No products in the cart.
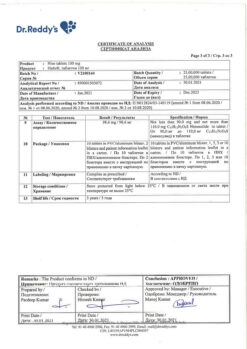
Diclofenac, 25 mg/ml 3 ml 10 pcs
€6.49 €5.68
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: Non-steroidal anti-inflammatory drug (NSAID).
The ATC code: M01AB05
Pharmacological properties
Pharmacodynamics
Diclofenac Velfarm contains diclofenac sodium, a substance of non-steroidal structure with pronounced anti-inflammatory, analgesic and antipyretic effect.
The main mechanism of action of diclofenac, established in studies, is considered to be inhibition of prostaglandin biosynthesis. Prostaglandins play an important role in the genesis of inflammation, pain and fever.
In vitro diclofenac sodium in concentrations equivalent to those achieved with human use does not inhibit cartilage proteoglycan biosynthesis.
In rheumatic diseases, the anti-inflammatory and analgesic properties of the drug provide a clinical effect characterized by a significant reduction of manifestations such as pain at rest and on movement, morning stiffness and joint swelling, as well as improvement of functional status.
In posttraumatic and postoperative inflammatory phenomena diclofenac quickly relieves pain (both at rest and on the move), reduces inflammatory edema and swelling of the postoperative wound.
The pronounced analgesic effect of diclofenac in moderate to severe pain was noted
of non-rheumatic origin. Pain relief comes in 15-30 minutes. In addition, diclofenac relieves migraine attacks.
When used in combination with opioids in patients with postoperative pain, diclofenac significantly reduces the need for opioid analgesics.
Pharmacokinetics
Absorption
After intramuscular (I/M) administration of 75 mg diclofenac its absorption begins immediately. The maximum plasma concentration (Cmax), which averages about 2.5 µg/mL (8 µmol/L), is reached after about 20 minutes. The amount of absorbed active ingredient is linearly related to the dose amount of the drug.
The magnitude of the area under the curve “concentration-time” (AUC) after diclofenac injection is approximately twice as large as after its oral or rectal administration, because in the latter cases about half of diclofenac is metabolized during the “first passage” through the liver.
The pharmacokinetic parameters do not change with subsequent administration. No cumulation is observed if the recommended intervals between diclofenac administration are observed.
Distribution
The binding to serum proteins is 99.7%, predominantly to albumin (99.4%). Apparent volume of distribution is 0.12-0.17 l/kg.
Diclofenac penetrates into the synovial fluid, where its maximum concentration is reached 2-4 hours later than in the blood plasma. The elimination half-life from synovial fluid is 3-6 hours. In 2 hours after reaching the maximum concentration in plasma, the concentration of diclofenac in synovial fluid is higher than in blood plasma, and its values remain higher for up to 12 hours.
Diclofenac was detected in low concentrations (100 ng/ml) in the breast milk of one nursing mother. The estimated amount of diclofenac absorbed through breast milk into the baby is equivalent to 0.03 mg/kg/day.
Metabolism
. Diclofenac is metabolized partly by glucuronidation of the unchanged molecule, but predominantly by single and multiple hydroxylation and methoxylation, resulting in several phenolic metabolites (3′-hydroxy-, 4′-hydroxy-, 5′-hydroxy-, 4′,5-dihydroxy- and 3′-hydroxy-4′-metoxydiclofenac),
most of which are converted to glucuron conjugates. Two phenolic metabolites are biologically active, but to a much lesser extent than diclofenac.
The total systemic plasma clearance of diclofenac is 263 ± 56 ml/min. Final elimination half-life is 1-2 hours. The half-life of 4 metabolites, including two pharmacologically active ones, is also short and is 1-3 hours. One of the metabolites, 3′-hydroxy-4′-methoxydiclofenac, has a longer half-life, but this metabolite is completely inactive.
About 60% of diclofenac dose is excreted by the kidneys as glucuron conjugates of the unchanged active substance, and as metabolites, most of which are also glucuron conjugates. Less than 1% of diclofenac is excreted unchanged. The remaining part of diclofenac is excreted as metabolites in the bile.
The concentration of diclofenac in plasma is linearly dependent on the dose used.
