No products in the cart.
Diclofenac-Solofarm, 25 mg/ml 3 ml 5 pcs
€4.19 €3.72
Description
Pharmacotherapeutic group
A nonsteroidal anti-inflammatory drug (NSAID).
ATX code: M01AB05
Pharmacological properties
Pharmacodynamics<
Diclofenac has anti-inflammatory, analgesic and antipyretic effects. Indiscriminately inhibiting cyclooxygenase 1 and 2, disrupts the metabolism of arachidonic acid, reduces the number of prostaglandins in the focus of inflammation. In rheumatic diseases anti-inflammatory and analgesic effect of diclofenac contributes to a significant reduction in the severity of pain, morning stiffness, joint swelling that improves the functional state of the joint. In trauma, in postoperative period diclofenac reduces pain and inflammatory swelling.
Pharmacokinetics
Absorption
After intramuscular administration of diclofenac its absorption begins immediately. The maximum plasma concentration (Cmax), averaging about 2.5 µg/mL (8 µmol/L), is reached after about 20 minutes. The amount of absorbed active ingredient is linearly related to the dose of the drug. The area under the curve “concentration-time” (AUC) after intramuscular diclofenac administration is approximately 2 times greater than after its oral or rectal administration, because in the latter cases, about half of diclofenac is metabolized during the “first passage” through the liver. Pharmacokinetic parameters do not change during subsequent administration of the drug. No cumulation is noted if the recommended intervals between doses of the drug are observed.
Distribution
The binding to serum proteins is 99.7%, mostly to albumin (99.4%). The apparent volume of distribution is 0.12-0.17 l/kg. Diclofenac penetrates into the synovial fluid, where its maximum concentration is reached 2-4 hours later than in blood plasma. The apparent half-life (T½) from synovial fluid is 3-6 hours. Two hours after reaching maximum plasma concentration, the concentration of diclofenac in synovial fluid is higher than in plasma, and its values remain higher for up to 12 hours.
Metabolism
. Diclofenac is metabolized partly by glucuronidation of the unchanged molecule, but mainly by single and multiple hydroxylation and methoxylation, resulting in several phenolic metabolites (3′-hydroxy-, 4′-hydroxy-, 5′-hydroxy-, 4′,5-dihydroxy- and 3′-hydroxy-4′-methoxydiclofenac), most of which are converted to glucuronide conjugates. The two phenolic metabolites are biologically active, but to a much lesser extent than diclofenac. The CYP2C9 isoenzyme is involved in metabolism of the drug.
The total systemic plasma clearance of diclofenac is 263 ± 56 ml/min. The final T½ is 1-2 hours. The T½ of the 4 metabolites, including the two pharmacologically active ones, is similarly short and is 1-3 hours. One of the metabolites, 3′-hydroxy-4′-methoxydiclofenac, has a longer T½, but this metabolite is completely inactive. About 60% of the drug dose is excreted through the kidneys as glucuron conjugates of the unchanged active substance, as well as metabolites, most of which are also glucuron conjugates. Less than 1% of diclofenac is excreted unchanged. The remaining part of the drug dose is excreted as metabolites in the bile.
Pharmacokinetics in individual groups of patients
Pharmacokinetic parameters of diclofenac do not change in elderly patients. In patients with impaired renal function there is no cumulation of unchanged active substance while following the recommended dosing regimen. When creatinine clearance is less than 10 ml/min, calculated equilibrium concentrations of diclofenac hydroxymetabolites are about 4 times higher than in healthy volunteers, and metabolites are excreted only with bile. In patients with chronic hepatitis or compensated liver cirrhosis pharmacokinetic parameters of diclofenac are similar to those of patients without liver disease. Diclofenac penetrates into breast milk.
Indications
Indications
For short-term treatment of pain of various origins, moderate intensity:
diseases of the musculoskeletal system (rheumatoid arthritis, psoriatic, juvenile chronic arthritis, ankylosing spondylitis; gouty arthritis, rheumatic soft tissue disease, osteoarthritis of peripheral joints and spine (including radicular syndrome);
lumbago, sciatica, neuralgia;
algodismenorrhea, inflammatory processes of the pelvic organs, incl. adnexitis;
post-traumatic pain syndrome accompanied by inflammation;
postoperative pain.
