No products in the cart.
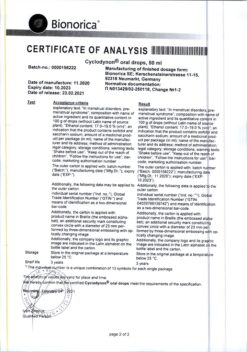
Diecyclene, 2 mg+0.03 mg 21 pcs
€20.28 €16.90
Description
Pharmaceutical group:
Contraceptive (estrogen+gestagen).
Pharmic action:
Diecyclene is a low-dose monophasic oral hormonal contraceptive. Contraceptive effect is based on the interaction of various factors, the most important of which is inhibition of ovulation and change of viscosity of cervical mucus, as a result of which it becomes impermeable for sperm, penetration of sperm through the cervical canal is difficult. If used correctly, the Perl Index (a measure of the number of pregnancies per 100 women using the contraceptive in a year) is less than 1. If the pill is missed or used incorrectly, the Perl Index may increase.
In addition to its contraceptive effect, it has other related positive properties. In women taking combined oral contraceptives, the cycle becomes more regular, the pain, intensity and duration of menstrual bleeding decrease, and as a result the risk of iron deficiency anemia decreases. There is also evidence of a decreased risk of endometrial and ovarian cancer.
The active gestagen component of the drug, dienogest, is a derivative of normestosterone with anti-androgenic activity and has a positive effect on the lipid profile by increasing high-density lipoprotein (HDL) concentrations.
Pharmacokinetics:
Ethinylestradiol:
When taken orally, it is rapidly and completely absorbed. The maximum concentration of estradiol in blood plasma (about 67 pg/ml) is reached after 1.5-4 hours. After absorption and the “first pass” effect through the liver, ethinylestradiol is metabolized, its absolute bioavailability with oral administration is about 44%.
Ethinylestradiol binds significantly to serum albumin (approximately 98%) and induces the synthesis of plasma sex hormone hormone binding globulin (hSPH). The volume of distribution of ethinylestradiol is about 2.8-8.6 L/kg.
Ethinylestradiol undergoes presystemic conjugation both in the mucosa of the small intestine and in the liver. The main metabolic pathway is aromatic hydroxylation with the formation of numerous hydroxylated and methylated derivatives in the form of free metabolites, glucuronide metabolites and sulfates. The blood plasma clearance rate is approximately 2.3-7 ml/min/kg.
Up to 30-50% of metabolites of ethinylsistrradiol a is excreted by the kidneys, 30-40% – through the intestine. Half-life of zestradiol (T1/2) does not exceed 10 hours after a single use of 1 tablet and increases to 15 hours after 3 cycles of the drug.
The equilibrium plasma concentration of ethinylsestradiol with regular use is reached in the second half of cyclic use of the drug.
Dienogest:
In oral administration, it is quickly and almost completely absorbed. The maximum concentration of dienogest in blood serum (about 51 pg/ml) is reached after 2.5 hours. Absolute bioavailability of dienogest is 96%, the equilibrium concentration in blood plasma is reached after 4 days with continuous administration.
90% of the total plasma concentration of dienogest is bound to serum albumin, but does not bind to hGH, or corticosteroid-binding globulin. Ten percent of the total plasma concentration of dienogest is unbound. The distribution volume of dienogest is about 37-45 liters.
It is metabolized mainly by hydroxylation, but also by hydrogenation, conjugation and aromatization with formation of inactive metabolites. After a single dose, the total clearance of dienogest is approximately 3.6 L/h.
After a dose of 0.1 mg/kg, the ratio of dienogest excretion as metabolites by the kidneys to the intestine is 3:1. Only a small amount of unchanged dienogest is excreted by the kidneys. The half-life (T1/2) of dienogest is approximately 8.5-10.8 hours. After oral administration 86% of the administered dose of dienogest is excreted within 6 days; a significant portion of it is excreted within the first 24 hours after administration mainly by the kidneys.
