No products in the cart.
Crestor, 20 mg 28 pcs.
€114.42 €95.35
Description

Pharmacotherapeutic group: hypolipidemic drug – HMG-CoA reductase inhibitor
ATX code: C10A A07
Pharmacological properties
Mechanism of action
Rosuvastatin is a selective, competitive inhibitor of HMG-CoA reductase, the enzyme that converts 3-hydroxy-3-methylglutaryl coenzyme A to mevalonate, a cholesterol precursor. The main target of rosuvastatin action is the liver, where cholesterol (cholesterol) synthesis and low-density lipoprotein (LDL) catabolism take place.
Rosuvastatin increases the number of “hepatic” LDL receptors on the cell surface, increasing capture and catabolism of LDL, which in turn leads to inhibition of synthesis of very low density lipoproteins (VLDL), thereby reducing the total amount of LDL and VLDL.
Pharmacodynamics
Crestor® reduces elevated concentrations of LDL cholesterol (LDL-C), total cholesterol, triglycerides (TG), increases concentrations of high-density lipoprotein cholesterol (HDL-C), and reduces concentrations of apolipoprotein B (ApoB), non-HDL-C, HDL-C, TG-LDL-C and increases apolipoprotein A-I (ApoA-I) (see Tables 1 and 2), decreases the ratio of LDL-C/HC-LDL, total CH/LDL and non-LDL-C/HC-LDL and the apoB/apoA-I ratio. Therapeutic effect is developed within one week after the start of therapy with Crestor®, after 2 weeks of treatment it reaches 90% of the maximum possible effect. Maximum therapeutic effect is usually reached by the 4th week of therapy and is maintained with regular use of the drug.
Table 1. Dose-dependent effect in patients with primary hypercholesterolemia (type IIa and IIb according to Fredrickson) (mean adjusted percentage change from baseline)
Dose | Number patients | CHC- LDL | Total CHS | CHS- HDL | TG | CHS- non-LPVP | strong>Apo B | Apo A-I | |||||
Placebo | 13 | -7 | -5 | 3 < | -3 | -7 | -3 | 0 |
10 mg | 17 | -52 | -36 | 14 | -10 | -48 | -42 | 4 |
20 mg | 17 | -55 | -40 | 8 | -23 | -51 | -46 |
|
40 mg | 18 | -63 | -46 | 10 | -28 | -60 |
0 |
Table 2. Dose-dependent effect in patients with hypertriglyceridemia (Fredrickson type IIb and IV) (mean percentage change from baseline value)
Dose | Number of patients | TG | HC- LP NP | Total HC | HC- LPV P | HC- non-LPV P |
TG- LPONP | |
Placebo | 26 | 1 | 5 | 1 | -3 | 2 | 2 | 6 |
10 mg | 23 | -37 | -45 | -40 | 8 | -49 | -48 | -39 |
20 mg | 27 | -37 | -31 | -34 | 22 | -43 | -49 | -40 |
40 mg | 25 | -43 | -43 | -40 | 17 | -51 | -56 |
Clinical Efficacy
Crestor® is effective in adult patients with hypercholesterolemia with or without hypertriglyceridemia, regardless of race, sex or age, including patients with diabetes and familial hypercholesterolemia.
In 80% of patients with hypercholesterolemia type IIa and IIb according to Fredrickson (mean baseline concentration of LDL-C about 4.8 mmol/l) with the use of the drug in dose 10 mg, concentration of LDL-C reached values less than 3 mmol/l.
In patients with heterozygous familial hypercholesterolemia receiving Crestor® in dose of 20-80 mg the positive dynamics of lipid profile indexes are marked (study with participation of 435 patients). After titration to a daily dose of 40 mg (12 weeks of therapy), there is a 53% reduction of LDL-C concentration. In 33% of patients a concentration of less than 3 mmol/l of LDL-C is achieved.
In patients with homozygous familial hypercholesterolemia taking Crestor® in doses of 20 mg and 40 mg the average decrease of LDL-C concentration is 22%.
