No products in the cart.
Description
Pharmacodynamics
Antitumor agent from the group of pyrimidine analogues antimetabolites. It is assumed that cytarabine acts by inhibiting DNA polymerase. In addition, it appears to be incorporated into DNA and RNA in a limited way.
Pharmacokinetics
In rapid IV administration, cytarabine only penetrates the BBB in moderate amounts, but after continuous IV infusion, the concentration in cerebrospinal fluid reaches 40-50% of the steady-state plasma concentration.
Protein binding is 15%. It is rapidly metabolized by deamination in the blood and tissues, especially in the liver, and in minimal amounts in the cerebrospinal fluid.
T1/2 is characterized by individual differences. Excreted by the kidneys, less than 10% in unchanged form.
Indications
Indications
Acute non-lymphoblastic leukemia;
blast crisis of chronic myeloid leukemia;
lymphogranulomatosis;
erythromyelosis;
neuroleukemia;
non-Hodgkin’s lymphomas.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
An antitumor agent from the group of antimetabolites-pyrimidine analogues. Cytarabine is thought to act by inhibiting DNA polymerase. In addition, it appears to be incorporated into DNA and RNA to a limited extent.
Pharmacokinetics
With rapid intravenous administration, cytarabine penetrates the blood-brain barrier only in moderate quantities, but after continuous intravenous infusion, the concentration in the cerebrospinal fluid reaches 40-50% of the steady-state plasma concentration.
Protein binding is 15%. Rapidly metabolized by deamination in the blood and tissues, especially in the liver, and in minimal quantities in the cerebrospinal fluid.
T1/2 is characterized by individual differences. Excreted by the kidneys, less than 10% unchanged.
Special instructions
Special instructions
It is not recommended to use cytarabine in patients with chickenpox (including recent or after contact with sick people), herpes zoster or other acute infectious diseases.
Cytarabine is used with caution in patients with suppression of the hematopoietic system, impaired renal and/or liver function, with infiltration of the bone marrow by tumor cells, as well as in patients who have previously received cytotoxic drugs or radiation therapy.
During therapy with cytarabine, the peripheral blood picture, liver and kidney function, and the level of uric acid in the blood plasma should be monitored.
24 hours after administration, the number of leukocytes decreases, on the 7-9th day it reaches minimum values, then briefly increases until the 12th day, after which it decreases again more significantly with a minimum on the 15-24th day. Over the next 10 days, the number of leukocytes quickly increases to the initial level. The platelet count decreases significantly on the 5th day after cytarabine administration, the lowest level is reached on the 12-15th day, reaching the initial level over the next 10 days.
The administration of GCS can prevent or reduce the manifestations of cytarabine syndrome.
During the treatment period, especially in the presence of a large number of blast cells or with a large tumor mass (lymphoma), it is necessary to carry out mandatory drug prevention of hyperuricemia and ensure the intake of allopurinol and a sufficient amount of fluid.
Experimental studies have established the mutagenic effect of cytarabine.
