No products in the cart.
Delsia, 3 mg+0.03 mg 63 pcs
€58.34 €50.56
EAN: 8901127035918
SKU: 486339
Categories: Contraceptive, Gynecology and Obstetrics, Hormonal, Medicine
Description
A combined monophasic hormonal contraceptive. The contraceptive effect is based on the interaction of various factors, the most important of which are inhibition of ovulation, increasing the viscosity of the cervical secretion, as a result of which it becomes impermeable to sperm.
When used correctly, the Perl index (a measure of the number of pregnancies per 100 women using the contraceptive over the course of a year) is less than 1. The Perl Index may increase if you miss a dose or use it incorrectly.
In a therapeutic dose, drospirenone also has antiandrogenic and weak anti-mineralocorticoid properties. Deprived of estrogenic, glucocorticoid and antiglucocorticoid activity, drospirenone has a pharmacological profile similar to that of natural progesterone.
With its anti-androgenic activity, it helps to reduce sebum production and improve the clinical course in women with acne (acne vulgaris).
This should be considered when choosing a contraceptive drug, especially for women with hormone-dependent fluid retention and for women with acne and seborrhea. In combination with ethinylestradiol, it improves the lipid profile and increases HDL concentrations.
The use of this combination regulates menstrual bleeding, helping to reduce the severity of pain and volume of menstrual bleeding, reducing one of the risk factors for iron deficiency anemia.
Pharmacokinetics
Indications
Indications
Contraception
Pharmacological effect
Pharmacological effect
Combined monophasic hormonal contraceptive. The contraceptive effect is based on the interaction of various factors, the most important of which are inhibition of ovulation, increasing the viscosity of the cervical secretion, as a result of which it becomes impenetrable to sperm.
When used correctly, the Pearl index (an indicator reflecting the number of pregnancies in 100 women using a contraceptive drug during the year) is less than 1. If a dose is missed or used incorrectly, the Pearl index may increase.
At a therapeutic dose, drospirenone also has antiandrogenic and weak antimineralocorticoid properties. Lacking estrogenic, glucocorticoid and antiglucocorticoid activity, drospirenone has a pharmacological profile similar to that of natural progesterone.
Possessing antiandrogenic activity, it helps reduce the production of sebaceous gland secretions and improve the clinical course in women with acne (acne vulgaris).
This should be taken into account when choosing a contraceptive drug, especially for women with hormone-dependent fluid retention, as well as women with acne and seborrhea. In combination with ethinyl estradiol, it improves the lipid profile and increases the concentration of HDL.
The use of this combination regulates menstrual bleeding, helping to reduce the severity of pain and the volume of menstrual bleeding, reducing one of the risk factors for the development of iron deficiency anemia.
Pharmacokinetics
Special instructions
Special instructions
Before starting to use drugs containing this combination, pregnancy should be excluded and it is recommended to undergo a thorough general medical and gynecological examination, including examination of the mammary glands and cytological examination of the cervix.
In addition, a violation of the blood coagulation system should be excluded. In case of long-term use, preventive control examinations must be carried out at least once every 6 months.
A number of epidemiological studies have revealed an increased incidence of venous and arterial thrombosis and thromboembolism when taking COCs.
The greatest risk of developing these complications exists in the first year of taking the drug (especially in the first 3 months) or resuming use after a 4-week break. The use of any COC may be complicated by the development of venous thromboembolism (VTE), manifested as deep vein thrombosis and pulmonary embolism.
The estimated incidence of VTE in women taking low-dose estrogen oral contraceptives (less than 50 mcg ethinyl estradiol) is up to 4 per 10,000 women per year, compared with 0.5 to 3 per 10,000 women not using oral contraceptives.
The risk of thrombosis (venous and/or arterial) and thromboembolism increases: with age, in smokers (with an increase in the number of cigarettes smoked or increasing age, the risk further increases, especially in women over 35 years of age), with a family history (i.e., venous or arterial thromboembolism ever in close relatives or parents at a relatively young age), obesity (BMI more than 30 kg/m2); dyslipoproteinemia, arterial hypertension, heart valve diseases, atrial fibrillation; prolonged immobilization; temporary immobilization, including air travel for more than 4 hours; major surgery; any surgery on the lower extremities or major trauma – in these situations it is necessary to stop taking the drug; in case of planned surgery – 4 weeks before it and do not resume taking it for 2 weeks after the end of immobilization.
