No products in the cart.
Diabeton MB, 60 mg 30 pcs
€5.99 €5.24
Description
Diabeton MB is an oral hypoglycemic drug from the group of sulfonylurea derivatives of the II generation, which differs from similar drugs by the presence of N-containing heterocyclic ring with endocyclic bond.
Diabeton MB reduces blood glucose levels by stimulating insulin secretion by P-cells of Langerhans islets. After 2 years of treatment, increased postprandial insulin levels and C-peptide secretion persist.
In insulin-independent diabetes mellitus (type II), the drug restores early peak insulin secretion in response to glucose intake and enhances the second phase of insulin secretion. Significant increases in insulin secretion are observed in response to stimulation caused by food intake and glucose administration.
It has been demonstrated that gliclazide increases peripheral tissue sensitivity to insulin. In muscle tissue, the effect of insulin on glucose uptake assessed during the euglycemic hyperinsulin test was significantly increased (+35%), which was due to improved peripheral tissue sensitivity to insulin.
These changes significantly improve the ability to control diabetes. This effect of gliclazide is mainly due to the fact that it promotes the action of insulin on muscle glycogen synthetase. Moreover, studies on muscle tissues have shown that gliclazide induces posttranscriptional changes in GLUT4 relative to glucose. Diabeton MB reduces glucose formation in the liver by normalizing fasting glucose levels.
In addition to affecting carbohydrate metabolism, Diabeton MB has an effect on the microcirculation. Preparation decreases risk of small vessel thrombosis by influence on two mechanisms, which may be involved in development of complications in diabetes: partial inhibition of platelet aggregation and adhesion and decrease of concentration of platelet activating factors (beta-thromboglobulin and thromboxane B2) and restoration of fibulinolytic activity of vascular endothelium and increase of activity of tissue plasminogen activator.
Controlled clinical trials in diabetic patients confirmed antioxidant properties of gliclazide previously demonstrated in clinical pharmacological studies: reduction of plasma lipid peroxide levels and increase of erythrocyte superoxide dismutase activity.
Indications
Indications
Prevention of diabetes complications: reducing the risk of microvascular (nephropathy, retinopathy) and macrovascular complications (myocardial infarction, stroke) in patients with type 2 diabetes through intensive glycemic control.
Type 2 diabetes mellitus with insufficient effectiveness of diet therapy, physical activity and weight loss.
Pharmacological effect
Pharmacological effect
Diabeton MB is an oral hypoglycemic drug from the group of sulfonylurea derivatives of the second generation, which differs from similar drugs by the presence of an N-containing heterocyclic ring with an endocyclic linkage.
Diabeton MB reduces blood glucose levels by stimulating insulin secretion by P cells of the islets of Langerhans. After 2 years of treatment, increases in postprandial insulin levels and C-peptide secretion persist.
In non-insulin-dependent diabetes mellitus (type II), the drug restores the early peak of insulin secretion in response to glucose and enhances the second phase of insulin secretion. A significant increase in insulin secretion is observed in response to stimulation caused by food intake and glucose administration.
Gliclazide has been demonstrated to increase the sensitivity of peripheral tissues to insulin. In muscle tissue, the effect of insulin on glucose uptake assessed during the euglycemic hyperinsulin test was significantly increased (+35%), which was due to improved sensitivity of peripheral tissues to insulin.
These changes significantly improve your ability to control your diabetes. This effect of gliclazide is mainly that it promotes the action of insulin on muscle glycogen synthetase. Moreover, results from studies in muscle tissue showed that gliclazide induces posttranscriptional changes in GLUT4 relative to glucose. Diabeton MB reduces the formation of glucose in the liver, normalizing fasting glucose levels.
In addition to its effect on carbohydrate metabolism, Diabeton MB has an effect on microcirculation. The drug reduces the risk of thrombosis of small vessels by influencing two mechanisms that may be involved in the development of complications in diabetes mellitus: partial inhibition of platelet aggregation and adhesion and a decrease in the concentration of platelet activating factors (beta-thromboglobulin, thromboxane B2), as well as restoration of fibinolytic activity of the vascular endothelium and increased activity of tissue plasminogen activator.