In patients with hypertriglyceridemia with an initial TG concentration of 273 to 817 mg/dL who received Crestor® in doses ranging from 5 mg to 40 mg once daily for 6 weeks, plasma TG concentrations were significantly reduced (see Table 2).
Additive effect is observed in combination with fenofibrate with regard to triglyceride concentration and with nicotinic acid in lipid-lowering doses with regard to HDL-C concentration (see also section “Special indications”).
. In the METEOR study involving 984 patients aged 45-70 years with a low risk of coronary heart disease (CHD) (10-year Framingham Scale risk less than 10%), a mean CHD-LDL concentration of 4,0 mmol/L (154.5 mg/dL) and subclinical atherosclerosis (which was assessed by carotid intima-media complex thickness – CCTIM), the effect of rosuvastatin on intima-media complex thickness was studied.
Patients received rosuvastatin at a dose of 40 mg/day or placebo for 2 years. Rosuvastatin therapy significantly slowed the rate of progression of maximal SCIM for 12 carotid segments compared with placebo, with a difference of -0.0145 mm/year [95% confidence interval, -0.0196 to -0.0093; p < 0.001]. Compared with baseline values, there was a decrease of 0.0014 mm/year (0.12%/year (nonsignificant difference)) in the maximal SCIM in the rosuvastatin group compared with an increase of 0.0131 mm/year (1.12%/year (p< 0.001)) in the placebo group. To date, no direct correlation has been demonstrated between decreased SCIM and reduced risk of cardiovascular events. METEOR study was conducted in patients with low risk of CHD, for whom the dose of Crestor® 40 mg is not recommended. The dose of 40 mg should be used in patients with significant hypercholesterolemia and high risk of cardiovascular events.
The results of the JUPITER (Rationale for Use of Statins for Primary Prevention: An Interventional Study to Evaluate Rosuvastatin) study in 17802 patients showed that rosuvastatin significantly reduced the risk of cardiovascular complications (252 in the placebo group versus 142 in the rosuvastatin group) (p < 0.001) with a relative risk reduction of 44%. The efficacy of therapy was noted after the first 6 months of use of the drug. There was a statistically significant 48% reduction in the combined criterion of cardiovascular death, stroke, and myocardial infarction (hazard ratio: 0.52, 95% confidence interval 0.40-0.68, p< 0.001), a 54% reduction in the occurrence of fatal or nonfatal myocardial infarction (hazard ratio: 0.46, 95% confidence interval 0.30-0.70), and a 48% reduction in fatal or nonfatal stroke. Overall mortality was reduced by 20% in the rosuvastatin group (hazard ratio: 0.80, 95% confidence interval 0.67-0.97, p=0.02). The safety profile in patients taking rosuvastatin at a dose of 20 mg was generally similar to the safety profile in the placebo group.
Pharmacokinetics
Absorption and distribution
The maximum plasma concentration of rosuvastatin is reached approximately 5 hours after oral administration. Absolute bioavailability is approximately 20%.
Rosuvastatin is metabolized primarily by the liver, which is the main site of cholesterol synthesis and metabolism of LDL-C. The volume of distribution of rosuvastatin is approximately 134 liters. Approximately 90% of rosuvastatin is bound to plasma proteins, mainly to albumin.
Metabolism
It is subject to limited metabolism (about 10%). Rosuvastatin is a non-core substrate for metabolism by enzymes of cytochrome P450 system. The main isoenzyme involved in metabolism of rosuvastatin is CYP2C9 isoenzyme. CYP2C19, CYP3A4 and CYP2D6 isoenzymes are less involved in metabolism.
The main identified metabolites of rosuvastatin are N-desmethyl and lactone metabolites. N-desmethyl is about 50% less active than rosuvastatin, lactone metabolites are pharmacologically inactive. More than 90% of the pharmacological activity for inhibition of circulating HMG-CoA reductase is provided by rosuvastatin, the rest by its metabolites.
