No products in the cart.
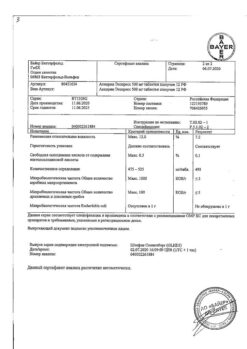
Dexamethasone-Vial, 4 mg/ml 1 ml 25 pcs
€6.12 €5.44
Description
Dexamethasone-Vial is a glucocorticosteroid (GCS), a methylated derivative of fluoroprednisolone, inhibits the release of interleukin-1, interleukin-2, interferon gamma from lymphocytes and macrophages. It has anti-inflammatory, anti-allergic, desensitizing, anti-shock, anti-toxic and immunosuppressive effects.
Inhibits release of adrenocorticotropic hormone (ACTH) and beta-lipotropin by pituitary gland, but does not decrease circulating beta-endorphin. It inhibits the secretion of thyrotropic hormone (TSH) and follicle stimulating hormone (FSH).
It increases CNS excitability, reduces the number of lymphocytes and eosinophils, increases the number of red blood cells (stimulates production of erythropoietins).
Interacts with specific cytoplasmic receptors and forms a complex that penetrates the cell nucleus and stimulates mRNA synthesis; the latter induces the formation of proteins, including lipocortin, which mediate cellular effects.
Lipocortin inhibits phospholipase A2, inhibits the release of arachidonic acid and inhibits the synthesis of endoperoxins, prostaglandins and leukotrienes which contribute to inflammatory processes and allergies.
Protein metabolism: decreases the amount of protein in the plasma (at the expense of globulins) with an increase in the albumin/globulin ratio, increases the synthesis of albumin in the liver and kidneys; increases protein catabolism in muscle tissue.
Lipid metabolism: increases the synthesis of higher fatty acids and thyroglobulin (TG), redistributes fat (fat accumulation mainly in the shoulder girdle, face, abdomen), leads to hypercholesterolemia.
Carbohydrate metabolism: increases absorption of carbohydrates from the gastrointestinal tract; increases the activity of glucose-6-phosphatase, leading to increased glucose flow from the liver into the blood; increases phosphoenolpyruvate carboxylase activity and synthesis of aminotransferases, leading to activation of gluconeogenesis.
Water-electrolyte metabolism: retains sodium ions and water in the body, stimulates excretion of potassium ions (mineralocorticosteroid activity), reduces absorption of calcium ions from the gastrointestinal tract, “washes” calcium ions from the bones, increases excretion of calcium ions by the kidneys.
The anti-inflammatory effect is associated with inhibition of release of inflammatory mediators by eosinophils; induction of lipocortin formation and reduction of the number of mast cells producing hyaluronic acid; and reduction of capillary permeability, stabilization of cell and organelle membranes (especially lysosomal).
The anti-allergic effect develops as a result of suppression of synthesis and secretion of allergy mediators, inhibition of release of histamine and other biologically active substances from sensitized mast cells and basophils, reduction of circulating basophils, suppression of development of lymphoid and connective
tissue, decrease in quantity of T- and B-lymphocytes, mast cells, decrease in sensitivity of effector cells to mediators of allergy, suppression of antibody formation, changes in immune response of the body.
In chronic obstructive pulmonary disease (COPD) the action is mainly based on inhibition of inflammatory processes, inhibition or prevention of mucous membrane edema, inhibition of eosinophilic infiltration of submucous layer of bronchial epithelium, deposition of circulating immune complexes in bronchial mucosa and inhibition of mucous membrane erosion and desquamation.
It increases sensitivity of beta-adrenoreceptors of small and medium caliber bronchi to endogenous catecholamines and exogenous sympathomimetics, reduces mucus viscosity by inhibiting or reducing its production.
The antishock and antitoxic action is associated with increase of arterial pressure (BP) (due to increase of concentration of circulating catecholamines and restoration of sensitivity of adrenoreceptors to them and vasoconstriction), reduction of vascular wall permeability, membranoprotective properties, activation of liver enzymes involved in metabolism of endo- and xenobiotics.