Controlled clinical trials on patients with diabetes mellitus confirmed the antioxidant properties of gliclazide, previously demonstrated in clinical pharmacological studies: a decrease in the level of lipid peroxides in plasma, an increase in the activity of erythrocyte superoxide dismutase.
Special instructions
Special instructions
Hypoglycemia
When taking sulfonylurea derivatives, incl. and gliclazide, hypoglycemia may develop, in some cases in a severe and prolonged form, requiring hospitalization and intravenous administration of dextrose solution for several days (see “Side effects”).
The drug can be prescribed only to those patients whose meals are regular and include breakfast. It is very important to maintain a sufficient intake of carbohydrates from food, because… The risk of developing hypoglycemia increases with irregular or insufficient nutrition, as well as with consumption of foods low in carbohydrates. Hypoglycemia most often develops during a low-calorie diet, after prolonged or vigorous exercise, after drinking alcohol, or when taking several hypoglycemic drugs at the same time.
Typically, symptoms of hypoglycemia go away after eating a meal rich in carbohydrates (such as sugar). It should be borne in mind that taking sweeteners does not help eliminate hypoglycemic symptoms. Experience with other sulfonylureas suggests that hypoglycemia may recur despite initial effective management of the condition. If hypoglycemic symptoms are pronounced or prolonged, even if the condition improves temporarily after eating a meal rich in carbohydrates, emergency medical care is necessary, including hospitalization.
To avoid the development of hypoglycemia, careful individual selection of drugs and dosage regimen is necessary, as well as providing the patient with complete information about the treatment being carried out.
An increased risk of hypoglycemia may occur in the following cases:
– refusal or inability of the patient (especially the elderly) to follow the doctor’s prescriptions and control their condition;
– insufficient and irregular nutrition, skipping meals, fasting and changes in diet;
– imbalance between physical activity and the amount of carbohydrates taken;
– renal failure;
– severe liver failure;
– overdose of the drug Diabeton® MV;
– some endocrine disorders: thyroid diseases, pituitary and adrenal insufficiency;
– simultaneous use of certain drugs (see “Interaction”).
Kidney and liver failure
In patients with hepatic and/or severe renal impairment, the pharmacokinetic and/or pharmacodynamic properties of gliclazide may be altered. The state of hypoglycemia that develops in such patients can be quite long-lasting; in such cases, immediate appropriate therapy is necessary.
Patient Information
It is necessary to inform the patient, as well as his family members, about the risk of hypoglycemia, symptoms and conditions that contribute to its development. The patient must be informed of the potential risks and benefits of the proposed treatment.
The patient must be explained the importance of diet, the need for regular exercise and monitoring blood glucose concentrations.
Insufficient glycemic control
Glycemic control in patients treated with hypoglycemic agents may be impaired in the following situations: fever, trauma, infectious diseases, or major surgery. In these conditions, it may be necessary to stop therapy with Diabeton® MB and prescribe insulin therapy.
In many patients, the effectiveness of oral hypoglycemic agents, incl. gliclazide tends to decrease after a long period of treatment. This effect may be due to both progression of the disease and a decrease in the therapeutic response to the drug. This phenomenon is known as secondary drug resistance, which must be distinguished from primary resistance, in which the drug does not give the expected clinical effect even at the first prescription. Before diagnosing secondary drug resistance in a patient, it is necessary to assess the adequacy of dose selection and the patient’s compliance with the prescribed diet.
Laboratory tests
To assess glycemic control, regular determination of fasting blood glucose concentration and glycosylated hemoglobin HbA1c level is recommended. In addition, it is advisable to regularly self-monitor blood glucose concentrations.
Sulfonylureas may cause hemolytic anemia in patients with glucose-6-phosphate dehydrogenase deficiency. Since gliclazide is a sulfonylurea derivative, caution must be exercised when prescribing it to patients with glucose-6-phosphate dehydrogenase deficiency. The possibility of prescribing a hypoglycemic drug of another group should be assessed.
Impact on the ability to drive vehicles and machinery
Due to the possible development of hypoglycemia when using the drug Diabeton® MB, patients should be aware of the symptoms of hypoglycemia and exercise caution when driving vehicles or performing work that requires a high speed of physical and mental reactions, especially at the beginning of therapy.