Elimation
About 90% of the dose of rosuvastatin is excreted unchanged through the intestine (including absorbed and unabsorbed rosuvastatin). The remainder is excreted by the kidneys. Plasma elimination half-life (T½) is approximately 19 hours. The elimination half-life does not change with increasing drug dose. Mean geometric plasma clearance is approximately 50 L/hour (coefficient of variation 21.7%). As in the case of other HMG-CoA reductase inhibitors, the membrane cholesterol transporter, which plays an important role in hepatic elimination of rosuvastatin, is involved in the “hepatic” uptake of rosuvastatin.
Linearity
The systemic exposure of rosuvastatin increases in proportion to the dose. Pharmacokinetic parameters do not change with daily administration.
Particular patient populations Age and sex
Gender and age have no clinically significant effect on the pharmacokinetics of rosuvastatin.
Ethnic groups
. Pharmacokinetic studies have shown an approximately two-fold increase in median AUC (area under the concentration-time curve) and Cmax (maximum plasma concentration) of rosuvastatin in patients of the Mongoloid race (Japanese, Chinese, Filipino, Vietnamese and Korean) compared with Caucasians; median AUC and Cmax increased 1.3-fold in Indian patients. Pharmacokinetic analysis showed no clinically significant differences in pharmacokinetics among Caucasians and non-Hispanics.
Renal dysfunction
In patients with mild to moderate renal dysfunction the plasma concentrations of rosuvastatin or N-desmethyl do not change significantly. In patients with severe renal dysfunction (creatinine clearance (CK) less than 30 ml/min) the plasma concentration of rosuvastatin is 3 times higher and that of N-desmethyl is 9 times higher than in healthy volunteers. Plasma concentrations of rosuvastatin were approximately 50% higher in patients on hemodialysis than in healthy volunteers.
Hepatic dysfunction
In patients with hepatic dysfunction of varying severity, no increase in the half-life of rosuvastatin was found in patients with a Child-Pugh score of 7 or lower. Two patients with Child-Pugh scores 8 and 9 showed at least 2-fold increase in half-life. There is no experience with rosuvastatin in patients with a Child-Pugh score above 9.
Genetic polymorphism
. HMG-CoA reductase inhibitors, including Crestor®, bind to the transport proteins OATP1B1 (organic anion transport polypeptide involved in statin uptake by hepatocytes) and BCRP (efflux transporter). Carriers of SLCO1B1 (OATP1B1) c.521CC and ABCG2 (BCRP) c.421AA genotypes had 1.6 and 2.4-fold increased exposure (AUC) to rosuvastatin compared with SLCO1B1 c.521TT and ABCG2 c.421CC genotypes, respectively.
Indications
Indications
Fredrickson primary hypercholesterolemia (type IIa, including familial heterozygous hypercholesterolemia) or mixed hypercholesterolemia (type IIb) as an adjunct to diet when diet and other non-drug treatments (eg, exercise, weight loss) are insufficient;
familial homozygous hypercholesterolemia as an adjunct to diet and other lipid-lowering therapy (eg, LDL apheresis), or in cases where such therapy is not sufficiently effective;
hypertriglyceridemia (Fredrickson type IV) as an adjunct to diet;
to slow the progression of atherosclerosis as an addition to diet in patients who are indicated for therapy to reduce the concentration of total cholesterol and LDL cholesterol;
primary prevention of major cardiovascular complications (stroke, heart attack, arterial revascularization) in adult patients without clinical signs of coronary artery disease, but with an increased risk of its development (age over 50 years for men and over 60 years for women, increased concentration of C-reactive protein (≥ 2 mg/l) in the presence of at least one of the additional risk factors, such as arterial hypertension, low HDL-C concentration, smoking, family history of early onset ischemic heart disease).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Lipid-lowering agent – HMG-CoA reductase inhibitor
Pharmacological action
Lipid-lowering drug, selective competitive inhibitor of HMG-CoA reductase.