The immunosuppressive effect is caused by inhibition of release of cytokines (interleukin-1 and interleukin-2, interferon gamma) from lymphocytes and macrophages.
Inhibits the synthesis and secretion of ACTH and secondary to the synthesis of endogenous GCS. Inhibits connective tissue reactions during the inflammatory process and reduces the possibility of scar tissue formation.
The peculiarity of action is a significant inhibition of pituitary function and almost complete absence of mineralocorticosteroid activity. Doses of 1-1.5 mg/day inhibit adrenal cortex; biological half-life is 32-72 hours (duration of suppression of hypothalamic-pituitary-adrenal system).
In terms of glucocorticosteroid activity, 0.5 mg of dexamethasone corresponds to approximately 3.5 mg of prednisone (or prednisolone), 15 mg of hydrocortisone or 17.5 mg of cortisone.
Pharmacokinetics
It is slowly absorbed after an intravenous injection, reaching maximum plasma levels after 7-9 hours.
The binding to plasma proteins is 80%. It penetrates through the blood-brain and placental barriers.
Metabolized in the liver. T1/2 is 3-5 hours. It is excreted by the kidneys (a small part is excreted by the lactating glands).
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
1 ml of the solution contains:
The active ingredient:
dexamethasone sodium phosphate 4 mg;
Excipients:
Methylparaben, 1.5 mg;
propylparaben, 0.2 mg;
sodium metabisulfite, 2 mg;
dinatrium edetate – 1 mg;
sodium hydroxide – to pH 7-8.5;
water for injection – up to 1 ml.
How to take, the dosage
How to take, the dosage
The dosing regimen is individual and depends on indications, patient’s condition and his reaction to therapy. The drug is administered intravenously slowly by trickle or drip (in acute and emergency conditions); intramuscularly; local (to the pathological formation) administration is also possible. In order to prepare a solution for intravenous (IV) drip infusion sodium chloride isotonic solution or 5% dextrose solution should be used.
Dexamethasone sodium phosphate: intraarticularly, in the lesion – 0.2-6 mg, repeated once every 3 days or 3 weeks.
I/m or IV: 0.5-9 mg/day.
To treat cerebral edema, 10 mg for the first administration, 4 mg w/v/m every 6 h thereafter until symptoms disappear. The dose may be reduced after 2-4 days with gradual withdrawal over a period of 5-7 days after elimination of cerebral edema. The maintenance dose is 2 mg 3 times a day.
For treatment of shock, the first administration is 20 mg w/v, followed by 3 mg/kg over 24 h as an IV infusion or a single injection of 2 to 6 mg/kg or 40 mg as a single injection given every 2-6 h; a single injection of 1 mg/kg may be administered w/v. Shock therapy should be discontinued as soon as the patient’s condition has stabilized; the usual duration is no more than 2-3 days.
Allergic diseases – 4-8 mg in/m in the first injection. Further treatment is carried out with oral dosage forms.
In case of nausea and vomiting during chemotherapy – IV 8-20 mg 5-15 minutes before the chemotherapy session. Further chemotherapy should be carried out using oral dosage forms.
For treatment of neonatal respiratory distress syndrome – in/m 4 injections of 5 mg every 12 hours, thereafter from the seventh day once every 24 hours. The maximum daily dose is 80 mg.
For children: for treatment of adrenal insufficiency, 23 µg/kg (0.67 mg/m2) once every 3 days, or 7.8-12 µg/kg (0.23-0.34 mg/m2/day), or 28-170 µg/kg (0.83-5 mg/m2) once every 12-24h, in/m.
Interaction
Interaction
Dexamethasone is pharmaceutically incompatible with other drugs (may form insoluble compounds).
Dexamethasone increases the toxicity of cardiac glycosides (due to the resulting hypokalemia the risk of arrhythmias increases). It accelerates excretion of acetylsalicylic acid, reduces the content of its metabolites in blood (when dexamethasone is canceled the concentration of salicylates in blood increases and the risk of side effects increases).