Pharmacokinetics in special groups of patients
The absorption, metabolism and excretion of diclofenac are independent of age. In children the concentrations of diclofenac in plasma when using equivalent doses of the drug (mg/kg body weight) are similar to those in adults. But in some elderly patients after 15-min intravenous infusion an increase of diclofenac plasma concentration by 50% was noted in comparison with such index in healthy volunteers of younger age.
In patients with impaired renal function, there is no cumulation of the unchanged active substance while following the recommended dosing regimen.
In patients with a creatinine clearance of less than 10 ml/min, the calculated equilibrium concentrations of diclofenac hydroxymetabolites are approximately 4 times higher than in healthy volunteers, and the metabolites are excreted exclusively in the bile.
In patients with chronic hepatitis or compensated cirrhosis the pharmacokinetics of diclofenac are similar to those of patients without liver disease.
Indications
Indications
Inflammatory and degenerative diseases of the musculoskeletal system including:
– rheumatoid arthritis,
– ankylosing spondylitis and other spondyloarthropathy,
– osteoarthritis,
– gouty arthritis,
– bursitis, tendovaginitis,
– pain syndromes from the spine (lumbago, sciatica, ossalgia, neuralgia, myalgia, arthralgia, radiculitis). Renal and biliary colic.
Post-traumatic and postoperative pain syndrome accompanied by inflammation. Severe migraine attacks.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: non-steroidal anti-inflammatory drug (NSAID).
ATX code: М01АВ05
Pharmacological properties
Pharmacodynamics
The drug Diclofenac Velpharm contains diclofenac sodium, a non-steroidal substance that has a pronounced anti-inflammatory, analgesic and antipyretic effect.
The main mechanism of action of diclofenac, established in studies, is considered to be inhibition of prostaglandin biosynthesis. Prostaglandins play an important role in the genesis of inflammation, pain and fever.
In vitro, diclofenac sodium in concentrations equivalent to those achieved when used in humans does not inhibit the biosynthesis of proteoglycans in cartilage tissue.
In rheumatic diseases, the anti-inflammatory and analgesic properties of the drug provide a clinical effect, characterized by a significant decrease in the severity of such manifestations as pain at rest and during movement, morning stiffness and swelling of the joints, as well as an improvement in the functional state.
In case of post-traumatic and postoperative inflammatory phenomena, diclofenac quickly relieves pain (both at rest and during movement), reduces inflammatory swelling and swelling of the postoperative wound.
A pronounced analgesic effect of diclofenac was noted for moderate and severe pain
non-rheumatic origin. Pain relief occurs within 15-30 minutes. In addition, diclofenac relieves migraine attacks.
When used in combination with opioids in patients with postoperative pain, diclofenac significantly reduces the need for opioid analgesics.
Pharmacokinetics
Special instructions
Special instructions
Damage to the gastrointestinal tract
When using diclofenac, phenomena such as bleeding or ulceration/perforation of the gastrointestinal tract, in some cases with fatal outcome, were observed. These events may occur at any time when using drugs in patients with or without previous symptoms and a history of serious gastrointestinal diseases. In older patients, such complications can have serious consequences. If bleeding or gastrointestinal ulceration develops in patients receiving Diclofenac Velpharm, the drug should be discontinued.
To reduce the risk of toxic effects on the gastrointestinal tract, patients with gastrointestinal ulcers, especially those complicated by bleeding or a history of perforation, as well as in elderly patients, the drug should be used in the minimum effective dose. Patients at increased risk of developing gastrointestinal complications, as well as patients receiving low-dose acetylsalicylic acid therapy, should take gastroprotectors (proton pump inhibitors or misoprostol) or other medications to reduce the risk of unwanted effects on the gastrointestinal tract. Patients with a history of gastrointestinal lesions, especially the elderly, should report all abdominal symptoms to the doctor.
Patients with bronchial asthma
Exacerbation of asthma (NSAID intolerance/NSAID-induced asthma), angioedema and urticaria are most often observed in patients with asthma, seasonal allergic rhinitis, nasal polyps, chronic obstructive pulmonary disease or chronic respiratory infections (especially those associated with allergic rhinitis-like symptoms). In this group of patients, as well as in patients with allergies to other drugs (rash, itching or urticaria), special care should be taken when using Diclofenac Velpharm (preparedness for resuscitation measures).