Crestor® reduces elevated concentrations of LDL cholesterol (LDL-C), total cholesterol, triglycerides (TG), increases the concentration of high-density lipoprotein cholesterol (HDL-C), and also reduces the concentrations of apolipoprotein B (Apo-B), non-HDL-C, VLDL-C, TG-VLDL and increases the concentration of apolipoprotein A-I (ApoA-I), reduces the ratio LDL-C/HDL-C, total cholesterol/HDL-C and non-HDL-C/HDL-C and Apo-B/ApoA-1 ratio.
The therapeutic effect develops within one week after the start of therapy with Crestor®, after 2 weeks of treatment it reaches 90% of the maximum possible effect. The maximum therapeutic effect is usually achieved by the 4th week of therapy and is maintained with regular use of the drug.
Clinical effectiveness
Crestor® is effective in adult patients with hypercholesterolemia with or without hypertriglyceridemia; regardless of race, gender or age, incl. in patients with diabetes mellitus and familial hypercholesterolemia. In 80% of patients with Fredrickson type IIa and IIb hypercholesterolemia (the average initial LDL-C concentration is about 4.8 mmol/l), when taking the drug at a dose of 10 mg, the LDL-C concentration reaches values of less than 3 mmol/L.
In patients with heterozygous familial hypercholesterolemia receiving Crestor® at a dose of 20-80 mg, positive dynamics in the lipid profile were observed (study involving 435 patients). After titration to a daily dose of 40 mg (12 weeks of therapy), a decrease in LDL-C concentrations by 53% was observed. In 33% of patients, an LDL-C concentration of less than 3 mmol/l is achieved.
In patients with homozygous familial hypercholesterolemia taking Crestor® at doses of 20 mg and 40 mg, the average reduction in LDL-C concentrations is 22%.
In patients with hypertriglyceridemia with an initial TG concentration of 273 to 817 mg/dL who received Crestor® at a dose of 5 mg to 40 mg once daily for 6 weeks, the concentration of TG in the blood plasma was significantly reduced.
An additive effect is observed in combination with fenofibrate in relation to the concentration of triglycerides and with nicotinic acid in lipid-lowering doses in relation to the concentration of HDL-C.
The METEOR study, involving 984 patients aged 45-70 years with a low risk of developing CAD (10-year Framingham risk less than 10%), a mean LDL-C concentration of 4.0 mmol/L (154.5 mg/dL) and subclinical atherosclerosis (assessed by carotid intima-media thickness – IMT) examined the effect of rosuvastatin on the thickness of the intima-media complex. Patients received rosuvastatin at a dose of 40 mg/day or placebo for 2 years. Rosuvastatin treatment significantly slowed the rate of progression of maximum IMT for 12 carotid artery segments compared with placebo, with a difference of -0.0145 mm/year [95% confidence interval -0.0196 to -0.0093; p<0.001]. Compared with baseline values, the rosuvastatin group showed a decrease in maximum IMT by 0.0014 mm/year (0.12%/year (not significant difference)) compared with an increase of 0.0131 mm/year (1.12%/year (p < 0.001)) in the placebo group. To date, a direct relationship between a decrease in IMT and a decrease in the risk of cardiovascular events has not been demonstrated. The METEOR study was conducted in patients at low risk of coronary artery disease for whom the recommended dose of Crestor® 40 mg is not recommended. A dose of 40 mg should be prescribed to patients with severe hypercholesterolemia and a high risk of cardiovascular disease.Results from the JUPITER trial (Rationale for Statins in Primary Prevention: An Intervention Study Evaluating Rosuvastatin) in 17,802 patients showed that rosuvastatin significantly reduced the risk of cardiovascular events (252 in the placebo group compared with 142 in the rosuvastatin group) (p < 0.001) with a relative risk reduction of 44%. The effectiveness of therapy was noted after the first 6 months of using the drug. There was a statistically significant reduction of 48% in the combined criterion, which included death from cardiovascular causes, stroke and myocardial infarction (risk ratio: 0.52, 95% confidence interval: 0.40-0.68, p < 0.001), a 54% reduction in the occurrence of fatal or non-fatal