes in the mucous membranes or other signs of hypersensitivity appear, you should stop taking Dilaxa®.
GCS therapy
GCS therapy should not be replaced with Dilaxa® in the treatment of glucocorticosteroid deficiency.
Inhibition of the function of the CYP2D6 isoenzyme
Celecoxib has been found to be a moderate inhibitor of the CYP2D6 isoenzyme. During the period of initiation of therapy with celecoxib, the dose of drugs metabolized by the CYP2D6 isoenzyme should be reduced, and after completion of treatment with celecoxib, the dose of these drugs should be increased (see section “Interaction with other drugs”).
Special information on excipients
Dilaxa® contains lactose, therefore the drug is contraindicated in patients with lactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome.
Caution must be exercised when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions, since Dilaxa® may cause dizziness and other side effects that may affect these abilities.
Active ingredient
Active ingredient
Celecoxib
Composition
Composition
1 capsule 100 mg/200 mg contains:
Active ingredient:
Celecoxib 100.00 mg/200.00 mg
Excipients: lactose monohydrate, sodium lauryl sulfate, povidone-K30, croscarmellose sodium, magnesium stearate
Hard gelatin capsules No. 3
Body: titanium dioxide (E171), gelatin
Cap: titanium dioxide (E171), gelatin
Hard gelatin capsules No. 1
Body: titanium dioxide (E171), iron oxide yellow (E172), gelatin
Cap: titanium dioxide (E171), iron oxide yellow (E172), gelatin
Pregnancy
Pregnancy
Pregnancy
Animal studies (rats and rabbits) have shown reproductive toxicity, including developmental defects. The use of Pg synthesis inhibitors may adversely affect pregnancy. Data from epidemiological studies suggest an increased risk of miscarriage after the use of Pg synthesis inhibitors in early pregnancy. There is insufficient data on the use of celecoxib in pregnant women, but a potential risk cannot be excluded. Celecoxib, like other drugs that inhibit Pg synthesis, can cause weakness of labor and premature closure of the ductus arteriosus in the third trimester of pregnancy.
When used in the second and third trimesters of pregnancy, NSAIDs, including celecoxib, can cause renal dysfunction in the fetus, which can lead to a decrease in the volume of amniotic fluid or, in severe cases, to oligohydramnios. These effects may develop soon after the start of treatment and are usually reversible.
The use of Dilaxa® is contraindicated during pregnancy and women planning pregnancy. If pregnancy occurs during treatment, celecoxib should be discontinued.
Breastfeeding period
Celecoxib is excreted into milk in lactating rats in concentrations similar to those in plasma. Studies have shown that celecoxib is excreted into women’s breast milk in very low concentrations. When using Dilaxa®, breastfeeding should be stopped.
Fertility
According to the mechanism of action, when NSAIDs, including celecoxib, are used in the ovaries, there may be a delay in follicle maturation or failure to rupture the follicle wall, which may be associated with reversible infertility.
Contraindications
Contraindications
Hypersensitivity to celecoxib or any other component of the drug.
Known hypersensitivity to sulfonamides.
Complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid or other NSAIDs, including other COX-2 inhibitors (including a history).
The period after coronary artery bypass surgery.
Active erosive and ulcerative lesions of the mucous membrane of the stomach or duodenum, peptic ulcer of the stomach and duodenum in the acute stage or gastrointestinal bleeding.
Inflammatory bowel diseases (Crohn’s disease, ulcerative colitis) in the acute phase.
Chronic heart failure (II-IV functional class according to the NYHA classification).
Clinically confirmed coronary heart disease, peripheral arterial disease and cerebrovascular disease in an advanced stage.
Hemorrhagic stroke.
Subarachnoid hemorrhage.
Pregnancy and breastfeeding (see section “Use during pregnancy and breastfeeding”).
Severe liver failure (class C according to the Child-Pugh classification) (no experience with use).
Severe renal failure (creatinine clearance less than 30 ml/min), progressive kidney disease, confirmed hyperkalemia (no experience with use).
Age up to 18 years (no experience of use).
Lactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome (Dilaxa® contains lactose).