Skin reactions
Serious dermatological reactions such as exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis, in some cases fatal, have been reported very rarely with the use of diclofenac. The highest risk and incidence of severe dermatological reactions were observed in the first month of treatment with diclofenac. If patients receiving Diclofenac Velpharm develop the first signs of skin rash, damage to the mucous membranes or other symptoms of hypersensitivity, the drug should be discontinued.
In rare cases, in patients who are not allergic to diclofenac, anaphylactic/anaphylactoid reactions may develop when using Diclofenac Velpharm.
Effects on the liver
Since during the period of use of the drug Diclofenac Velpharm there may be an increase in the activity of one or more liver enzymes, during long-term therapy with the drug, monitoring of liver function is indicated as a precaution. If liver dysfunction persists or progresses or signs of liver disease or other symptoms (for example, eosinophilia, rash, etc.) occur, the drug should be discontinued. It should be borne in mind that hepatitis during the use of the drug Diclofenac Velpharm can develop without prodromal phenomena.
Effects on the kidneys
During therapy with Diclofenac Velpharm, it is recommended to monitor renal function in patients with hypertension, impaired cardiac or renal function, the elderly, patients receiving diuretics or other drugs that affect renal function, as well as in patients with a significant decrease in the volume of circulating blood plasma of any etiology, for example, during the period before and after major surgical interventions. After discontinuation of drug therapy, normalization of renal function indicators to initial values is usually observed.
Effects on the cardiovascular system
Therapy with NSAIDs, including diclofenac, particularly long-term and high-dose therapy, may be associated with a small increased risk of serious cardiovascular thrombotic events (including myocardial infarction and stroke).
In patients with diseases of the cardiovascular system and a high risk of developing diseases of the cardiovascular system (for example, with arterial hypertension, hyperlipidemia, diabetes mellitus, smokers), the drug should be used with extreme caution, at the lowest effective dose for the shortest possible duration of treatment, since the risk of thrombotic complications increases with increasing dose and duration of treatment. With long-term therapy (more than 4 weeks), the daily dose of diclofenac in such patients should not exceed 100 mg. The effectiveness of treatment and the patient’s need for symptomatic therapy should be periodically assessed, especially in cases where its duration is more than 4 weeks. The patient should be instructed to seek immediate medical attention if the first symptoms of thrombotic disorders (eg, chest pain, shortness of breath, weakness, speech disturbances) appear.
Impact on the hematopoietic system
The drug Diclofenac Velpharm may temporarily inhibit platelet aggregation. Therefore, in patients with hemostasis disorders, it is necessary to carefully monitor relevant laboratory parameters.
With long-term use of the drug Diclofenac Velpharm, it is recommended to conduct regular clinical tests of peripheral blood.
Masking signs of an infectious process
The anti-inflammatory effect of Diclofenac Velpharm may complicate the diagnosis of infectious processes.
Use simultaneously with other NSAIDs
Diclofenac Velpharm should not be used concomitantly with other NSAIDs, including selective COX-2 inhibitors, due to the risk of increased adverse events.
Impact on the ability to drive vehicles and machinery
Patients who experience visual disturbances, dizziness, drowsiness, vertigo or other central nervous system disorders while using Diclofenac Velpharm should not drive vehicles or operate machinery.
Active ingredient
Active ingredient
Diclofenac
Composition
Composition
For 1 ml:
Active ingredient: diclofenac sodium – 25 mg.
Excipients: benzyl alcohol, propylene glycol, mannitol (mannitol), sodium disulfite (sodium metabisulfite), sodium hydroxide solution 1 M, water for injection.
Pregnancy
Pregnancy
There is insufficient data on the safety of diclofenac in pregnant women, and therefore Diclofenac Velpharm should be used in the first and second trimesters of pregnancy only in cases where the expected benefit to the mother outweighs the potential risk to the fetus. Diclofenac, like other NSAIDs (prostaglandin synthesis inhibitors), is contraindicated in the last 3 months of pregnancy (possible suppression of uterine contractility, impaired renal function in the fetus with subsequent oligohydramnios (oligohydroamnion) and/or premature closure of the ductus arteriosus in the fetus).
Despite the fact that diclofenac, like other NSAIDs, passes into breast milk in small quantities, the drug should not be used during breastfeeding to avoid undesirable effects on the baby. If it is necessary to use the drug in a woman during this period, breastfeeding is stopped.
Since diclofenac, like other NSAIDs, can have a negative effect on fertility, women planning pregnancy are not recommended to use the drug. For patients undergoing examination and treatment for infertility, the drug should be discontinued.