myocardial infarction (risk ratio: 0.46, 95%, confidence interval 0.30-0.70) and 48% - fatal or non-fatal stroke. Overall mortality decreased by 20% in the rosuvastatin group (hazard ratio: 0.80, 95%, confidence interval 0.67-0.97, p=0.02). The safety profile in patients treated with rosuvastatin 20 mg was generally similar to that in the placebo group.PharmacokineticsSuction and distributionCmax of rosuvastatin in blood plasma is achieved approximately 5 hours after oral administration. Absolute bioavailability is approximately 20%.Rosuvastatin is metabolized primarily by the liver, which is the main site of cholesterol synthesis and LDL-C metabolism. Vd of rosuvastatin is approximately 134 l. Approximately 90% of rosuvastatin is bound to plasma proteins, mainly albumin.MetabolismSubject to limited metabolism (about 10%). Rosuvastatin is a non-core substrate for metabolism by enzymes of the cytochrome P450 system. The main isoenzyme involved in the metabolism of rosuvastatin is the CYP2C9 isoenzyme. Isoenzymes CYP2C19, CYP3A4 and CYP2D6 are involved in metabolism to a lesser extent.The main identified metabolites of rosuvastatin are N-desmethyl rosuvastatin and lactone metabolites. N-desmethyl rosuvastatin is approximately 50% less active than rosuvastatin; the lactone metabolites are pharmacologically inactive. More than 90% of the pharmacological activity of inhibiting circulating HMG-CoA reductase is provided by rosuvastatin, the rest is provided by its metabolites.RemovalAbout 90% of the dose of rosuvastatin is excreted unchanged through the intestine (including absorbed and unabsorbed rosuvastatin). The remaining part is excreted by the kidneys. Plasma T1/2 is approximately 19 hours. T1/2 does not change with increasing doses of the drug. The geometric mean plasma clearance is approximately 50 L/h (coefficient of variation 21.7%). As with other HMG-CoA reductase inhibitors, the process of “hepatic” uptake of rosuvastatin involves a membrane cholesterol transporter, which plays an important role in the hepatic elimination of rosuvastatin.LinearitySystemic exposure of rosuvastatin increases in proportion to the dose. Pharmacokinetic parameters do not change when taken daily.Pharmacokinetics in special clinical situationsAge and gender do not have a clinically significant effect on the pharmacokinetics of rosuvastatin.Ethnic groups. Pharmacokinetic studies have shown an approximately twofold increase in the median AUC and Cmax of rosuvastatin in patients of Asian nationality (Japanese, Chinese, Filipinos, Vietnamese and Koreans) compared to Europeans; Indian patients showed a 1.3-fold increase in median AUC and Cmax. Pharmacokinetic analysis did not reveal clinically significant differences in pharmacokinetics between Europeans and representatives of the Black race.Kidney failure. In patients with mild to moderate renal failure, the plasma concentration of rosuvastatin or N-desmethylrosuvastatin does not change significantly. In patients with severe renal failure (creatinine clearance less than 30 ml/min), the concentration of rosuvastatin in the blood plasma is 3 times higher, and the concentration of N-desmethyl rosuvastatin is 9 times higher than in healthy volunteers. Plasma concentrations of rosuvastatin in hemodialysis patients were approximately 50% higher than in healthy volunteers.Liver failure. In patients with various stages of liver failure, an increase in T1/2 of rosuvastatin was not detected in patients with a score of 7 or lower on the Child-Pugh scale. In two patients with 8 and 9 points on the Child-Pugh scale, an increase in T1/2 of at least 2 times was noted. There is no experience with the use of rosuvastatin in patients with a Child-Pugh score of more than 9.Genetic polymorphism. HMG-CoA reductase inhibitors, incl. Crestor® binds to the transport proteins OATP1B1 (organic anion transport polypeptide involved in the uptake of statins by hepatocytes) and BCRP (efflux transporter). Carriers of the SLCO1B1 (OATP1B1) c.521CC and ABCG2 (BCRP) c.421AA genotypes had an increase in exposure (AUC) to rosuvastatin by 1.6 and 2.4 times, respectively, compared with carriers of the SLCO1B1 c.521TT and ABCG2 c.421CC genotypes.
