No products in the cart.
Diaglinide, tablets 2 mg 30 pcs
€4.52 €4.01
Description
Diaglinide is an oral hypoglycemic agent, it stimulates insulin release from functioning beta cells of the pancreas.
Blocks ATP-dependent channels in the membranes of beta cells through target proteins, which leads to depolarization of beta cells and the opening of calcium channels. The increased influx of calcium ions induces insulin secretion.
In patients with type 2 diabetes an insulinotropic response to a meal is observed within 30 min after the meal. This provides a decrease in blood glucose concentration during the whole period of the meal. At the same time, the plasma concentration of repaglinide decreases rapidly, and 4 hours after taking the drug, low concentrations of repaglinide are detected in the plasma of patients with type 2 diabetes. There is a dose-dependent decrease in glucose concentrations when repaglinide is used in the dose range from 0.5 to 4 mg.
Pharmacokinetics:
In oral administration, absorption of repaglinide from the gastrointestinal tract is high. Time of reaching maximum concentration is 1 hour. Average bioavailability of repaglinide is 63 % (coefficient of variability is 11 %). Since repaglinide dose titration depends on the response to therapy, interindividual variability does not affect the effectiveness of therapy.
The volume of distribution is 30 liters. Binding to plasma proteins – 98%. It is fully metabolized in the liver under the influence of CYP3A4 to inactive metabolites. It is excreted mainly with bile, 8 % by kidneys as metabolites and 1 % by intestine. Elimination half-life is 1 hour.
Hepatic failure
The use of repaglinide in usual doses in patients with impaired liver function may lead to higher concentrations of repaglinide and its metabolites than in patients with normal liver function. In this regard, the use of repaglinide is contraindicated in patients with severe hepatic impairment, and repaglinide should be used with caution in patients with mild to moderate hepatic impairment. Intervals between dose adjustments should also be increased to more accurately assess response to therapy.
Renal failure
The area under the curve “concentration-time” (AUC) and maximum plasma concentration (C) of repaglinide are similar in patients with normal renal function and in patients with mild to moderate renal impairment. In patients with severe renal impairment an increase in AUC and C was observed, but only a weak correlation between repaglinide concentration and creatinine clearance was found. It seems that patients with impaired renal function do not need an initial dose adjustment. However, subsequent dose escalation in patients with type 2 diabetes mellitus in combination with severe renal impairment, in which hemodialysis is required, should be performed with caution.
Indications
Indications
Type 2 diabetes mellitus (if diet, weight loss and exercise are ineffective) in monotherapy or in combination with metformin or thiazolidinediones in cases where it is not possible to achieve satisfactory glycemic control with monotherapy with repaglinide or metformin or thiazolidinediones.
Pharmacological effect
Pharmacological effect
Diaglinide is an oral hypoglycemic agent that stimulates the release of insulin from functioning beta cells of the pancreas.
Blocks ATP-dependent channels in beta cell membranes through target proteins, which leads to depolarization of beta cells and the opening of calcium channels. An increased influx of calcium ions induces insulin secretion.
In patients with type 2 diabetes mellitus, an insulinotropic response to food intake is observed within 30 minutes after ingestion. This ensures a decrease in blood glucose concentrations throughout the entire meal period. At the same time, the concentration of repaglinide in plasma decreases rapidly, and 4 hours after taking the drug, low concentrations of repaglinide are found in the plasma of patients with type 2 diabetes. When repaglinide is used in a dose range from 0.5 to 4 mg, a dose-dependent decrease in glucose concentration is observed.
Pharmacokinetics:
When taken orally, the absorption of repaglinide from the gastrointestinal tract is high. The time to reach maximum concentration is 1 hour. The average bioavailability of repaglinide is 63% (variability coefficient is 11%). Since the dose of repaglinide is titrated based on response to therapy, interindividual variability does not affect the effectiveness of therapy.
Distribution volume – 30 l. Communication with plasma proteins – 98%. Completely metabolized in the liver under the influence of CYP3A4 to inactive metabolites. It is excreted mainly with bile, by the kidneys – 8% in the form of metabolites, through the intestines – 1%. Half-life is 1 hour.