Contraindications
Contraindications
– Exacerbation of gastric and duodenal ulcers, bleeding from the gastrointestinal tract (GIT), perforation of the GIT organs.
– Hypersensitivity to diclofenac and any other components of the drug (including sodium disulfite).
– III trimester of pregnancy.
– Like other NSAIDs, Diclofenac Velpharm is contraindicated in patients with a complete or incomplete combination of bronchial asthma, recurrent nasal or paranasal sinus polyposis and intolerance to acetylsalicylic acid or other non-steroidal anti-inflammatory drugs (including a history).
– Severe liver dysfunction, renal failure (GFR less than 15 ml/min/1.73 m2), chronic heart failure (II-IV functional class according to the NYHA classification).
– Clinically confirmed coronary heart disease.
– Diseases of peripheral arteries and cerebral vessels.
– Uncontrolled arterial hypertension.
– Conditions accompanied by a risk of bleeding.
– Confirmed hyperkalemia.
– Coronary artery bypass grafting (perioperative period).
– Inflammatory bowel diseases (Crohn’s disease, ulcerative colitis) in the acute phase.
– Active liver diseases.
– Breastfeeding period.
The drug Diclofenac Velpharm, a solution for intramuscular administration, is not indicated for use in children and adolescents under 18 years of age.
With caution
When using the drug Diclofenac Velpharm and other NSAIDs, it is necessary to exercise caution and carefully monitor patients with symptoms/signs indicating lesions/diseases of the gastrointestinal tract or with medical history that allows one to suspect ulcerative lesions of the stomach or intestines, bleeding or perforation; in patients with a history of Helicobacter pylori infection, ulcerative colitis, Crohn’s disease, with a history of liver dysfunction, and in patients with complaints suggestive of disease
Gastrointestinal tract. The risk of developing gastrointestinal bleeding increases with increasing doses of NSAIDs or with a history of ulcers, especially bleeding and perforation of the ulcer and in elderly patients. Particular caution should be exercised when using Diclofenac Velpharm in patients receiving drugs that increase the risk of gastrointestinal bleeding: systemic glucocorticosteroids (including prednisolone), anticoagulants (including warfarin), antiplatelet agents (including clopidogrel, acetylsalicylic acid) or selective serotonin reuptake inhibitors (including citalopram, fluoxetine, paroxetine, sertraline).
Caution is required when using Diclofenac Velpharm in patients with mild to moderate liver dysfunction, as well as in patients with hepatic porphyria, since the drug can provoke attacks of porphyria.
The drug should be used with caution in patients with bronchial asthma, seasonal allergic rhinitis, swelling of the nasal mucosa (including nasal polyps), chronic obstructive pulmonary disease, chronic infectious diseases of the respiratory tract (especially those associated with allergic rhinitis-like symptoms).
Particular caution is required when treating patients with cardiovascular diseases, impaired renal function, including chronic renal failure (GFR 15-60 ml/min/1.73 m2), dyslipidemia/hyperlipidemia, diabetes mellitus, hypertension, when treating patients who smoke or drink alcohol, when treating elderly patients receiving diuretics or other drugs that affect renal function, as well as patients with significant decrease in circulating blood volume (CBV) of any etiology, for example, in the periods before and after major surgical interventions.
Diclofenac Velpharm should be used with caution in patients with defects in the hemostatic system. Caution should be exercised when using Diclofenac Velpharm in patients at risk of developing cardiovascular thrombosis.
Caution should be exercised when using Diclofenac Velpharm in elderly patients. This is especially true in frail or low-weight elderly people. In patients in this category, it is recommended to use the drug in the minimum effective dose.
Particular caution should be observed when administering Diclofenac Velpharm intramuscularly in patients with bronchial asthma due to the risk of exacerbation of the disease, since sodium disulfite contained in the drug can cause severe hypersensitivity reactions.
Side Effects
Side Effects
Below are the adverse events (AEs) that were identified during clinical trials, as well as when using diclofenac in clinical practice.
To assess the frequency of AEs, the following criteria were used: “very often” (> 1/10); “often” (> 1/100, 1/1000, 1/10000, < 1/1000); “very rare” (< 1/10000).
AEs are grouped in accordance with the system-organ class of the medical dictionary for regulatory activities MedDRA, within each class AEs are listed in descending order of frequency of occurrence; Within each group, identified by frequency of occurrence, AEs are distributed in decreasing order of their importance.