Special instructions
Special instructions
Effect on the kidneys
In patients receiving high doses of Crestor® (mainly 40 mg), tubular proteinuria was observed, which, in most cases, was transient. This proteinuria did not indicate acute kidney disease or progression of kidney disease. In patients taking the drug at a dose of 40 mg, it is recommended to monitor renal function parameters during treatment.
From the musculoskeletal system
The following musculoskeletal effects have been reported with Crestor® at all doses, especially doses greater than 20 mg: myalgia, myopathy, and in rare cases, rhabdomyolysis.
Determination of CPK activity
Determination of CPK activity should not be carried out after intense physical activity or in the presence of other possible reasons for increased CPK activity, which may lead to incorrect interpretation of the results obtained. If the initial CPK activity is significantly increased (5 times higher than ULN), a repeat measurement should be taken after 5-7 days. Therapy should not be started if a repeat test confirms the initial CPK activity (more than 5 times higher than the ULN).
Before starting therapy
When prescribing Crestor®, as well as when prescribing other HMG-CoA reductase inhibitors, caution should be exercised in patients with existing risk factors for myopathy/rhabdomyolysis, it is necessary to consider the balance of risk and possible benefit of therapy and conduct clinical observation.
During therapy
The patient should be informed to immediately report to the doctor the unexpected onset of muscle pain, muscle weakness or cramps, especially in combination with malaise and fever. In such patients, CPK activity should be determined. Therapy should be discontinued if CPK activity is significantly increased (more than 5 times the ULN) or if muscle symptoms are severe and cause daily discomfort (even if CK activity is increased no more than 5 times the ULN).
If symptoms disappear and CPK activity returns to normal, re-prescribing Crestor® or other HMG-CoA reductase inhibitors in lower doses should be considered with careful monitoring of the patient.
Routine monitoring of CPK activity in the absence of symptoms is not advisable.
Very rare cases of immune-mediated necrotizing myopathy have been reported with clinical manifestations in the form of persistent proximal muscle weakness and increased serum CPK levels during treatment or upon discontinuation of statins, incl. rosuvastatin. Additional studies of the muscular and nervous system, serological studies, and therapy with immunosuppressive drugs may be required.
There were no signs of increased effects on skeletal muscles when taking Crestor® and concomitant therapy. However, an increased incidence of myositis and myopathy has been reported in patients taking other HMG-CoA reductase inhibitors in combination with fibric acid derivatives, including gemfibrozil, cyclosporine, nicotinic acid in lipid-lowering doses (more than 1 g/day), azole antifungals, HIV protease inhibitors and macrolide antibiotics. Gemfibrozil increases the risk of myopathy when combined with certain HMG-CoA reductase inhibitors. Thus, simultaneous administration of Crestor® and gemfibrozil is not recommended. The risk/benefit ratio should be carefully weighed when using Crestor® together with fibrates or lipid-lowering doses of nicotinic acid. Taking Crestor® at a dose of 40 mg together with fibrates is contraindicated.
2-4 weeks after the start of treatment and/or when increasing the dose of Crestor®, monitoring of lipid metabolism parameters is necessary (if necessary, dose adjustment is required).
Liver
It is recommended to determine liver function indicators before starting therapy and 3 months after starting therapy. Taking Crestor® should be stopped or the dose reduced if the activity of “liver” transaminases in the blood serum is 3 times higher than the ULN.
In patients with hypercholesterolemia due to hypothyroidism or nephrotic syndrome, treatment of underlying diseases should be carried out before starting treatment with Crestor®.
Special populations: ethnic groups
In pharmacokinetic studies among Chinese and Japanese patients, an increase in systemic concentrations of rosuvastatin was noted compared with values obtained among European patients.
HIV protease inhibitors
Concomitant use of the drug with HIV protease inhibitors is not recommended.
Lactose
The drug should not be used in patients with lactase deficiency, galactose intolerance and glucose-galactose malabsorption.