Active ingredient
Active ingredient
Cytarabine
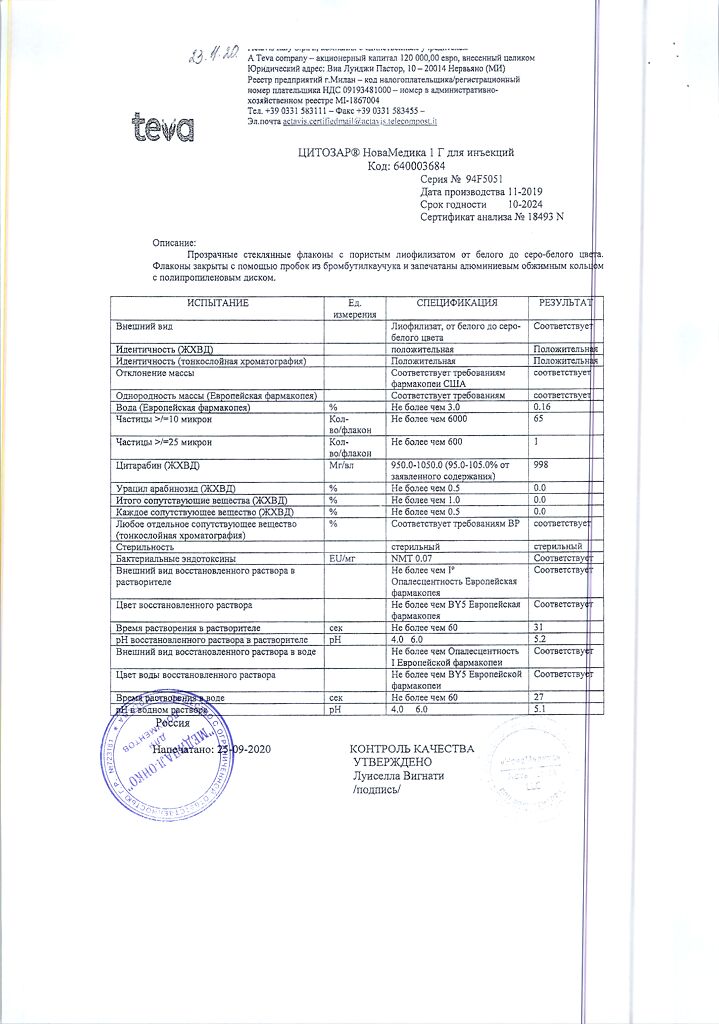
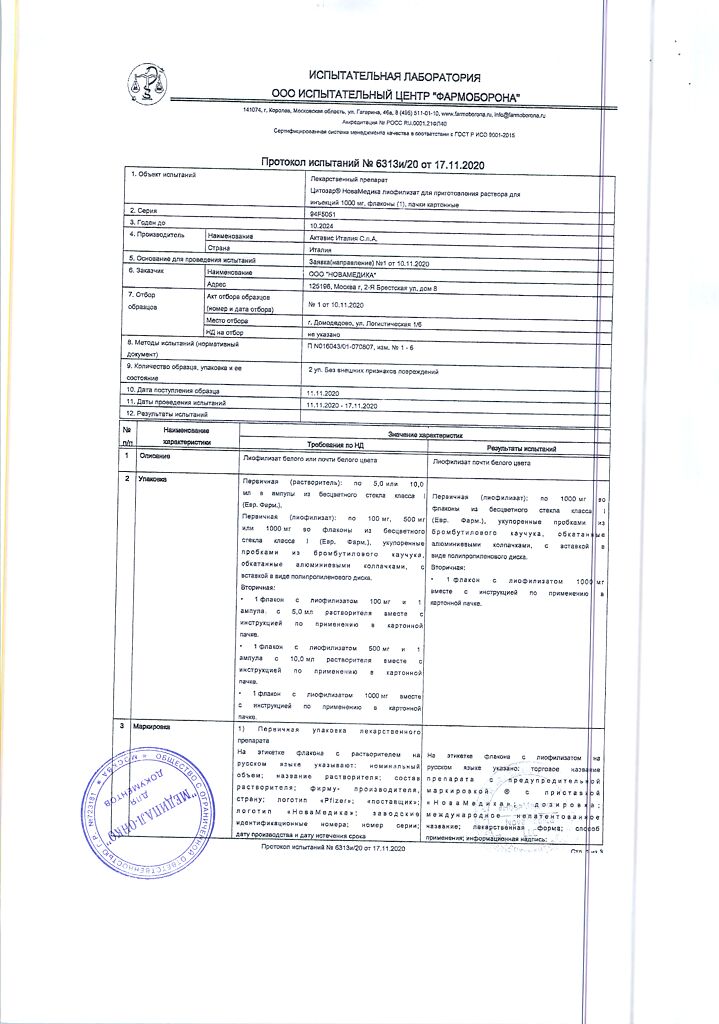
Composition
Composition
1 bottle contains:
Active ingredients:
cytarabine 1000 mg.