Side Effects
Side Effects
Adverse reactions (AR) are presented by class of organ system and by frequency of occurrence in accordance with the data obtained:
Adverse events with a frequency of more than 0.01% and more often than in the placebo group were observed when using celecoxib in doses of 100-800 mg/day in patients with osteoarthritis and rheumatoid arthritis for up to 12 weeks during 12 placebo- and/or active-drug-controlled clinical studies. In additional studies using non-selective NSAIDs (comparator), approximately 7400 patients with arthritis received celecoxib at doses up to 800 mg/day, including approximately 2300 patients treated for at least 1 year or more; NRs were consistent with those in patients with osteoarthritis and rheumatoid arthritis;
ADRs with a frequency higher than in the placebo group were observed in patients receiving celecoxib at a dose of 400 mg/day in long-term studies (up to 3 years) studying the prevention of intestinal polyps (Adenoma Prevention with Celecoxib (APC) and Prevention of Colorectal Sporadic Adenomatous Polyps (PreSAP); studying the effect of the drug on cardiovascular safety in patients with sporadic adenomatous polyps);
Adverse events in the post-marketing period based on spontaneous reports during treatment with celecoxib in more than 70 million patients (at different doses, with different durations and for different indications for use). Although ADRs were observed in the post-marketing period, clinical trial data were used to estimate the incidence of ADRs. The incidence of adverse reactions was calculated based on a pooled meta-analysis that combined many studies in which 38,102 patients received the drug.
ADRs are grouped according to MedDRA terminology and frequency of occurrence: very common (≥ 1/10); often (from ≥ 1/100 to < 1/10); uncommon (from ≥ 1/1000 to < 1/100); rare (from ≥ 1/10,000 to < 1/1000); very rare (<1/10,000); frequency unknown (cannot be estimated from available data).
Adverse drug reactions observed in clinical trials and observational experience with celecoxib (MedDRA terminology)1,2
Infectious and parasitic diseases:
often: sinusitis, upper respiratory tract infections, pharyngitis, urinary tract infections.
Blood and lymphatic system disorders:
uncommon: anemia;
rarely: leukopenia, thrombocytopenia;
very rare: pancytopenia4.
Immune system disorders:
often: hypersensitivity;
very rare: anaphylactic shock4, anaphylactic reactions4.
Metabolic and nutritional disorders:
uncommon: hyperkalemia.
Mental disorders:
often: insomnia;
uncommon: anxiety, depression, fatigue;
rarely: confusion, hallucinations4.
Nervous system disorders:
often: dizziness, hypertension, headache4;
uncommon: cerebral infarction1, paresthesia, drowsiness;
rarely: ataxia, dysgeusia;
very rare: intracranial hemorrhage (including death)4, aseptic meningitis4, epilepsy (including exacerbation of epilepsy)4, ageusia4, anosmia4.
Visual disorders:
uncommon: blurred vision, conjunctivitis4;
rarely: intraocular hemorrhage4;
very rare: retinal artery occlusion4, retinal vein occlusion4.
Hearing and labyrinth disorders:
uncommon: tinnitus, hearing loss1.
Cardiac disorders:
often: myocardial infarction1;
uncommon: heart failure, palpitations, tachycardia;
rarely: arrhythmia4.
Vascular disorders:
very often: arterial hypertension1 (including worsening arterial hypertension);
rarely: pulmonary embolism4, hot flashes4;
very rare: vasculitis4.
Disorders of the respiratory system, chest and mediastinal organs:
often: rhinitis, cough, shortness of breath1;
uncommon: bronchospasm4;
rare: pneumonitis4.
Gastrointestinal disorders:
often: nausea4, abdominal pain, diarrhea, dyspepsia, flatulence, vomiting1, dysphagia1;
uncommon: constipation, gastritis, stomatitis, inflammation of the gastrointestinal tract (including intensification of existing inflammation), belching;
rare: gastrointestinal bleeding4, duodenal ulcer, gastric ulcer, esophageal ulcer, intestinal ulcer, large intestinal ulcer, intestinal perforation, esophagitis, melena, pancreatitis, colitis4.
Disorders of the liver and biliary tract:
uncommon: impaired liver function, increased activity of liver enzymes (including alanine aminotransferase and aspartate aminotransferase);
rarely: hepatitis4;
very rare: liver failure4 (sometimes with death or the need for liver transplantation), fulminant hepatitis4 (sometimes with death), liver necrosis4, cholestasis4, cholestatic hepatitis4, jaundice4.
Disorders of the skin and subcutaneous tissues:
often: skin rash, skin itching (including generalized);
uncommon: urticaria, ecchymosis4;
rarely: Quincke’s edema4, alopecia, photosensitivity;
very rare: exfoliative dermatitis4, erythema multiforme4, Stevens-Johnson syndrome4, toxic epidermal necrolysis4, drug reaction with eosinophilia and systemic symptoms (DRESS or hypersensitivity syndrome)4, acute generalized exanthematous pustulosis (AGEP)4, bullous dermatitis4.