Peripheral circulatory disorders may also occur in diabetes mellitus, SLE, hemolytic uremic syndrome, chronic inflammatory bowel disease (Crohn’s disease or ulcerative colitis) and sickle cell anemia.
An increase in the frequency and severity of migraine during the use of COCs (which may precede cerebrovascular events) may be grounds for immediate discontinuation of these medications.
In rare cases, the development of liver tumors has been observed during the use of COCs. If severe abdominal pain, liver enlargement, or signs of intra-abdominal bleeding occur, this should be taken into account when making a differential diagnosis.
Recurrent cholestatic jaundice, which develops for the first time during pregnancy or during previous use of sex hormones, requires discontinuation of COCs.
Women with hypertriglyceridemia or a family history of hypertriglyceridemia are at increased risk of developing pancreatitis while taking COCs.
Although slight increases in blood pressure have been described in many women taking COCs, clinically significant increases have rarely been reported. The relationship between taking COCs and a clinically significant increase in blood pressure has not been established. However, if a persistent, clinically significant increase in blood pressure develops while taking a COC, discontinuation of the drug and treatment of arterial hypertension is necessary. Taking COCs can be continued after consulting a doctor if blood pressure has returned to normal with the help of antihypertensive therapy.
Although COCs may have an effect on insulin resistance and glucose tolerance, there is no need to change the therapeutic regimen in diabetic patients using COCs. However, women with diabetes mellitus should be carefully monitored while taking COCs.
Women with a tendency to chloasma should avoid prolonged exposure to the sun and exposure to UV radiation while taking COCs.
Due to its antimineralocorticoid activity, drospirenone increases the concentration of renin and aldosterone in the blood plasma.
While taking COCs, the course of endogenous depression and epilepsy may worsen.
While taking COCs, irregular bleeding (spotting or breakthrough bleeding) may occur, especially during the first months of use. Therefore, assessing any irregular bleeding is only meaningful after 3-4 months of contraception.
If irregular bleeding recurs or develops after previous regular cycles, careful evaluation should be performed to rule out malignancy or pregnancy.
Some women may not develop withdrawal bleeding while off the pill. If you take COCs as directed, pregnancy is unlikely. However, if you have not been taking COCs regularly before, or if there are no two withdrawal bleedings in a row, then pregnancy must be ruled out before continuing to take the drug.
Active ingredient
Active ingredient
Drospirenone, Ethinylestradiol
Composition
Composition
1 tab.
drospirenone
3 mg
ethinylestradiol
30 mcg
Excipients: lactose monohydrate – 60 mg, corn starch – 12.77 mg, colloidal silicon dioxide – 0.8 mg, hypromellose 2910 – 1.6 mg, talc – 1.2 mg, magnesium stearate – 0.6 mg.
Film shell composition: opadry II yellow 31F82689 – 2.4 mg (hypromellose 2910 – 33%, lactose monohydrate – 28%, titanium dioxide (E171) – 22.5%, macrogol 6000 – 10%, talc – 5%, iron dye yellow oxide (E172) – 1.5%).
Pregnancy
Pregnancy
Contraindicated for use during pregnancy and lactation (breastfeeding).
Contraindications
Contraindications
Thrombosis (venous and arterial) currently or in history (including deep vein thrombosis, pulmonary embolism, myocardial infarction, cerebrovascular disorders); conditions preceding thrombosis (including transient ischemic attacks, atrial fibrillation, angina) currently or in history; the presence of multiple or severe risk factors for venous or arterial thrombosis, incl. complicated lesions of the valvular apparatus of the heart, atrial fibrillation, diseases of the cerebral vessels or coronary arteries; uncontrolled arterial hypertension, prolonged immobilization, extensive surgery, surgery on the lower extremities, major injuries, smoking over the age of 35 years, obesity with a BMI of more than 30 kg/m2; hereditary or acquired predisposition to venous or arterial thrombosis, such as resistance to activated protein C (APC), antithrombin III deficiency, protein C deficiency, protein S deficiency, hyperhomocysteinemia and the presence of antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant); migraine with focal neurological symptoms currently or in history; diabetes mellitus with diabetic angiopathy; liver failure and severe liver diseases (before normalization of liver function test values and within 3 months after these indicators return to normal); liver tumors (benign or malignant) currently or in history; severe or acute renal failure; identified hormone-dependent malignant diseases (including genital organs or mammary glands) or suspicion of them; bleeding from the vagina of unknown origin; pregnancy or suspicion of it; lactation period (breastfeeding); pancreatitis with severe hypertriglyceridemia currently or in history; hypersensitivity to the components of the combination.