1000 mg in a bottle.
In a cardboard package there is 1 bottle complete with solvent.
Pregnancy
Pregnancy
Cytarabine is contraindicated during pregnancy. If necessary, use during lactation should stop breastfeeding.
Women of childbearing potential should use reliable methods of contraception during treatment with cytarabine.
Experimental studies have established the teratogenic and embryotoxic effects of cytarabine.
Contraindications
Contraindications
Myelodepression;
pregnancy;
hypersensitivity to cytarabine.
Side Effects
Side Effects
From the hematopoietic system: leukopenia, thrombocytopenia, anemia, megaloblastosis, reticulocytopenia. The decrease in the number of leukocytes is biphasic, with the first maximum decrease being achieved by 7-9 days. This is followed by a short rise with a maximum on the 12th day. With a second and deeper decrease, the minimum number of leukocytes is observed in days 15-24. Over the next 10 days, the white blood cell count increases rapidly. The decrease in platelet count becomes noticeable by day 5, with a minimum occurring between days 12-15. Over the next 10 days, there is a rapid increase in the platelet count to the initial level.
Infectious complications: against the background of immunosuppression caused by Cytosar and other cytostatic agents, secondary infections may develop.
From the gastrointestinal tract: nausea, vomiting, loss of appetite, abdominal pain, diarrhea, inflammation or ulceration of the gastrointestinal mucosa. When using high doses (2-3 g/m2), ulcerations of the gastrointestinal tract can be severe, and the development of necrotizing colitis, necrosis of the small intestine, and cystic pneumatosis intestinalis, leading to peritonitis, is possible.
From the central and peripheral nervous system: paresthesia, headache, dizziness, neuritis. When using high-dose therapy, disturbances in central nervous system function (confusion, fatigue, memory loss, seizures, coma) and cerebellar function (difficulty speaking, standing or walking, tremor) may occur. With intrathecal administration of Cytosar, cases of paraplegia and necrotizing leukoencephalopathy have been described.
From the liver: impaired liver function with hyperbilirubinemia; with high-dose therapy – sepsis and liver abscess.
From the skin and skin appendages: rash leading to desquamation, itching, spots on the skin, alopecia.
On the part of the organ of vision: when treated with high doses, reversible toxic changes in the cornea and hemorrhagic conjunctivitis may occur. These reactions can be prevented or reduced by topical prophylactic use of corticosteroid eye drops.
From the cardiovascular and respiratory systems: arrhythmias, cardiomyopathy, pericarditis, bronchospasm, pulmonitis, progressive respiratory distress syndrome leading to pulmonary edema and cardiomegaly with possible death; the incidence of these phenomena increases with the use of high doses of Cytosar and cyclophosphamide.
Other side effects: anaphylaxis, hyperuricemia, rarely – impaired renal function, urinary retention, pain, inflammation of the subcutaneous tissue, thrombophlebitis at the injection site, the so-called cytarabine syndrome, characterized by fever, myalgia, bone pain, sometimes chest pain, maculopapular rash, conjunctivitis and malaise. It usually occurs 6-12 hours after using the drug. Corticosteroids have been shown to be effective in preventing and treating this syndrome.
Interaction
Interaction
Cytosar should not be mixed in the same syringe or dropper with other drugs.
The combined use of Cytosar with other antitumor myelosuppressive drugs or radiation therapy in some cases enhances the cytotoxic as well as immunosuppressive activity of these drugs.
When using polychemotherapy with the inclusion of Cytosar, a reversible decrease in the stabilized plasma concentration of digoxin and renal excretion of the glycoside was noted. An alternative for such patients may be the use of digitoxin, a stabilized plasma concentration, which, as it turned out, does not change under similar conditions.