The equilibrium concentration. Induction of globulin synthesis by ethinylestradiol does not affect the pharmacokinetics of dienogest with daily use of the drug, the serum concentration of dienogest increases by 1.5 times.
Indications
Indications
— oral contraception;
– treatment of mild to moderate acne and seborrhea.
Pharmacological effect
Pharmacological effect
Pharmaceutical group:
contraceptive (estrogen + gestagen).
Pharmaceutical action:
The drug Diecyclen is a low-dose, monophasic oral hormonal contraceptive. The contraceptive effect is based on the interaction of various factors, the most important of which is inhibition of ovulation and a change in the viscosity of cervical mucus, as a result of which it becomes impermeable to sperm, and the penetration of sperm through the cervical canal is difficult. When used correctly, the Pearl index (an indicator reflecting the number of pregnancies in 100 women using a contraceptive during the year) is less than 1. If pills are missed or used incorrectly, the Pearl index may increase.
In addition to the contraceptive effect, it also has other associated positive properties. In women taking combined oral contraceptives, the cycle becomes more regular, the pain, intensity and duration of menstrual bleeding decreases, resulting in a reduced risk of iron deficiency anemia. There is also evidence of a reduced risk of endometrial and ovarian cancer.
The gestageic component dienogest, which is part of the drug, is an active gestagen, is a derivative of nortestosterone with antiandrogenic activity and has a positive effect on the lipoprotein profile, increasing the concentration of high-density lipoproteins (HDL).
Pharmacokinetics:
Ethinyl estradiol:
When taken orally, it is quickly and completely absorbed. The maximum concentration of estradol in the blood plasma (about 67 pg/ml) is achieved after 1.5-4 hours. After absorption and the “first pass” effect through the liver, ethinyl estradiol is metabolized, its absolute bioavailability when administered orally is about 44%.
Ethinyl estradiol binds significantly to serum albumin (approximately 98%) and induces the synthesis of sex hormone binding globulin (SHBG) in plasma. The volume of distribution of ethinyl estradiol is about 2.8-8.6 l/kg.
Ethinyl stradiol undergoes presystemic conjugation both in the mucous membrane of the small intestine and in the liver. The main route of metabolism is aromatic hydroxylation to form a variety of hydroxylated and methylated derivatives in the form of free metabolites, glucuronide metabolites and sulfates. The clearance rate from plasma is approximately 2.3-7 ml/min/kg.
Up to 30-50% of ethinyl stradiol metabolites are excreted by the kidneys, 30-40% through the intestines. The half-life of zstrradiol (T1/2) does not exceed 10 hours after a single dose of 1 tablet and increases to 15 hours after 3 cycles of taking the drug.
When taken regularly, the equilibrium concentration of ethinyl strradiol in the blood plasma is achieved in the second half of the cyclic dosing of the drug.
Dienogest:
When taken orally, it is quickly and almost completely absorbed. The maximum concentration of dienogest in the blood serum (about 51 pg/ml) is achieved after 2.5 hours. The absolute bioavailability of dienogest is 96%, the equilibrium concentration in the blood plasma with continuous use is achieved after 4 days.
90% of the total plasma concentration of dienogest is bound to serum albumin, but not to SHBG or corticosteroid binding globulin. 10% of the total concentration of dienogest in the blood plasma is found in unbound form. The volume of distribution of dienogest is about 37-45 liters.
Metabolized primarily by hydroxylation, but also by hydrogenation, conjugation and aromatization to form inactive metabolites. After taking a single dose, the total clearance of dienogest is approximately 3.6 l/h.
After taking a dose of 0.1 mg/kg, the ratio of dienogest excretion in the form of metabolites by the kidneys and through the intestines is 3:1. Only a small amount of unchanged dienogest is excreted by the kidneys. The half-life (T1/2) of dienogest is approximately 8.5-10.8 hours. After oral administration, 86% of the dose of dienogest is eliminated within 6 days; a significant part of it is excreted in the first 24 hours after administration, mainly by the kidneys.