Liver failure
Use of repaglinide in normal doses in patients with impaired liver function may result in higher concentrations of repaglinide and its metabolites than in patients with normal liver function. Therefore, the use of repaglinide is contraindicated in patients with severe hepatic impairment, and in patients with mild to moderate hepatic impairment, repaglinide should be used with caution. The intervals between dose adjustments should also be increased to more accurately assess the response to therapy.
Kidney failure
The area under the concentration-time curve (AUC) and the maximum plasma concentration of repaglinide (Cmax) are similar in patients with normal renal function and in patients with mild or moderate renal impairment. In patients with severe renal impairment, increases in AUC and C were observed, but only a weak correlation was found between repaglinide concentrations and creatinine clearance. It appears that there is no need for initial dosage adjustment in patients with impaired renal function. However, subsequent dose increases in patients with type 2 diabetes mellitus in combination with severe renal impairment requiring hemodialysis should be carried out with caution.
Special instructions
Special instructions
Major surgical interventions and injuries, extensive burns, infectious diseases with febrile syndrome may require the abolition of oral hypoglycemic drugs and the prescription of insulin.
It is necessary to regularly monitor the concentration of glucose in the blood on an empty stomach and after meals. The patient should be warned about the increased risk of hypoglycemia when taking alcohol, NSAIDs, or fasting.
Dose adjustment is necessary in case of physical and emotional stress, or changes in diet.
In malnourished and malnourished patients, care must be taken when selecting the initial and maintenance dose and its titration to avoid hypoglycemia.
Repaglinide is indicated for unsatisfactory glycemic control and persistence of symptoms of diabetes mellitus during diet therapy and exercise.
Because repaglinide is an insulin secretagogue, it may cause hypoglycemia. With combination therapy, the risk of hypoglycemia increases.
Special patient groups
Kidney failure
Dose selection in patients with type 2 diabetes in combination with severe renal impairment should be done with caution.
Liver failure
Administration of normal doses of repaglinide to patients with impaired hepatic function may result in higher concentrations of repaglinide and its metabolites than in patients with normal hepatic function. In this regard, the use of repaglinide is contraindicated in patients with severe liver dysfunction (See section “Contraindications”), and in patients with mild to moderate liver dysfunction, repaglinide should be used with caution. The intervals between dose adjustments should also be increased to more accurately assess the response to therapy.
Impact on the ability to drive vehicles and operate machinery.
Patients’ ability to concentrate and react quickly may be impaired during hypoglycemia and hyperglycemia, which can be dangerous in situations where this ability is especially necessary (for example, when driving or operating machinery).
Patients should be advised to take measures to prevent the development of hypoglycemia and hyperglycemia when driving vehicles and operating machinery. This is especially important for patients with no or decreased severity of symptoms that are warning signs of developing hypoglycemia or who suffer from frequent episodes of hypoglycemia. In these cases, the feasibility of performing such work should be considered.
Active ingredient
Active ingredient
Repaglinide
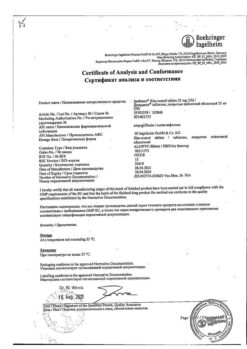
Composition
Composition
Active ingredient:
repaglinide 500 mcg
Excipients:
poloxamer – 3 mg,
meglumine – 10 mg,
lactose monohydrate – 47.8 mg,
microcrystalline cellulose – 33.7 mg,
polacrilin potassium – 4 mg,
colloidal silicon dioxide – 500 mcg,
magnesium stearate – 500 mcg.
Contraindications
Contraindications
diabetic ketoacidosis; diabetic precoma and coma;
infectious diseases, major surgical interventions and other conditions requiring insulin therapy;
severe liver dysfunction;
known hypersensitivity to repaglinide or to any of the components of the drug;
type 1 diabetes mellitus;
simultaneous administration of gemfibrozil (see Interaction with other drugs);
lactase deficiency, lactose intolerance, glucose-galactose malabsorption;
pregnancy and lactation;
age up to 18 years.