Active ingredient
Active ingredient
Gliclazide
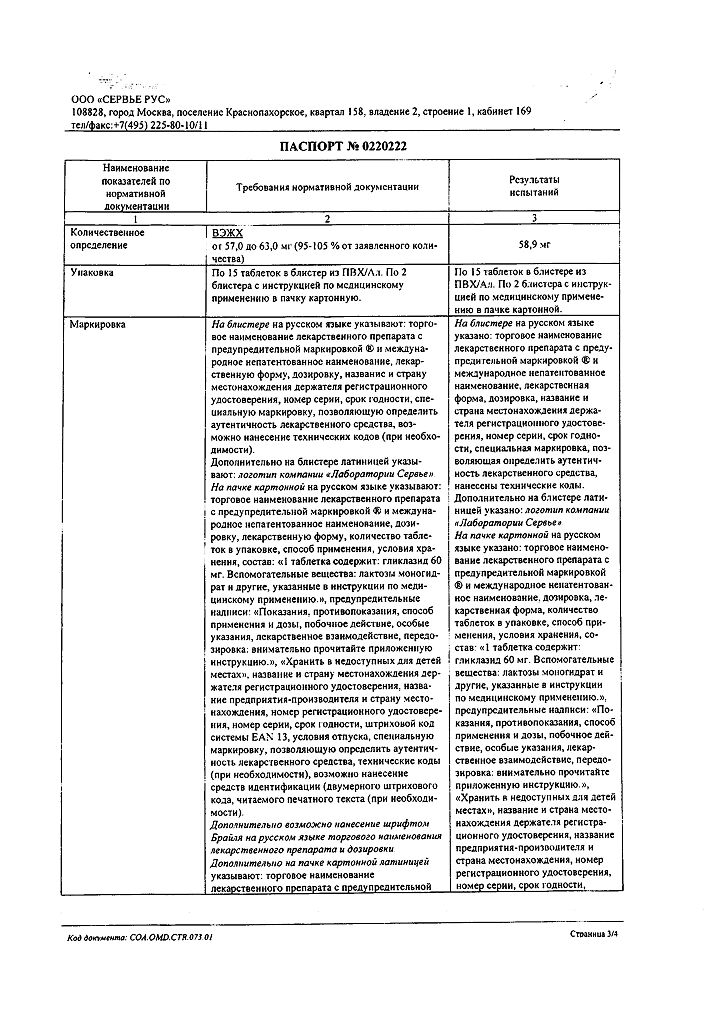
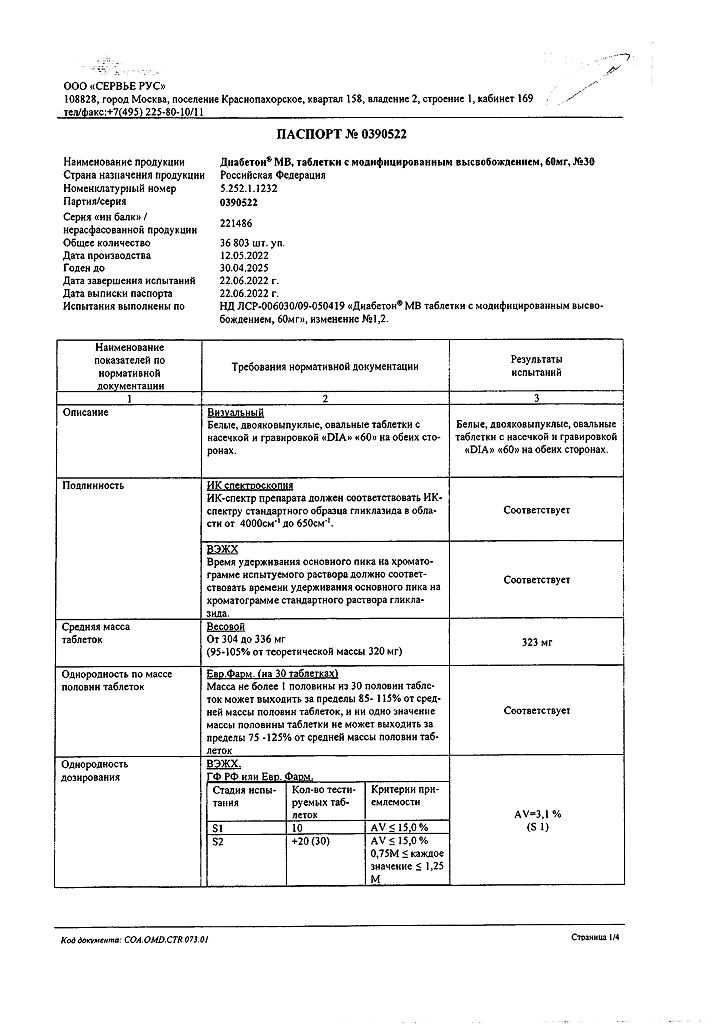
Composition
Composition
Active ingredient:
Gliclazide – 60.0 mg.