When used simultaneously with live antiviral vaccines and against the background of other types of immunization increases the risk of virus activation and development of infections. Increases the metabolism of isoniazid, mexiletine (especially in “fast acetylators”), which leads to a decrease in their plasma concentrations. Increases the risk of hepatotoxic effects of paracetamol (induction of “liver” enzymes and formation of the toxic metabolite of paracetamol).
Enhances (with prolonged therapy) folic acid.
Hypokalemia caused by GCS may increase the severity and duration of muscle blockade against myorelaxants.
In high doses it reduces the effect of somatropin.
Dexamethasone reduces the effect of hypoglycemic drugs; increases the anticoagulant effect of coumarin derivatives.
Limits the effect of vitamin D on absorption of calcium ions in the intestinal lumen.
Ergocalciferol and parathormone prevent the development of osteopathy caused by GCS.
Decreases the concentration of praziquantel in the blood.
Cyclosporine (depresses metabolism) and ketoconazole (reduces clearance) increase toxicity.
Thiazide diuretics, carboanhydrase inhibitors, other GCS and amphotericin B increase the risk of hypokalemia; sodium-containing drugs increase the risk of edema and increased BP.
NSAIDs and ethanol increase the risk of gastrointestinal mucosal ulceration and bleeding; in combination with NSAIDs for treatment of arthritis, the dose of GCS may be reduced because of the summation of therapeutic effect.
Indomethacin, by displacing dexamethasone from binding to albumin, increases the risk of its side effects.
Amphotericin B and carboanhydrase inhibitors increase the risk of osteoporosis.
The therapeutic effect of GKS is reduced by phenytoin, barbiturates, ephedrine, theophylline, rifampicin and other inducers of “hepatic” microsomal enzymes (increased metabolic rate).
Mitotan and other adrenal cortex inhibitors may necessitate increasing the dose of GCS.
The clearance of GCS is increased with thyroid hormones.
Immunosuppressants increase the risk of developing infections and lymphoma or other lymphoproliferative disorders associated with Epstein-Barr virus.
Estrogens (including oral estrogen-containing contraceptives) decrease GCS clearance, prolong the elimination half-life and their therapeutic and toxic effects.
The occurrence of hirsutism and acne is promoted by the simultaneous use of other steroid hormonal drugs – androgens, estrogens, anabolics, and oral contraceptives.
Tricyclic antidepressants may increase the severity of depression caused by taking GCS (not indicated for therapy of these side effects).
The risk of cataracts increases when used with other GCS, antipsychotic medications (neuroleptics), carbutamide and azathioprine.
The concomitant use with m-cholinoblockers (including antihistamines, tricyclic antidepressants) and nitrates promotes increased intraocular pressure.
The risk of arachnoiditis increases with concomitant intertreatment with yofendilat.
Special Instructions
Special Instructions
Contraindications
Contraindications
For short-term use for “vital” indications, the only contraindication is hypersensitivity.
For intraarticular administration: previous arthroplasty, pathological bleeding (endogenous or caused by anticoagulants), intraarticular bone fracture, infectious (septic) inflammatory process in the joint and periarticular infections (incl. history), as well as general infectious disease, marked periarticular osteoporosis, absence of signs of inflammation in the joint (so-called “dry” joint, for example, in osteoarthritis without synovitis), marked bone destruction and deformity of the joint (severe narrowing of the joint cleft, ankylosis), instability of the joint as an arthritis outcome, aseptic necrosis of bone epiphyses forming the joint.
With caution:
For intraarticular administration: the patient’s general severe state and ineffective (or of short duration) of 2 previous injections (taking into consideration the individual properties of the GCS used).
Side effects
Side effects
Endocrine system disorders: decreased glucose tolerance, “steroid” diabetes mellitus or manifestation of latent diabetes mellitus, suppression of adrenal function, Icenko-Cushing’s syndrome (moon-shaped face, pituitary-type obesity, hirsutism, increased BP, dysmenorrhea, amenorrhea, myasthenia, stretch marks), delayed sexual development in children.