If any of the above diseases or conditions develop for the first time while using a drug containing this combination, it should be discontinued immediately.
With caution
Risk factors for the development of thrombosis and thromboembolism: smoking, obesity with a BMI less than 30 kg/m2, dyslipoproteinemia, controlled arterial hypertension, migraine without focal neurological symptoms, uncomplicated valvular heart disease, the presence of thrombosis and thromboembolism in a family history (thrombosis, myocardial infarction or cerebrovascular accident at a young age in someone close to relatives); age over 35 years in non-smoking women.
Diseases in which peripheral circulatory disorders may occur: diabetes mellitus without vascular disorders, SLE, hemolytic-uremic syndrome, Crohn’s disease, ulcerative colitis, sickle cell anemia, phlebitis of the superficial veins.
Hereditary angioedema.
Hypertriglyceridemia;
Liver diseases of mild to moderate severity.
Diseases that first appeared or worsened during pregnancy or against the background of previous use of sex hormones (including jaundice and/or itching associated with cholestasis, cholelithiasis, otosclerosis with hearing impairment, porphyria, history of herpes during pregnancy, Sindenham’s chorea, chloasma, postpartum period).
Side Effects
Side Effects
From the immune system: rarely – bronchial asthma, hypersensitivity reactions.
From the nervous system: often – headache.
Mental disorders: often – depression; infrequently – changes in libido.
From the side of the hearing organ: rarely – hearing loss.
From the cardiovascular system: often – migraine; infrequently – increased blood pressure, decreased blood pressure; rarely – thromboembolism.
From the digestive system: often – nausea; infrequently – vomiting, diarrhea.
From the skin and subcutaneous tissues: infrequently – acne, eczema, itching; rarely – erythema nodosum, erythema multiforme.
From the reproductive system and mammary gland: often – menstrual irregularities, acyclic bleeding, tenderness of the mammary glands, increased sensitivity of the mammary gland, leucorrhoea, vulvovaginal candidiasis; uncommon – breast enlargement, vaginitis; rarely – discharge from the mammary glands.
Other: infrequently – fluid retention, changes in body weight.
Interaction
Interaction
Long-term treatment with drugs that induce microsomal liver enzymes, which increases the clearance of sex hormones, can lead to a decrease in contraceptive effectiveness. These drugs include: phenytoin, barbiturates, primidone, carbamazepine, oxcarbazepine, rifampicin, rifabutin, topiramate, felbamate, griseofulvin and drugs containing St. John’s wort.
HIV protease inhibitors (ritonavir), non-nucleoside reverse transcriptase inhibitors (nevirapine) and combinations thereof may also potentially affect hepatic metabolism.
Maximum enzyme induction is usually achieved approximately 10 days after starting these medications, but may persist for at least 4 weeks after discontinuation.
When taking drugs that affect the induction of microsomal liver enzymes simultaneously and within 28 days after their discontinuation, it is necessary to temporarily use a barrier method of contraception.
Contraceptive protection is reduced when taking antibiotics of the penicillin and tetracycline series due to their reduction in the intrahepatic circulation of estrogens, and as a consequence, a decrease in the concentration of ethinyl estradiol. While taking these antibiotics and for 7 days after their discontinuation, it is necessary to additionally use a barrier method of contraception.
Because The main metabolites of drospirenone in human plasma are formed without the participation of the cytochrome P450 system; inhibitors of this enzyme system do not affect the metabolism of drospirenone.
Oral combined estrogen-progestin contraceptives may affect the metabolism of other drugs, leading to an increase (cyclosporine) or decrease (lamotrigine) in their concentrations in plasma and tissues.
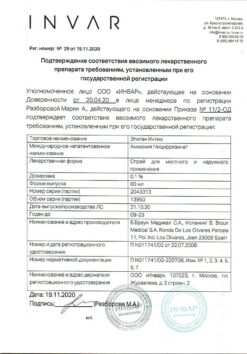
Manufacturer
Manufacturer
Sun Pharmaceutical Industries Ltd, India
Additional information
| Manufacturer | Sun Pharmaceutical Industries Ltd, India |
|---|---|
| Medication form | pills |
| Brand | Sun Pharmaceutical Industries Ltd |
Other forms…
Related products
Gynecology and Obstetrics
Buy Delsia, 3 mg+0.03 mg 63 pcs with delivery to USA, UK, Europe and over 120 other countries.