Excipients:
lactose monohydrate 71.36 mg,
maltodextrin 22.0 mg,
hypromellose 100 cP 160.0 mg,
magnesium stearate 1.6 mg,
colloidal silicon dioxide anhydrous 5.04 mg.
Pregnancy
Pregnancy
There is no experience with the use of gliclazide during pregnancy. Data on the use of other sulfonylureas during pregnancy are limited.
In studies on laboratory animals, no teratogenic effects of gliclazide were identified. To reduce the risk of developing congenital defects, optimal control (appropriate therapy) of diabetes mellitus is necessary. Oral hypoglycemic drugs are not used during pregnancy. Insulin is the drug of choice for the treatment of diabetes mellitus in pregnant women.
It is recommended to replace the intake of oral hypoglycemic drugs with insulin therapy both in the case of a planned pregnancy and if pregnancy occurs while taking the drug.
Taking into account the lack of data on the entry of gliclazide into breast milk and the risk of neonatal hypoglycemia, breastfeeding is contraindicated during therapy with Diabeton MV.
Contraindications
Contraindications
– hypersensitivity;
– diabetes mellitus type 1;
– diabetic ketoacidosis, diabetic precoma, diabetic coma;
– severe renal or liver failure (in these cases it is recommended to use insulin);
– taking miconazole;
– pregnancy and lactation;
– age up to 18 years.
Due to the fact that the drug contains lactose, Diabeton® MB is not recommended for patients with congenital lactose intolerance, galactosemia, or glucose-galactose malabsorption.
It is not recommended to use in combination with phenylbutazone or danazol. With caution. Old age, irregular and/or unbalanced diet, glucose-6-phosphate dehydrogenase deficiency, severe diseases of the cardiovascular system, hypothyroidism, adrenal or pituitary insufficiency, renal and/or liver failure, long-term therapy with glucocorticosteroids (GCS), alcoholism.
Side Effects
Side Effects
Given the experience with the use of gliclazide and other sulfonylurea derivatives, one should be aware of the possibility of developing the following side effects. Hypoglycemia Like other drugs of the sulfonylurea group, Diabeton® MB can cause hypoglycemia in case of irregular meals and especially if meals are missed.
Possible symptoms of hypoglycemia: headache, severe hunger, nausea, vomiting, increased fatigue, sleep disturbance, irritability, agitation, decreased concentration, slow reaction, depression, confusion, blurred vision and speech, aphasia, tremor, paresis, impaired perception, dizziness, weakness, convulsions, bradycardia, delirium, difficulty breathing, drowsiness, loss of consciousness with the possible development of coma, even to death. Andrenergic reactions may also occur: increased sweating, clammy skin, anxiety, tachycardia, increased blood pressure, palpitations, arrhythmia and angina.
As a rule, the symptoms of hypoglycemia are relieved by taking carbohydrates (sugar). Taking sweeteners is ineffective. Against the background of other sulfonylurea derivatives, relapses of hypoglycemia were observed after its successful relief. For severe or prolonged hypoglycemia, emergency medical attention, possibly hospitalization, is indicated, even if carbohydrate intake is effective. Other side effects
• From the gastrointestinal tract: abdominal pain, nausea, vomiting, diarrhea, constipation. Taking the drug during breakfast can avoid or minimize these symptoms. The following side effects are less common:
• From the skin and subcutaneous tissue: rash, itching, urticaria, erythema, maculopapular rash, bullous rash.