Equilibrium concentration. Induction of globulin synthesis by ethinyl estradiol does not affect the pharmacokinetics of dienogest. With daily use of the drug, the concentration of dienogest in the serum increases by 1.5 times.
Special instructions
Special instructions
Irregular use can lead to acyclic bleeding and reduce the contraceptive effectiveness of the drug.
Before starting or resuming use of the drug, it is recommended to conduct a thorough general medical and gynecological examination (including examination of the mammary glands and cytological examination of scrapings from the cervix) and exclude pregnancy. In addition, disorders of the blood coagulation system should be excluded. When using the drug, it is necessary to carry out preventive control examinations at least once every 6 months.
The drug Diecyclen does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Diseases of the cardiovascular system:
Venous thromboembolism (VTE) may occur in the form of deep vein thrombosis and/or pulmonary embolism when using hormonal contraceptives. The estimated incidence of VTE in women taking oral contraceptives with low doses of estrogens (less than 50 mcg ethinyl estradiol) is up to 4 per 10 thousand women per year, compared with 0.5-3 per 10 thousand women not using oral contraceptives. However, the incidence of VTE developing when taking combined oral contraceptives is less than the incidence of VTE associated with pregnancy (6 per 10 thousand pregnant women per year).
In women taking combined oral contraceptives, extremely rare cases of thrombosis of other blood vessels, such as the hepatic, mesenteric, renal arteries and veins or retinal veins and arteries, have been described. The connection of these cases with the use of combined oral contraceptives has not been proven. A woman should stop taking the drug and consult a doctor if symptoms of venous or arterial thrombosis develop, which may include unilateral pain in the lower extremity and/or swelling; sudden severe chest pain; with or without irradiation to the left hand; sudden shortness of breath; sudden attacks of coughing; any unusual, severe, prolonged headache; increased frequency and severity of migraines; sudden partial or complete loss of vision; diplopia; slurred speech or aphasia; dizziness; collapse with or without partial seizure; weakness or very significant loss of sensation that suddenly appears on one side or in one part of the body; movement disorders; “sharp” stomach.
The risk of thrombosis (venous and/or arterial) and thromboembolism increases: with age, in smokers (with an increase in the number of cigarettes smoked or increasing age, the risk further increases, especially in women over 35 years of age), with a family history (i.e., venous or arterial thromboembolism ever in close relatives or parents at a relatively young age), obesity, dyslipoproteinemia, arterial hypertension, valve disease heart disease, prolonged immobilization, major surgery, any surgery on the lower extremities or major trauma, atrial fibrillation.
In case of prolonged immobilization, in case of major surgery, any leg surgery or major trauma, it is advisable to stop using the drug (in the case of planned surgery, at least 4 weeks before it) and not to resume use for 2 weeks after the end of immobilization.
The possible role of varicose veins and superficial thrombophlebitis in the development of venous thromboembolism remains controversial. The increased risk of thromboembolism in the postpartum period should be taken into account.
Microcirculatory disorders may also occur in diabetes mellitus, SLE, hemolytic uremic syndrome, Crohn’s disease, ulcerative colitis and sickle cell anemia.
Tumors:
The most significant risk factor for developing cervical cancer is persistent human papillomavirus infection. There are reports of a slight increase in the risk of developing cervical cancer with long-term use of combined oral contraceptives. However, the connection with the use of combined oral contraceptives has not been proven. The possibility of the relationship of these data with screening for cervical diseases and with characteristics of sexual behavior (less frequent use of barrier methods of contraception) is discussed.
A meta-analysis of 54 epidemiological studies found that there is a slightly increased relative risk of developing breast cancer diagnosed in women currently taking combined oral contraceptives (relative risk 1.24). The increased risk gradually disappears within 10 years of stopping these drugs. Because breast cancer is rare in women under 40 years of age, the increase in breast cancer diagnoses in women currently or recently taking combined oral contraceptives is small relative to the overall risk of breast cancer. The relationship between the development of breast cancer and the use of combined oral contraceptives has not been proven. The observed increased risk may also be a consequence of careful monitoring and earlier diagnosis of breast cancer in women using combined oral contraceptives. Women who have ever used combined oral contraceptives are diagnosed with earlier stages of breast cancer than women who have never used them.