In vitro interaction studies between gentamicin and cytarabine have revealed the existence of cytarabine-associated antagonism in the susceptibility of K. pneumoniae strains to gentamicin.
Clinical data from one patient suggest that the effectiveness of fluorocytosine may be reduced.
Overdose
Overdose
There is a report in the literature that the administration of 4.5 g/m2 Cytarabine in the form of an intravenous infusion (over 1 hour) every 12 hours 12 times in a row led to irreversible changes in the central nervous system and even death. There is no specific antidote.
Treatment is symptomatic.
Storage conditions
Storage conditions
Store the undissolved drug at room temperature (20-25°C). After dissolving the drug in a solvent containing a preservative, store at room temperature for no more than 48 hours. After dissolving in a solvent that does not contain a preservative
Shelf life
Shelf life
5 years.
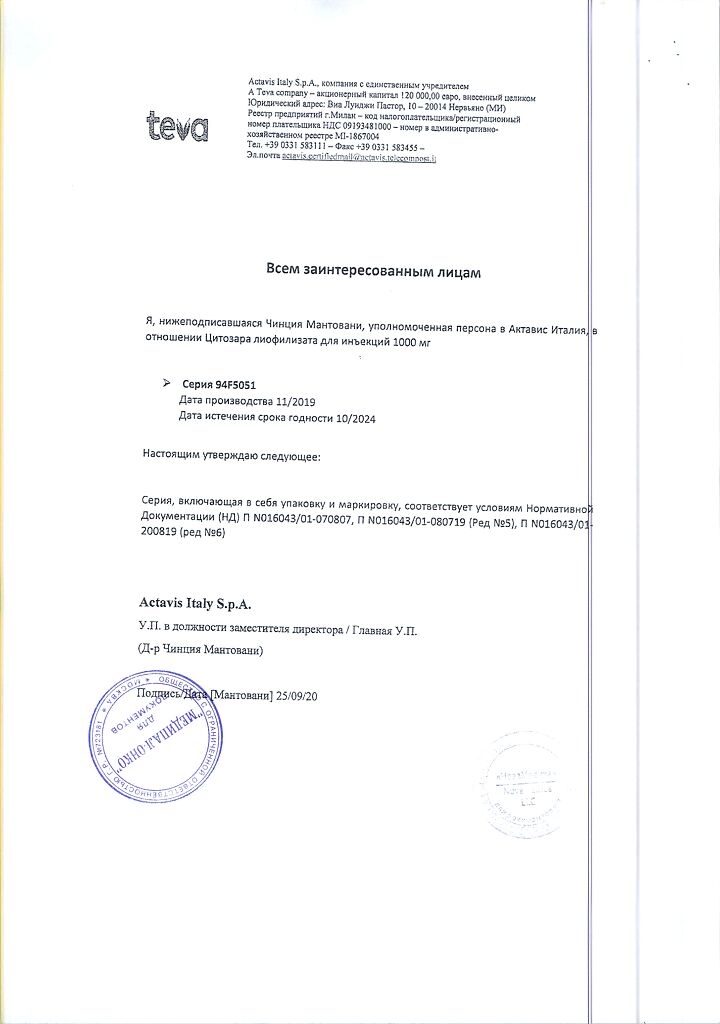
Manufacturer
Manufacturer
Actavis Italy S.p.A., Italy
Additional information
| Shelf life | 5 years. |
|---|---|
| Conditions of storage | Store the undissolved drug at room temperature (20-25°C). After dissolving the drug in a solvent containing a preservative, store at room temperature for no more than 48 hours. After dissolving in a solvent containing no preservative |
| Manufacturer | Actavis Italia S.p.A., Italy |
| Medication form | lyophilizate |
| Brand | Actavis Italia S.p.A. |
Related products
Buy Cytosar, lyophilizate 1000 mg with delivery to USA, UK, Europe and over 120 other countries.