Clinical studies have not been conducted in patients under 18 years of age and over 75 years of age.
It should be used with caution (the need for more careful monitoring) in case of mild to moderate liver dysfunction, febrile syndrome, chronic renal failure, alcoholism, general serious condition, malnutrition.
Side Effects
Side Effects
The most common side effect is hypoglycemia, the frequency of which depends, as with any type of therapy with
diabetes mellitus, from individual factors such as dietary habits, drug dose, physical activity and stress.
The following are side effects that have been observed with repaglinide and other oral hypoglycemic agents.
All side effects are divided into groups according to the frequency of development, defined as: often (≥1/100 to
Immune system disorders
Very rare: generalized hypersensitivity reactions or immunological reactions such as vasculitis may occur.
Not known: hypersensitivity reactions such as itching, rash, urticaria.
Metabolic disorders
Common: hypoglycemia.
Unknown: hypoglycemic coma, hypoglycemia with loss of consciousness.
As with the use of other hypoglycemic agents, hypoglycemia may develop when using repaglinide. These reactions are in most cases mild and can be managed by eating carbohydrates. Severe reactions may require medical attention, including intravenous dextrose (glucose). The risk of hypoglycemia may increase when repaglinide interacts with other drugs (see section “Interactions with other drugs”).
Visual disorders
Very rare: visual disturbances.
Changes in blood glucose concentrations can lead to visual disturbances, especially at the initial stage of therapy with hypoglycemic drugs. However, these changes are usually transitory.
Cardiovascular disorders
Rarely: cardiovascular diseases.
The risk of cardiovascular disease increases with type 2 diabetes. An increased risk of acute coronary syndrome was found in patients receiving repaglinide compared with patients receiving a sulfonylurea, but not compared with patients receiving metformin or acarbose. However, a cause-and-effect relationship has not been established.
Digestive system disorders
Common: abdominal pain, diarrhea.
Very rare: vomiting, constipation.
Unknown: nausea.
Disorders of the liver and biliary tract
Very rare: liver dysfunction.
In very rare cases, severe liver dysfunction has been reported, however, a causal relationship with repaglinide has not been established.
Very rare: increased activity of liver enzymes.
Interaction
Interaction
It is necessary to take into account the possible interaction of repaglinide with drugs that affect glucose metabolism.
Metabolism, and thus clearance of repaglinide, may be altered by drugs that act by inhibiting or activating cytochrome P-450 enzymes. Particular caution should be exercised when co-administering inhibitors of CYP2C8 and CYP3A4 with repaglinide. Inhibitors of the anion transport protein OATP1B1 (eg, cyclosporine) may also increase plasma concentrations of repaglinide.
The following drugs may enhance and/or prolong the hypoglycemic effect of repaglinide:
Gemfibrozil, trimethoprim, rifampicin, clarithromycin, ketoconazole, itraconazole, cyclosporine, other hypoglycemic drugs, monoamine oxidase inhibitors, non-selective beta blockers, angiotensin-converting enzyme inhibitors, salicylates, non-steroidal anti-inflammatory drugs (NSAIDs), octreotide, ethanol and anabolic steroids.
Beta blockers may mask the symptoms of hypoglycemia.
Co-administration of cimetidine, nifedipine or simvastatin (which are CYP3A4 substrates) with repaglinide does not have a significant effect on the pharmacokinetic parameters of repaglinide.
Repaglinide does not have a clinically significant effect on the pharmacokinetic properties of digoxin, theophylline or warfarin when used in healthy volunteers. Thus, there is no need for dose adjustment of these drugs when used together with repaglinide.
The following drugs may reduce the hypoglycemic effect of repaglinide:
Oral contraceptives, rifampicin, barbiturates, carbamazepine, thiazides, glucocorticosteroids, danazol, thyroid hormones and sympathomimetics.