Musculoskeletal and connective tissue disorders:
often: arthralgia4;
uncommon: muscle spasms (calf muscle spasms);
very rare: myositis4.
Renal and urinary tract disorders:
infrequently: increased concentrations of creatinine, urea in the blood plasma;
rarely: acute renal failure4, hyponatremia4;
very rare: tubulointerstitial nephritis4, nephrotic syndrome4, minimal change disease4.
Disorders of the genital organs and breast:
rarely: menstrual irregularities4;
frequency unknown: infertility in women (decreased fertility in women)3.
General disorders and disorders at the injection site:
often: flu-like condition, peripheral edema/fluid retention;
Uncommon: facial swelling, chest pain4.
Injuries, intoxications and complications of manipulation:
often: injuries (accidental injuries).
1 adverse reaction that occurred in 2 clinical trials studying the prevention of polyp formation (APS and PreSAP lasting up to 3 years), when using celecoxib at a dose of 400 mg/day. Listed above are only adverse reactions that were previously noted in the post-registration period or that developed with a higher frequency than in studies of the drug in a population of patients with arthritis.
2 Previously unknown adverse reactions that developed in 2 clinical trials studying the prevention of polyp formation (APS and PreSAP lasting up to 3 years), when using celecoxib at a dose of 400 mg/day:
often: angina pectoris, irritable bowel syndrome, nephrolithiasis, increased plasma creatinine concentration, benign prostatic hyperplasia, weight gain;
uncommon: helicobacteriosis, herpes zoster, erysipelas, bronchopneumonia, labyrinthitis, gum infection, lipoma, vitreous floaters, conjunctival hemorrhage, deep vein thrombosis, dysphonia, hemorrhoidal hemorrhage, frequent bowel movements, ulcerative stomatitis, allergic dermatitis, ganglion, nocturia, vaginal bleeding, breast tenderness, fracture of the lower limb, increased sodium levels in the blood plasma.
3 Consulting the database to determine frequency was not informative because all studies excluded women planning a pregnancy.
4 Frequency values are based on a meta-analysis of studies in which the drug was taken by 38,102 patients.
In the final (confirmed) data obtained from the APC and PreSAP studies (data from both studies combined), in patients receiving celecoxib 400 mg/day for up to 3 years, the increase in the incidence of myocardial infarction relative to placebo was 7.6 cases per 1000 patients (uncommon). There was no increase in the incidence of stroke (without differentiation by type) compared to placebo.
Interaction
Interaction
In vitro studies have shown that celecoxib, although not a substrate of the CYP2D6 isoenzyme, inhibits its activity. Therefore, there is a possibility of drug interactions in in vivo conditions with drugs whose metabolism is associated with the CYP2D6 isoenzyme.
Warfarin and other anticoagulants: with simultaneous use, prothrombin time may be prolonged.
Fluconazole, ketoconazole: with simultaneous use of 200 mg of fluconazole 1 time per day, an increase in the concentration of celecoxib in the blood plasma by 2 times is observed. This effect is associated with inhibition of the metabolism of celecoxib by fluconazole through the CYP2C9 isoenzyme. Patients taking fluconazole (an inhibitor of the CYP2C9 isoenzyme) should reduce the recommended dose of celecoxib by half (see section “Dosage and Administration”). Ketoconazole (an inhibitor of the CYP3A4 isoenzyme) does not have a clinically significant effect on the metabolism of celecoxib.
Dextromethorphan and metoprolol: It was found that the simultaneous use of celecoxib at a dose of 200 mg per day led to an increase in the concentrations of dextromethorphan and metoprolol (substrates of the CYP2D6 isoenzyme) by 2.6 and 1.5 times, respectively. This increase in concentrations is associated with inhibition of the metabolism of CYP2D6 isoenzyme substrates by celecoxib through inhibition of the activity of the CYP2D6 isoenzyme itself.
Methotrexate: No pharmacokinetic clinically significant interactions were observed between celecoxib and methotrexate.
Antihypertensive drugs, including angiotensin-converting enzyme (ACE) inhibitors/angiotensin II receptor antagonists (ARBs), diuretics and beta-blockers: Inhibition of Pg synthesis may reduce the effect of antihypertensive drugs, including ACE inhibitors and/or ARB II, diuretics and beta-blockers. This interaction should be taken into account when celecoxib is used concomitantly with ACE inhibitors and/or ARB II, diuretics and beta-blockers. However, there was no significant pharmacodynamic interaction with lisinopril regarding the effect on blood pressure.