• From the circulatory and lymphatic system: hematological disorders (anemia, leukopenia, thrombocytopenia, granulocytopenia) rarely develop. As a rule, these phenomena are reversible if therapy is discontinued.
• From the liver and biliary tract: increased activity of liver enzymes (aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase), hepatitis (isolated cases). If cholestatic jaundice appears, therapy should be discontinued. The following side effects are usually reversible if therapy is stopped.
• From the organ of vision: transient visual disturbances may occur caused by changes in blood glucose concentrations, especially at the beginning of therapy.
• Side effects inherent in sulfonylurea derivatives: as with other sulfonylurea derivatives, the following side effects were noted: erythrocytopenia, agranulocytosis, hemolytic anemia, pancytopenia, allergic vasculitis, hyponatremia.
There was an increase in the activity of liver enzymes, impaired liver function (for example, with the development of cholestasis and jaundice) and hepatitis; manifestations decreased over time after discontinuation of sulfonylurea drugs, but in some cases led to life-threatening liver failure.
In the ADVANCE study, there was little difference in the incidence of various serious adverse events between the two groups of patients. No new safety data were obtained. A small number of patients experienced severe hypoglycemia, but the overall incidence of hypoglycemia was low. The incidence of hypoglycemia in the intensive glycemic control group was higher than in the standard glycemic control group. Most episodes of hypoglycemia in the intensive glycemic control group were observed during concomitant insulin therapy.
Interaction
Interaction
1. Drugs and substances that increase the risk of hypoglycemia (increasing the effect of gliclazide)
Contraindicated combinations
Miconazole (with systemic administration and when using the gel on the oral mucosa): enhances the hypoglycemic effect of gliclazide (possible development of hypoglycemia up to the state of coma).
Not recommended combinations
Phenylbutazone (systemic administration): enhances the hypoglycemic effect of sulfonylurea derivatives (displaces them from association with plasma proteins and/or slows down their elimination from the body).
It is preferable to use another anti-inflammatory drug. If taking phenylbutazone is necessary, the patient should be warned about the need for glycemic control. If necessary, the dose of Diabeton® MB should be adjusted while taking phenylbutazone and after its termination.
Ethanol: increases hypoglycemia by inhibiting compensatory reactions and can contribute to the development of hypoglycemic coma. It is necessary to stop taking drugs that contain ethanol and drinking alcohol.
Combinations requiring precautions
Taking gliclazide in combination with certain drugs: other hypoglycemic agents (insulin, acarbose, metformin, thiazolidinediones, dipeptidyl peptidase-4 inhibitors, GLP-1 agonists); beta-blockers, fluconazole; ACE inhibitors – captopril, enalapril; blockers of histamine H2 receptors; MAO inhibitors; sulfonamides; clarithromycin and NSAIDs are accompanied by an increased hypoglycemic effect and the risk of hypoglycemia.
2. Drugs that increase blood glucose levels (weakening the effect of gliclazide)
Not recommended combinations
Danazol: has a diabetogenic effect. If taking this drug is necessary, the patient is advised to carefully monitor blood glucose. If it is necessary to take drugs together, it is recommended to select the dose of a hypoglycemic agent both while taking danazol and after its discontinuation.
Combinations requiring precautions
Chlorpromazine (antipsychotic): in high doses (>100 mg/day) increases blood glucose concentrations, reducing insulin secretion. Careful glycemic control is recommended. If it is necessary to take drugs together, it is recommended to select the dose of a hypoglycemic agent, both while taking the antipsychotic and after its withdrawal.
GCS (systemic and local use – intra-articular, cutaneous, rectal administration) and tetracosactide: increase blood glucose concentrations with the possible development of ketoacidosis (decreased tolerance to carbohydrates). Careful glycemic control is recommended, especially at the beginning of treatment. If it is necessary to take drugs together, it may be necessary to adjust the dose of the hypoglycemic agent, both while taking GCS and after their withdrawal.
Ritodrine, salbutamol, terbutaline (intravenous administration): beta2-agonists help increase blood glucose concentrations.
Particular attention should be paid to the importance of self-glycemic control. If necessary, it is recommended to transfer the patient to insulin therapy.