In rare cases, during the use of combined oral contraceptives, the development of benign, and in extremely rare cases, malignant liver tumors, which in some cases led to life-threatening intra-abdominal bleeding, was observed. If severe abdominal pain, liver enlargement, or signs of intra-abdominal bleeding occur, this should be taken into account when making a differential diagnosis.
Other states:
Women with or a family history of hypertriglyceridemia may be at increased risk of developing pancreatitis when taking combined oral contraceptives.
Although slight increases in blood pressure (BP) have been described in many women taking combined oral contraceptives, clinically significant increases have been rare. The relationship between taking combined oral contraceptives and an increase in blood pressure has not been established. However, if persistent, clinically significant arterial hypertension develops while taking them, it is advisable to discontinue combined oral contraceptives and treat arterial hypertension. Taking combined oral contraceptives can be continued if normal blood pressure values are achieved with antihypertensive therapy.
Effect on the menstrual cycle:
During the use of combined oral contraceptives, irregular (acyclic) bleeding (“spotting” or “breakthrough” bleeding) may occur, especially during the first months of use. Therefore, any irregular bleeding should be assessed only after an adaptation period of approximately 3 cycles.
If irregular bleeding recurs or develops after previous regular cycles, careful evaluation should be performed to rule out malignancy or pregnancy.
Some women may not develop withdrawal bleeding while off the pill. If combined oral contraceptives were taken as directed, pregnancy is unlikely. However, if combined oral contraceptives were not taken regularly before, or if there are no two withdrawal bleedings in a row, then pregnancy must be excluded before continuing to take the drug.
Impact on laboratory test performance:
The use of oral combined contraceptive drugs may affect the results of some laboratory tests, including biochemical blood tests (indicators of liver, thyroid, kidney and adrenal function, concentrations of transport proteins in the blood plasma (such as SHBG), carbohydrate metabolism, lipid/lipoprotein fractions), as well as indicators of coagulation and fibrinolysis. However, changes in these indicators remain within normal values.
Impact on the ability to drive vehicles and machinery:
There is no data on the negative effect of the drug Diecyclen on the ability to drive vehicles and engage in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Dienogest, Ethinyl estradiol
Composition
Composition
1 tab.:
– ethinyl estradiol 0.03 mg
– dienogest 2 mg
Contraindications
Contraindications
– hypersensitivity to any of the components of the drug Diecyclen;
– thrombosis (venous and arterial) and thromboembolism currently or in history (including deep vein thrombosis, pulmonary embolism, myocardial infarction, stroke, cerebrovascular disorders);
– conditions preceding thrombosis (including transient ischemic attacks, angina) currently or in history;
– multiple or severe risk factors for venous or arterial thrombosis, including complicated lesions of the heart valve apparatus, atrial fibrillation, cerebral vascular disease or coronary artery disease; uncontrolled arterial hypertension, major surgery with prolonged immobilization, smoking over the age of 35 years, obesity with a body mass index > 30 kg/m2;
— diabetes mellitus with diabetic angiopathy;
– identified predisposition to venous or arterial thrombosis, including resistance to activated protein C, antithrombin III deficiency, protein C deficiency, protein S deficiency, hyperhomocysteinemia, antibodies to phospholipids, lupus antigen;
– severe liver diseases (until recovery and normalization of laboratory parameters of liver function);
– benign or malignant liver tumors, incl. history;
– severe forms of arterial hypertension with blood pressure >160/100 mmHg;
– identified or suspected hormone-dependent malignant diseases of the genital organs or mammary glands, incl. history;
– bleeding from the vagina of unknown origin;
– migraine with focal neurological symptoms currently or in history;
– pancreatitis, accompanied by severe hypertriglyceridemia at present or in history;
– severe and/or acute renal failure;
– pregnancy or suspicion of it;
– lactation period;
– hereditary lactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome or hypersensitivity to peanuts or soy (due to the presence of lactose and soy lecithin in Diecyclen).