Concomitant use of oral contraceptives (ethinyl estradiol/levonorgestrel) does not lead to a clinically significant change in the overall bioavailability of repaglinide, although the maximum concentration of repaglinide is achieved earlier. Repaglinide does not have a clinically significant effect on the bioavailability of levonorgestrel, but its effect on the bioavailability of ethinyl estradiol cannot be excluded.
In this regard, during the period of prescribing or discontinuing the above drugs, patients already receiving repaglinide should be closely monitored for timely detection of violations of glycemic control.
Overdose
Overdose
In case of overdose, hypoglycemia may develop. Symptoms: hunger, increased sweating, palpitations, tremors, anxiety, headache, insomnia, irritability, depression, speech and vision impairment.
When repaglinide was used in patients with type 2 diabetes mellitus at a weekly increasing dose from 4 to 20 mg 4 times a day (with each meal) for 6 weeks, a relative overdose was observed, manifested by an excessive decrease in glucose concentration with the development of symptoms of hypoglycemia.
If symptoms of hypoglycemia appear, appropriate measures should be taken to increase the concentration of glucose in the blood (take dextrose or foods rich in carbohydrates). For severe hypoglycemia (loss of consciousness, coma), dextrose is administered intravenously. After regaining consciousness, take easily digestible carbohydrates (to avoid re-development of hypoglycemia).
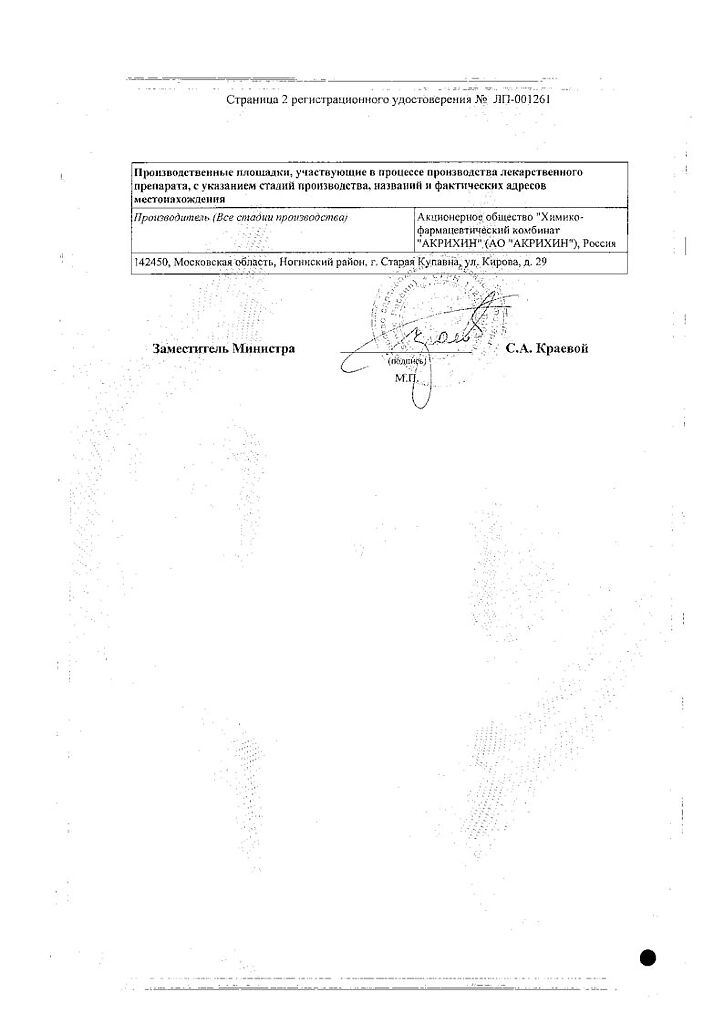
Manufacturer
Manufacturer
Akrikhin JSC, Russia
Additional information
| Manufacturer | Akrihin HFC JSC, Russia |
|---|---|
| Medication form | pills |
| Brand | Akrihin HFC JSC |
Related products
Buy Diaglinide, tablets 2 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.