The drug is intended for symptomatic therapy, reducing pain and inflammation at the time of use, and does not affect the progression of the disease.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Non-steroidal anti-inflammatory drug (NSAID).
ATX code: М01АВ05
Pharmacological properties
Pharmacodynamics
Diclofenac has anti-inflammatory, analgesic and antipyretic effects. By indiscriminately inhibiting cyclooxygenase 1 and 2, it disrupts the metabolism of arachidonic acid and reduces the amount of prostaglandins at the site of inflammation. In rheumatic diseases, the anti-inflammatory and analgesic effect of diclofenac helps to significantly reduce the severity of pain, morning stiffness, and swelling of the joints, which improves the functional state of the joint. For injuries, in the postoperative period, diclofenac reduces pain and inflammatory swelling.
Pharmacokinetics
Suction
After intramuscular administration of diclofenac, its absorption begins immediately. The maximum plasma concentration (Cmax), the average value of which is about 2.5 μg/ml (8 μmol/l), is reached after approximately 20 minutes. The amount of absorbed active substance is linearly dependent on the dose of the drug. The area under the concentration-time curve (AUC) after intramuscular administration of diclofenac is approximately 2 times greater than after its oral or rectal administration, since in the latter cases, about half of the amount of diclofenac is metabolized during the “first pass” through the liver. With subsequent administrations of the drug, the pharmacokinetic parameters do not change. Provided that the recommended intervals between administrations of the drug are observed, no accumulation is observed.
Distribution
Communication with serum proteins is 99.7%, mainly with albumin (99.4%). The apparent volume of distribution is 0.12-0.17 l/kg. Diclofenac penetrates into the synovial fluid, where its maximum concentration is reached 2-4 hours later than in the blood plasma. The apparent half-life (T½) from synovial fluid is 3-6 hours. 2 hours after reaching the maximum concentration in the blood plasma, the concentration of diclofenac in the synovial fluid is higher than in the plasma, and its values remain higher over a period of time up to 12 hours.
Metabolism
The metabolism of diclofenac is carried out partly by glucuronidation of the unchanged molecule, but mainly through single and multiple hydroxylation and methoxylation, which leads to the formation of several phenolic metabolites (3′-hydroxy-, 4′-hydroxy-, 5′-hydroxy-, 4′,5-dihydroxy- and 3′-hydroxy-4′-methoxydiclofenac), the majority from which it is converted into glucuronide conjugates. Two phenolic metabolites are biologically active, but to a much lesser extent than diclofenac. The CYP2C9 isoenzyme takes part in the metabolism of the drug.
Removal
The total systemic plasma clearance of diclofenac is 263 ± 56 ml/min. The final T½ is 1-2 hours. T½ of 4 metabolites, including two pharmacologically active ones, is also short-lived and lasts 1-3 hours. One of the metabolites, 3′-hydroxy-4′-methoxydiclofenac, has a longer half-life, but this metabolite is completely inactive. About 60% of the drug dose is excreted through the kidneys in the form of glucuronic conjugates of the unchanged active substance, as well as in the form of metabolites, most of which are also glucuronic conjugates. Less than 1% of diclofenac is excreted unchanged. The remainder of the drug dose is excreted in the form of metabolites in bile.
Pharmacokinetics in selected patient groups
The pharmacokinetic parameters of diclofenac in elderly patients do not change. In patients with impaired renal function, accumulation of unchanged active substance is not observed if the recommended dosage regimen is observed. When creatinine clearance is less than 10 ml/min, the calculated equilibrium concentrations of diclofenac hydroxymetabolites are approximately 4 times higher than in healthy volunteers, while the metabolites are excreted exclusively in bile. In patients with chronic hepatitis or compensated liver cirrhosis, the pharmacokinetics of diclofenac are similar to those in patients without liver disease. Diclofenac passes into breast milk.
Special instructions
Special instructions
To reduce the risk of adverse events, the minimum effective dose of diclofenac should be used for the shortest possible course. Long-term therapy with diclofenac and therapy using high doses may lead to an increased risk of developing serious cardiovascular thrombotic complications (including myocardial infarction and stroke).
Impact on the ability to drive vehicles and machinery
Patients suffering from dizziness and other disorders of the central nervous system should refrain from driving and operating dangerous machinery during the treatment period.