In elderly patients, in patients with dehydration (including patients receiving diuretic therapy) or in patients with impaired renal function, concomitant use of NSAIDs, including selective COX-2 inhibitors, with ACE inhibitors, ARB II and diuretics may lead to a deterioration of renal function, including possible acute renal failure. Usually these effects are reversible. Therefore, caution should be exercised when using these drugs simultaneously. In such cases, it is advisable to first rehydrate and then begin therapy with Dilaxa®. In addition, consideration should be given to monitoring renal function at the initiation of therapy and periodically during concomitant use of drugs.
Cyclosporine: Given that NSAIDs affect the renal synthesis of Pg, they may increase the risk of nephrotoxicity when used concomitantly with cyclosporine.
Diuretics: NSAIDs may reduce the natriuretic effect of furosemide and thiazides by reducing renal Pg synthesis in some patients. This must be taken into account when using celecoxib.
Oral contraceptives: Celecoxib does not have a clinically significant effect on the pharmacokinetics of the combined contraceptive drug (1 mg norethisterone / 35 mcg ethinyl estradiol).
Lithium: with the simultaneous use of lithium salts at a dose of 450 mg 2 times a day and celecoxib at a dose of 200 mg 2 times a day, an increase in the concentration of lithium in the blood plasma by approximately 17% was observed. Patients taking lithium should be closely monitored when using or discontinuing celecoxib. Other NSAIDs: The simultaneous use of celecoxib and other NSAIDs (not containing acetylsalicylic acid) should be avoided (the risk of side effects increases).
Other drugs: There were no clinically significant interactions between celecoxib and antacids (magnesium/aluminum hydroxide), omeprazole, glibenclamide, phenytoin or tolbutamide.
Celecoxib does not affect the antiplatelet effect of acetylsalicylic acid in low doses. Celecoxib does not have an antiplatelet effect on platelets, so it should not replace acetylsalicylic acid for the prevention of cardiovascular diseases.
In healthy volunteers, NSAIDs do not affect the pharmacokinetics of digoxin. However, with the simultaneous use of digoxin and indomethacin, ibuprofen, patients experienced an increase in the concentration of digoxin in the blood plasma. This must be taken into account when used simultaneously with other drugs that increase the concentration of digoxin in the blood plasma. There is no information on the interaction between celecoxib and digoxin. Given the other cardiovascular effects of celecoxib, caution should be exercised when coadministering digoxin. In this case, it is recommended to carefully monitor adverse reactions. Celecoxib is predominantly metabolized in the liver by the CYP2C9 isoenzyme. Since barbiturates are inducers of the CYP2C9 isoenzyme, when used simultaneously with celecoxib, a decrease in the concentration of the latter in the blood plasma may be observed.
Children: Interaction studies have only been conducted in adult patients.
Overdose
Overdose
Clinical data on overdose are limited. A single dose of up to 1200 mg and repeated doses of up to 1200 mg twice a day were not accompanied by clinically significant side effects. If an overdose is suspected, maintenance therapy should be carried out. Dialysis is presumably ineffective, since the binding of celecoxib to plasma proteins is high (97%).
Clinical pharmacology
Clinical pharmacology
Pharmacodynamics
Celecoxib has anti-inflammatory, analgesic and antipyretic effects by blocking the formation of inflammatory prostaglandins (Pg) mainly through inhibition of cyclooxygenase-2 (COX-2). Induction of COX-2 occurs in response to inflammation and leads to the synthesis and accumulation of Pg, primarily PgE2, which causes increased manifestations of inflammation (swelling and pain). At therapeutic doses in humans, celecoxib does not significantly inhibit cyclooxygenase-1 (COX-1) and does not affect the concentrations of Pg, which are synthesized as a result of activation of COX-1, as well as the normal physiological processes associated with COX-1 and occurring in tissues, primarily the stomach, intestines and platelets.
Effect on kidney function
Celecoxib reduces the renal excretion of PgE2 and 6-keto-PgF1 (a metabolite of prostacyclin), but does not affect the serum concentration of thromboxane B2 (TxB2) or the renal excretion of 11-dehydro-ThB2, a metabolite of thromboxane (both products of COX-1).
Celecoxib does not cause a decrease in glomerular filtration rate (GFR) in elderly patients and patients with chronic renal failure (CRF), and transiently reduces sodium excretion. In patients with arthritis, the incidence of peripheral edema, arterial hypertension and heart failure was comparable to that while taking non-selective COX inhibitors, which have inhibitory activity against COX-1 and COX-2. This effect was most pronounced in patients receiving diuretic therapy. However, there was no increase in the incidence of high blood pressure or heart failure, and peripheral edema was mild and self-limiting.