Infectious and parasitic diseases: very rarely – post-injection abscess. Disorders of the blood and lymphatic system: very rarely – thrombocytopenia, leukopenia, hemolytic anemia, aplastic anemia, agranulocytosis.
Immune system disorders: rarely – hypersensitivity, anaphylactic/anaphylactoid reactions, including decreased blood pressure (BP) and shock; very rarely – angioedema (including facial swelling).
Mental disorders: very rarely – disorientation, depression, insomnia, nightmares, irritability, mental disorders.
Nervous system disorders: often – headache, dizziness; rarely – drowsiness; very rarely – sensitivity disorders, including paresthesia, memory disorders, tremors, convulsions, anxiety, acute cerebrovascular accidents, aseptic meningitis.
Visual disturbances: very rarely – visual disturbances (blurred vision), diplopia.
Hearing and labyrinthine disorders: often – vertigo; very rarely – hearing impairment, tinnitus.
Cardiac disorders: uncommon – myocardial infarction, heart failure, palpitations, chest pain.
Vascular disorders: very rarely – increased blood pressure, vasculitis.
Disorders of the respiratory system, chest and mediastinal organs: rarely –
bronchial asthma (including shortness of breath); very rarely – pneumonitis.
Gastrointestinal disorders: often – abdominal pain, nausea, vomiting, diarrhea, dyspepsia, flatulence, loss of appetite; rarely – gastritis, gastrointestinal bleeding, vomiting blood, melena, diarrhea mixed with blood, gastric and intestinal ulcers (with or without bleeding, stenosis or perforation, with the possible development of peritonitis); very rarely – stomatitis, glossitis, damage to the esophagus, the occurrence of diaphragm-like strictures in the intestine, colitis (nonspecific hemorrhagic colitis, ischemic colitis, exacerbation of ulcerative colitis or Crohn’s disease), constipation, pancreatitis, dysgeusia.
Disorders of the liver and biliary tract: often – increased activity of aminotransferases in the blood plasma; rarely – hepatitis, jaundice, liver dysfunction; very rarely – fulminant hepatitis, liver necrosis, liver failure.
Disorders of the skin and subcutaneous tissues: often – skin rash; rarely – urticaria; very rarely – bullous dermatitis, eczema, erythema, erythema multiforme, Stevens-Johnson syndrome, Lyell’s syndrome (toxic epidermal necrolysis), exfoliative dermatitis, itching, alopecia, photosensitivity reactions, purpura, Henoch-Schönlein purpura. Renal and urinary tract disorders: very rarely – acute kidney injury (acute renal failure), hematuria, proteinuria, tubulointerstitial nephritis, nephrotic syndrome, papillary necrosis.
General disorders and disorders at the injection site: often – pain, compaction at the injection site; rarely – swelling, necrosis at the injection site.
Cardiovascular disorders
There may be a slight increase in the risk of developing cardiovascular thrombotic complications (for example, myocardial infarction), especially with long-term use of diclofenac in high doses (daily dose more than 150 mg).
Visual impairment
Visual disturbances such as blurred vision, blurred vision or diplopia appear to be class effects of NSAIDs and are reversible upon discontinuation of use. A possible mechanism for the development of such disorders is inhibition of the synthesis of prostaglandins and other related substances, which alters the regulation of retinal blood flow, which is manifested by potential visual disturbances. If such symptoms develop during diclofenac therapy, an ophthalmological examination should be considered to exclude any other causes.
If any of the side effects indicated in the instructions get worse, or you notice any other side effects not listed in the instructions, tell your doctor.
Interaction
Interaction
Identified interactions CYP2C9 isoenzyme inhibitors
Caution should be exercised when using diclofenac concomitantly with CYP2C9 inhibitors (such as voriconazole) due to the possible increase in diclofenac serum concentrations and exposure.
Lithium, digoxin
Diclofenac may increase lithium levels and digoxin concentrations in blood plasma. It is recommended to monitor lithium levels and digoxin concentrations in the blood serum.
Diuretics and antihypertensive drugs
When used simultaneously with diuretics and antihypertensive drugs (for example, beta-blockers, angiotensin-converting enzyme inhibitors, ACE inhibitors), diclofenac may reduce their hypotensive effect. Therefore, in patients, especially elderly patients, when diclofenac is used concomitantly with diuretics or antihypertensive drugs, blood pressure should be regularly measured, renal function and hydration levels monitored (due to an increased risk of nephrotoxicity).