3. Combinations to be taken into account
Anticoagulants (eg warfarin). Sulfonylurea derivatives may enhance the effect of anticoagulants when taken together. Anticoagulant dose adjustment may be required.
Overdose
Overdose
Symptoms: hypoglycemia, in severe cases accompanied by coma, convulsions and other neurological disorders.
Treatment: Moderate symptoms of hypoglycemia are corrected by taking carbohydrates, adjusting the dose and/or changing the diet. Careful monitoring of the patient’s condition must be continued until the attending physician is sure that the patient’s health is not in danger. In severe conditions, emergency medical care and immediate hospitalization are required.
If a hypoglycemic coma is suspected or diagnosed, the patient is quickly administered 50 ml of a concentrated glucose solution (40%) intravenously. Then a more diluted glucose solution (5%) is injected intravenously to maintain the required blood glucose level. Careful monitoring must be carried out for at least the next 48 hours. In the future, depending on the patient’s condition, the need for further monitoring of the patient’s vital functions should be decided.
In patients with liver disease, plasma clearance of gliclazide may be delayed. Dialysis in such patients is usually not performed due to the pronounced binding of gliclazide to plasma proteins.
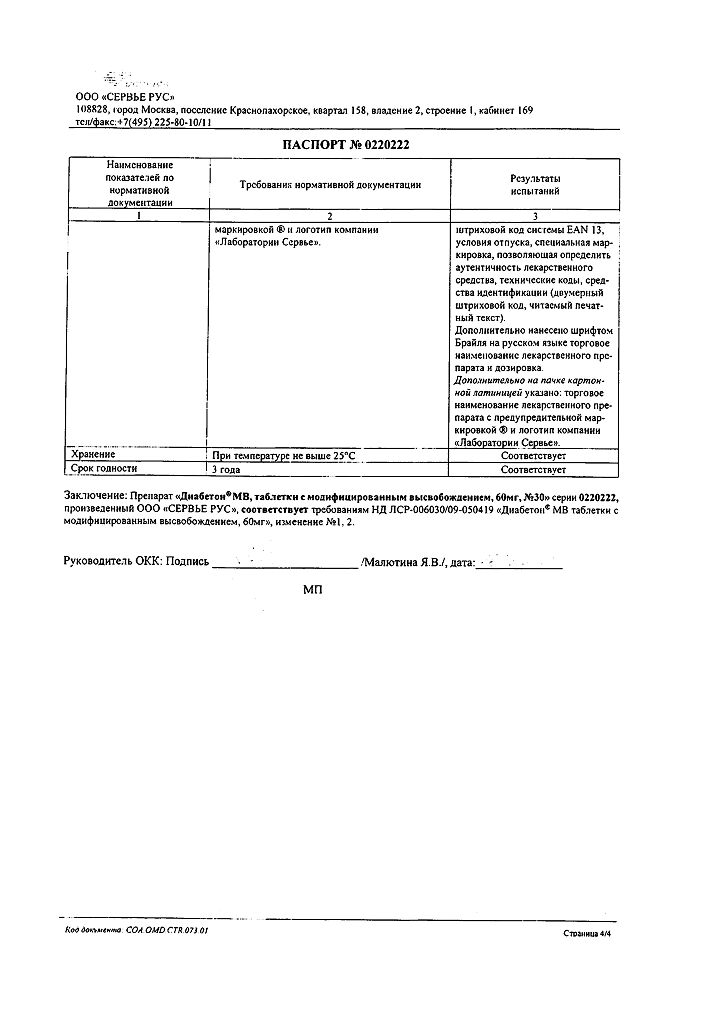
Storage conditions
Storage conditions
No special storage conditions required
Shelf life
Shelf life
2 years
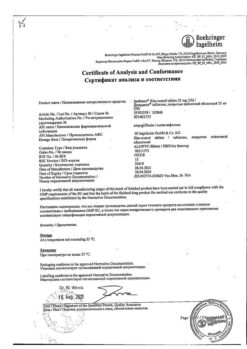
Manufacturer
Manufacturer
Servier Rus LLC, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | No special storage conditions required |
| Manufacturer | Servier Rus LLC, Russia |
| Medication form | controlled release tablets |
| Brand | Servier Rus LLC |
Related products
Buy Diabeton MB, 60 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.