Pharmacokinetics
Suction
When taken on an empty stomach, celecoxib is well absorbed, reaching its maximum concentration (Cmax) in the blood plasma after approximately 2-3 hours. Cmax in blood plasma after taking 200 mg of celecoxib is 705 ng/ml. The absolute bioavailability of celecoxib has not been studied. Cmax and area under the concentration-time curve (AUC) are approximately proportional to the dose taken in the therapeutic dose range up to 200 mg twice daily; with higher doses of celecoxib, the degree of increase in Cmax and AUC occurs less proportionally.
Impact of food intake
Taking celecoxib concomitantly with a fatty meal increases the time to Cmax by approximately 4 hours and increases absorption by approximately 20%.
Distribution
The degree of binding to plasma proteins does not depend on the concentration of celecoxib in the blood plasma and is about 97%. Celecoxib does not bind to red blood cells. Celecoxib penetrates the blood-brain barrier.
Metabolism
Celecoxib is metabolized mainly with the participation of the cytochrome P450 (CYP) isoenzyme CYP2C9 in the liver through hydroxylation, oxidation and partially glucuronidation (see section “Interaction with other drugs”). The resulting metabolites are pharmacologically inactive against COX-1 and COX-2.
The activity of the CYP2C9 isoenzyme is reduced in patients with genetic polymorphisms, such as the polymorphism homozygous for the CYP2C9*3 isoenzyme, which leads to a decrease in the effectiveness of the enzymes.
Removal
Celecoxib is excreted through the intestines and kidneys in the form of metabolites (57% and 27%, respectively), less than 1% of the dose taken is unchanged. With repeated use, the half-life (T1/2) is 8-12 hours, and clearance is about 500 ml/min. With repeated use, equilibrium plasma concentrations are achieved by the 5th day of administration. The variability of the main pharmacokinetic parameters (AUC, Cmax, T1/2) is about 30%. The mean volume of distribution at steady state is approximately 500 L/70 kg in young healthy patients, indicating a wide tissue distribution of celecoxib.
Pharmacokinetics in selected patient groups
Elderly patients
In patients over 65 years of age, there is a 1.5-2-fold increase in the average Cmax and AUC values, which is largely due to changes in body weight rather than age (elderly patients tend to have a lower average body weight than younger people, due to which, other things being equal, they achieve higher concentrations of celecoxib). For the same reason, older women generally have higher plasma concentrations of celecoxib than older men. These pharmacokinetic features, as a rule, do not require dose adjustment. However, in elderly patients weighing less than 50 kg, treatment should be started at the minimum recommended dose.
Race
In blacks, the AUC of celecoxib is approximately 40% higher than in Caucasians. The reasons and clinical significance of this fact are unknown, therefore it is recommended to start treatment of people of the Negroid race with the minimum recommended dose.
Liver dysfunction
Plasma concentrations of celecoxib in patients with mild hepatic impairment (Child-Pugh class A) change slightly. In patients with moderate hepatic impairment (Child-Pugh class B), the plasma concentration of celecoxib may increase almost 2-fold.
Renal dysfunction
In elderly patients with a decrease in GFR > 65 ml/min/1.73 m2 associated with age-related changes, and in patients with a GFR equal to 35-60 ml/min/1.73 m2, the pharmacokinetics of celecoxib do not change. There is no significant correlation between serum creatinine concentration (or creatinine clearance (CC)) and celecoxib clearance. It is assumed that the presence of severe renal failure does not affect the clearance of celecoxib, since its main route of elimination is conversion to inactive metabolites in the liver.
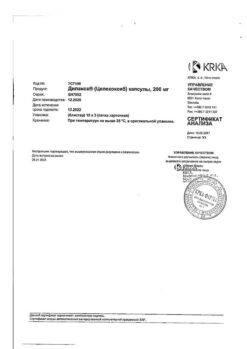
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C, in the original packaging.
Keep out of the reach of children.
Shelf life
Shelf life
2 years.
Do not use the drug after the expiration date.
Manufacturer
Manufacturer
KRKA dd Novo Mesto, Slovenia
Additional information
| Shelf life | 2 years. Do not use the product after the expiration date. |
|---|---|
| Conditions of storage | At temperature not exceeding 25°C, in original packaging. Store out of reach of children. |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | capsules |
| Brand | KRKA dd Novo mesto |
Other forms…
Related products
Buy Dilaxa, capsules 100 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.