With caution:
Risk factors for the development of thrombosis and thromboembolism: obesity, smoking, dyslipoproteinemia, arterial hypertension, migraine without focal neurological symptoms, heart valve defects, prolonged immobilization, major surgery, extensive trauma, hereditary predisposition to thrombosis (thrombosis, myocardial infarction or cerebrovascular accident at a young age in someone close to relatives).
Other diseases in which peripheral circulatory disorders may occur: diabetes mellitus without diabetic angiopathy, phlebitis of the superficial veins, systemic lupus erythematosus (SLE), hemolytic-uremic syndrome, Crohn’s disease, ulcerative colitis, sickle cell anemia.
Diseases that first appeared or worsened during pregnancy or during previous use of sex hormones, for example, jaundice and/or itching due to cholestasis, gallbladder disease, porphyria, Sydenham’s chorea, history of herpes during pregnancy, hearing impairment (associated with otosclerosis).
Endogenous depression, epilepsy; hereditary angioedema; hypertriglyceridemia; liver diseases; postpartum period.
Interaction
Interaction
Some drugs can increase the rate of metabolic clearance of sex hormones and lead to severe bleeding or a decrease in the contraceptive effect of the drug. Similar effects are typical for drugs that induce microsomal liver enzymes: hydantoin, barbiturates, primidone, carbamazepine and rifampicin. There are also suggestions regarding rifabutin, efavirenz, nevirapine, oxcarbazenin, topiramate, felbamate, ritonavir, nelvinafir, fiseofulvin, as well as drugs containing St. John’s wort (Hypericum perforatum).
Some antibiotics that reduce the enterohepatic circulation of estrogens (such as ampicillin or tetracycline) reduce the effectiveness of combined oral contraceptives.
Women taking short courses (maximum 1 week) of the above medications should use additional contraceptive measures (for example, a barrier method) during the period of concomitant use of the drugs and for the next 7 days.
When using oral contraceptives concomitantly with rifampicin, additional contraceptive measures (for example, a barrier method) should be used during the period of simultaneous use of the drugs and for the next 4 weeks after stopping treatment. If the package of oral contraceptives ends before the completion of the course of using other drugs, tablets from the next package of the drug should be taken without interruption.
The dose of contraceptives should be increased during a long-term course of treatment with drugs that induce microsomal liver enzymes. If side effects develop (for example, irregular menstruation) or the drug is ineffective, other non-hormonal contraceptives should be additionally used. Oral contraceptives may affect the metabolism of some other drugs. Accordingly, this may lead to an increase (cyclosporine) or decrease (lamotrigine) in their plasma or tissue concentrations.
Dienogest is a substrate of cytochrome P450 (CYP3A4). Known CYP3A4 inhibitors, such as antifungals (eg, ketoconazole), cimetidine, verapamil, macrolides (eg, erythromycin), diltiazem, antidepressants, and grapefruit juice, may increase dienogest plasma concentrations.
Overdose
Overdose
Possible symptoms of an overdose of Diecyclen: nausea, vomiting, irregular bleeding, absence of menstrual bleeding.
If necessary, symptomatic therapy is carried out.
Manufacturer
Manufacturer
Laboratorios Leon Pharma S.A., Spain
Additional information
| Manufacturer | Laboratorios Leon Pharma S.A., Spain |
|---|---|
| Medication form | pills |
| Brand | Laboratorios Leon Pharma S.A. |
Related products
Gynecology and Obstetrics
Gynecology and Obstetrics
Buy Diecyclene, 2 mg+0.03 mg 21 pcs with delivery to USA, UK, Europe and over 120 other countries.