Active ingredient
Active ingredient
Diclofenac
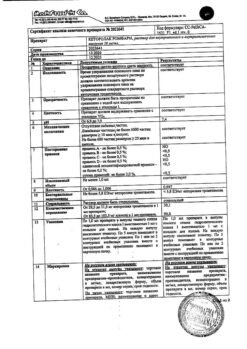
Composition
Composition
Composition of the drug per 1 ml
Active substance:
Diclofenac sodium – 25 mg
Excipients:
Mannitol – 6 mg
Propylene glycol – 200 mg
Benzyl alcohol – 40 mg
Sodium disulfite – 0.6 mg
Sodium hydroxide solution 1 M – to pH 7.8-8.8
Water for injections – up to 1 ml
Pregnancy
Pregnancy
The drug is contraindicated during pregnancy (see section “Contraindications”). There is no information on the use of Diclofenac during pregnancy. Diclofenac should not be taken during breastfeeding (see section “Contraindications”). Diclofenac passes into breast milk.
Contraindications
Contraindications
Hypersensitivity (including to other NSAIDs or auxiliary components), erosive and ulcerative lesions of the gastrointestinal tract (in the acute phase), bleeding from the gastrointestinal tract, inflammatory bowel diseases, severe liver failure, liver disease in the acute period, severe renal failure (creatinine clearance less than 30 ml/min), hyperkalemia, complete or incomplete syndrome intolerance to acetylsalicylic acid (rhinosinusitis, urticaria, polyps of the nasal mucosa, bronchial asthma that occurs when taking acetylsalicylic acid or other NSAIDs), hematopoietic disorders, hemostasis disorders (including hemophilia), pregnancy, childhood (up to 18 years), lactation period, the period after coronary artery bypass grafting, with an increased risk of arterial thrombosis and thromboembolism, clinically confirmed coronary heart disease, diseases of peripheral arteries and cerebral vessels, chronic heart failure, functional class II-IV according to the NYHA classification, uncontrolled arterial hypertension.
With caution
Edema syndrome, peripheral arterial diseases, dyslipidemia, diabetes mellitus, anemia, bronchial asthma, defects in the hemostatic system, with a risk of cardiovascular thrombosis (including myocardial infarction and stroke), renal failure (creatinine clearance 30-60 ml/min), alcoholism, erosive and ulcerative diseases of the gastrointestinal tract without exacerbation, Helicobacter pylori infection, diverticulitis, condition after major surgery, inducible porphyria, old age, smoking, severe somatic diseases, systemic connective tissue diseases, long-term use of non-steroidal anti-inflammatory drugs.
Caution should be exercised when used in patients with seasonal allergic rhinitis, swelling of the nasal mucosa (including nasal polyps), chronic infectious diseases of the respiratory tract (especially those associated with allergic rhinitis-like symptoms). Particular caution should be exercised when using diclofenac in patients receiving drugs that increase the risk of gastrointestinal bleeding: systemic glucocorticosteroids (including prednisolone), anticoagulants (including warfarin), antiplatelet agents (including acetylsalicylic acid, clopidogrel) or selective serotonin reuptake inhibitors (including citalopram, fluoxetine, paroxetine, sertraline).
Side Effects
Side Effects
To assess the frequency of adverse reactions of diclofenac (various dosage forms), the following gradations were used: “very often” > 1/10; “common” from >1/100 to 1/1000 to 1/10000 to <1/1000, “very rare” from <1/10000, including isolated reports.
From the gastrointestinal tract: Often – epigastric pain, nausea, vomiting, diarrhea, dyspepsia, flatulence, anorexia, increased aminotransferase activity; rarely – gastritis, proctitis, bleeding from the gastrointestinal tract (gastrointestinal tract) (vomiting with blood, melena, diarrhea mixed with blood), gastrointestinal ulcers (with or without bleeding or perforation), hepatitis, jaundice, impaired liver function; very rarely – stomatitis, glossitis, esophagitis, nonspecific hemorrhagic colitis, exacerbation of ulcerative colitis or Crohn’s disease, constipation, pancreatitis, fulminant hepatitis, hepatorenal syndrome.