Cyclosporine and tacrolimus
The effect of diclofenac on the activity of prostaglandins in the kidneys may enhance the nephrotoxicity of cyclosporine and tacrolimus. In connection with the above, the dose of diclofenac in patients receiving cyclosporine or tacrolimus should be lower than in patients not receiving these drugs.
Drugs that can cause hyperkalemia
The simultaneous use of diclofenac with potassium-sparing diuretics, cyclosporine, tacrolimus and trimethoprim may lead to an increase in the level of potassium in the blood plasma (in the case of such simultaneous use, this indicator should be monitored frequently). Antibacterial agents are quinolone derivatives.
There are isolated reports of the development of seizures in patients receiving concomitant quinolone derivatives and diclofenac.
Suggested interactions between NSAIDs and glucocorticosteroids
Simultaneous systemic use of diclofenac and other systemic NSAIDs or glucocorticosteroids may increase the incidence of adverse events (in particular, from the gastrointestinal tract).
Anticoagulants and antiplatelet agents
It is necessary to use diclofenac with caution simultaneously with drugs of these groups due to the risk of bleeding. Despite the fact that clinical studies have not established the effect of diclofenac on the action of anticoagulants, there are isolated reports of an increased risk of bleeding in patients taking this combination of drugs. Patients receiving concomitant treatment with these drugs should be carefully monitored.
Selective serotonin reuptake inhibitors
Concomitant use of diclofenac with selective serotonin reuptake inhibitors increases the risk of gastrointestinal bleeding.
Hypoglycemic drugs
The simultaneous use of diclofenac and hypoglycemic drugs is possible, but the effectiveness of the latter does not change. However, there are isolated reports of the development in such cases of both hypoglycemia and hyperglycemia, which necessitated the need to change the dose of hypoglycemic drugs during the use of diclofenac. In connection with the above, during the simultaneous use of diclofenac and hypoglycemic drugs, it is recommended to monitor the concentration of glucose in the blood.
There have been isolated reports of the development of metabolic acidosis with simultaneous use of diclofenac with metformin, especially in patients with impaired renal function.
Methotrexate
Caution should be exercised when using diclofenac less than 24 hours before or 24 hours after taking methotrexate, since in such cases the concentration of methotrexate in the blood may increase and its toxic effect may increase.
Phenytoin
When using phenytoin and diclofenac simultaneously, it is necessary to monitor the concentration of phenytoin in the blood plasma due to a possible increase in its systemic effect.
Inducers of the CYP2C9 isoenzyme
Caution should be exercised when using diclofenac concomitantly with inducers of the CYP2C9 isoenzyme (such as rifampicin), as this may lead to a significant decrease in the concentration of diclofenac in the blood plasma and a decrease in its exposure.
Overdose
Overdose
Symptoms: vomiting, gastrointestinal bleeding, diarrhea, dizziness, tinnitus, convulsions. In case of significant poisoning, acute renal failure and liver damage may develop.
Treatment: supportive and symptomatic treatment is indicated for complications such as decreased blood pressure, renal failure, seizures, gastrointestinal disorders and respiratory depression. Forced diuresis, hemodialysis or hemoperfusion to remove NSAIDs, incl. diclofenac from the body are ineffective, since the active substances of these drugs are largely bound to plasma proteins and undergo intensive metabolism.
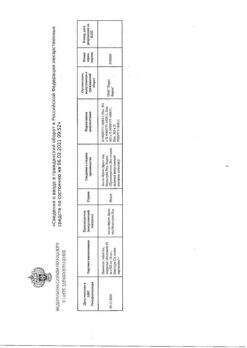
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25 ° C. Freezing is not allowed. Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
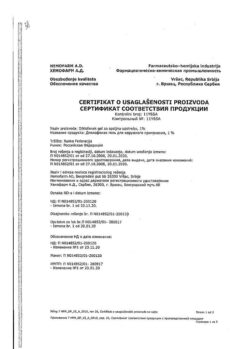
Manufacturer
Manufacturer
Velfarm LLC, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In a light-protected place at a temperature no higher than 25 oC. Freezing is not allowed. Keep out of the reach of children. |
| Manufacturer | Welfarm, Russia |
| Medication form | solution |
| Brand | Welfarm |
Other forms…
Related products
Buy Diclofenac, 25 mg/ml 3 ml 10 pcs with delivery to USA, UK, Europe and over 120 other countries.