In the digestive system: nausea, vomiting, pancreatitis, “steroid” gastric and duodenal ulcer, erosive esophagitis, bleeding and perforation of the gastrointestinal tract, increased or decreased appetite, flatulence, hiccups. In rare cases, increased activity of “liver” transaminases and alkaline phosphatase.
Cardiovascular system disorders: arrhythmias, bradycardia (up to cardiac arrest); development (in susceptible patients) or increase of severity of chronic heart failure, ECG-changes characteristic for hypokalemia, increased BP, hypercoagulation, thrombosis. In patients with acute and subacute myocardial infarction – expansion of the focus of necrosis, delayed formation of scar tissue, which may lead to rupture of the heart muscle.
Nervous system disorders: delirium, disorientation, euphoria, hallucinations, manic-depressive psychosis, depression, paranoia, increased intracranial pressure, nervousness or anxiety, insomnia, dizziness, vertigo, cerebellar pseudotum, headache, seizures.
Senses: sudden loss of vision (when parenteral administration in the head, neck, nasal cavities, scalp may cause deposition of crystals of the drug in the vessels of the eye), posterior subcapsular cataract, increased intraocular pressure with possible damage to the optic nerve, tendency to develop secondary bacterial, fungal or viral eye infections, trophic changes of the cornea, exophthalmus.
Metabolic disorders: increased excretion of calcium ions, hypocalcemia, weight gain, negative nitrogen balance (increased protein breakdown), increased sweating.
The mineralocorticosteroid-induced fluid and sodium ion retention (peripheral edema), hypernatremia, hypokalemic syndrome (hypocalemia, arrhythmia, myalgia or muscle spasm, unusual weakness and fatigue).
Musculoskeletal system disorders: growth retardation and ossification processes in children (premature closure of epiphyseal growth zones), osteoporosis (very rarely – pathological bone fractures, aseptic necrosis of the humeral and femoral head), rupture of muscle tendons, “steroid” myopathy, decrease of muscle mass (atrophy).
Skin and mucous membranes: delayed wound healing, petechiae, ecchymosis, skin thinning, hyper- or hypopigmentation, steroid acne, stretch marks, tendency to pyoderma and candidiasis.
Allergic reactions: generalized (skin rash, skin itching, anaphylactic shock), local allergic reactions.
Others: development or exacerbation of infections (the appearance of this side effect is promoted by coadministration of immunosuppressants and vaccination), leukocyturia, withdrawal syndrome.
Local when parenteral administration: burning, numbness, pain, paresthesia and infection at the injection site, rarely – necrosis of surrounding tissues, scar formation at the injection site; skin and subcutaneous tissue atrophy when administered in /m (injection into the deltoid muscle is especially dangerous).
In intravenous injection: arrhythmias, “rushes” of blood to the face, convulsions.
In intracranial administration: nasal bleeding.
In intraarticular injection – increase of pain in the joint.
Overdose
Overdose
Symptoms: increase in blood pressure, edema, peptic ulcer, hyperglycemia, impaired consciousness.
Treatment:symptomatic, no specific antidote.
Pregnancy use
Pregnancy use
Similarities
Similarities
Additional information
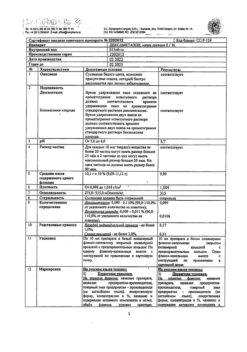
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a light-protected place, at a temperature not exceeding 25 °C |
| Manufacturer | C.S.P. C. Owy Pharmaceutical Co. Ltd, China |
| Medication form | solution for injection |
| Brand | C.S.P. C. Owy Pharmaceutical Co. Ltd |
Related products
Buy Dexamethasone-Vial, 4 mg/ml 1 ml 25 pcs with delivery to USA, UK, Europe and over 120 other countries.