From the nervous system: Often – headache, dizziness; rarely – drowsiness; very rarely – sensory disturbances (including paresthesia), memory disorders, tremors, convulsions, anxiety, cerebrovascular disorders, aseptic meningitis, disorientation, depression, insomnia, nightmares, irritability, mental disorders.
From the senses: Often – vertigo; very rarely – visual impairment (blurred visual perception, diplopia), hearing impairment, tinnitus, impaired taste.
From the skin: Often – skin rash; rarely – urticaria; very rarely – bullous rashes, erythema, including multiforme and Stevens-Johnson syndrome, Lyell’s syndrome, exfoliative dermatitis, itching, hair loss, photosensitivity, purpura, including allergic.
From the genitourinary system: Very rarely – acute renal failure, hematuria, proteinuria, interstitial nephritis, nephrotic syndrome, papillary necrosis. From the hematopoietic organs: Very rarely – thrombocytopenia, leukopenia, hemolytic and aplastic anemia, agranulocytosis, eosinophilia.
From the respiratory system: Rarely – bronchial asthma (including shortness of breath), cough, laryngeal edema; very rarely – pneumonitis.
From the cardiovascular system: Very rarely – palpitations, chest pain, increased blood pressure, vasculitis, heart failure, myocardial infarction. Allergic manifestations: Rarely – anaphylactic/anaphylactoid reactions, including a marked decrease in blood pressure and shock; very rarely – angioedema (including the face).
Other: Often – irritation at the injection site; very rarely – abscess at the injection site; rarely – swelling.
Interaction
Interaction
Increases plasma concentrations of digoxin, methotrexate, lithium and cyclosporine. Reduces the effect of diuretics; against the background of potassium-sparing diuretics, it increases the risk of hyperkalemia; against the background of anticoagulants, thrombolytic agents (alteplase, streptokinase, urokinase) – the risk of bleeding (usually from the gastrointestinal tract). Reduces the effects of antihypertensive and hypnotic drugs.
Increases the likelihood of side effects of other nonsteroidal anti-inflammatory drugs and glucocorticosteroids (bleeding in the gastrointestinal tract), methotrexate toxicity and cyclosporine nephrotoxicity. Acetylsalicylic acid reduces the concentration of diclofenac in the blood.
Concomitant use with paracetamol increases the risk of developing nephrotoxic effects of diclofenac. Reduces the effect of hypoglycemic drugs. Cefamandole, cefoperazone, cefotetan, valproic acid and plicamycin increase the incidence of hypoprothrombinemia. Cyclosporine and gold preparations increase the effect of diclofenac on the synthesis of prostaglandins in the kidneys, which increases nephrotoxicity.
Simultaneous administration with ethanol, colchicine, corticotropin, selective serotonin reuptake inhibitors and St. John’s wort preparations increases the risk of bleeding in the gastrointestinal tract. Diclofenac enhances the effect of drugs that cause photosensitivity. Drugs that block tubular secretion increase plasma concentrations of diclofenac, thereby increasing its toxicity. Diclofenac has an antiprostaglandin effect, so it is not recommended to take diclofenac within 8-12 days after using mifepristone.
Overdose
Overdose
Symptoms: Vomiting, dizziness, headache, shortness of breath, clouding of consciousness, in children – myoclonic convulsions, nausea, vomiting, abdominal pain, bleeding, impaired liver and kidney function, respiratory depression, coma.
Treatment: Symptomatic therapy, forced diuresis. Hemodialysis is ineffective.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C. Keep out of the reach of children.
Shelf life
Shelf life
2 years. Do not use after the expiration date!
Manufacturer
Manufacturer
Grotex LLC, Russia
Additional information
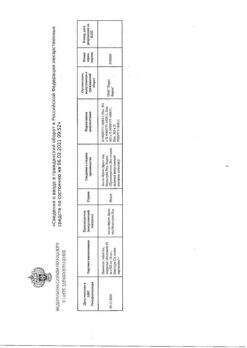
| Shelf life | 2 years. Do not use after the expiration date! |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C. Keep out of reach of children. |
| Manufacturer | Grotex Ltd, Russia |
| Medication form | solution |
| Brand | Grotex Ltd |
Other forms…
Related products
Buy Diclofenac-Solofarm, 25 mg/ml 3 ml 5 pcs with delivery to USA, UK, Europe and over 120 other countries.