Interstitial lung disease
Isolated cases of interstitial lung disease have been reported with the use of some statins, especially over long periods of time. Manifestations of the disease may include shortness of breath, nonproductive cough and deterioration in general health (weakness, weight loss and fever). If interstitial lung disease is suspected, statin therapy should be discontinued.
Diabetes mellitus type 2
In patients with glucose concentrations between 5.6 and 6.9 mmol/L, therapy with Crestor® was associated with an increased risk of developing type 2 diabetes mellitus.
Impact on the ability to drive vehicles and machinery
No studies have been conducted to study the effect of Crestor® on the ability to drive a vehicle and use machinery. Caution should be exercised when driving vehicles or doing work that requires increased concentration and speed of psychomotor reactions (dizziness may occur during therapy).
Active ingredient
Active ingredient
Rosuvastatin
Composition
Composition
Active substance:
rosuvastatin (as rosuvastatin calcium) – 20 mg
Excipients: lactose monohydrate – 179 mg, microcrystalline cellulose – 59.64 mg, calcium phosphate – 21.8 mg, crospovidone – 15 mg, magnesium stearate – 3.76 mg.
Pregnancy
Pregnancy
Crestor® is contraindicated during pregnancy and lactation (breastfeeding).
Women of reproductive age should use adequate methods of contraception.
Since cholesterol and other products of cholesterol biosynthesis are important for fetal development, the potential risk of inhibiting HMG-CoA reductase outweighs the benefit of using the drug in pregnant women.
If pregnancy occurs during therapy, the drug should be discontinued immediately.
There are no data regarding the excretion of rosuvastatin in breast milk, therefore, during breastfeeding, the drug should be discontinued
Contraindications
Contraindications
hypersensitivity to rosuvastatin or any of the components of the drug;
liver diseases in the active phase, including a persistent increase in serum transaminase activity and any increase in transaminase activity in the blood serum (more than 3 times compared to ULN);
severe renal dysfunction (creatinine clearance less than 30 ml/min);
myopathy;
simultaneous use of cyclosporine;
in women: pregnancy, lactation, lack of adequate methods of contraception;
patients predisposed to the development of myotoxic complications;
lactose intolerance, lactase deficiency or glucose-galactose malabsorption (the drug contains lactose).
With caution
There is a risk of developing myopathy/rhabdomyolysis – renal failure, hypothyroidism, personal or family history of hereditary muscle diseases and a previous history of muscle toxicity when using other HMG-CoA reductase inhibitors or fibrates; excessive alcohol consumption; age over 65 years; conditions in which an increase in plasma concentration of rosuvastatin is noted; race (Asian race); simultaneous administration with fibrates.
Side Effects
Side Effects
Side effects observed when taking Crestor® are usually mild and go away on their own. As with other HMG-CoA reductase inhibitors, the incidence of side effects is mainly dose-dependent.
Determination of the frequency of adverse reactions: often (> 1/100, 1/1000, 1/10,000, < 1/1000); very rare (< 1/10,000), unspecified frequency (cannot be calculated from the available data).
From the immune system: rarely – hypersensitivity reactions, including angioedema.
From the endocrine system: often – type 2 diabetes mellitus.
From the side of the central nervous system: often – headache, dizziness.
From the digestive system: often – constipation, nausea, abdominal pain; rarely – pancreatitis.
From the skin: infrequently – itching, rash, urticaria.
From the musculoskeletal system: often – myalgia; rarely – myopathy (including myositis), rhabdomyolysis.
Other: often – asthenic syndrome.
From the urinary system: patients receiving Crestor® may experience proteinuria. Changes in the amount of protein in the urine (from none or trace amounts to ++ or more) are observed in less than 1% of patients receiving 10-20 mg of the drug and in approximately 3% of patients receiving 40 mg of the drug. A slight change in the amount of protein in the urine was noted when taking a dose of 20 mg. In most cases, proteinuria decreases or disappears during therapy and does not indicate the onset of acute or progression of existing kidney disease.
From the musculoskeletal system: when using the drug Crestor® in all doses, especially when taken in doses exceeding 20 mg, the following effects on the musculoskeletal system were reported: myalgia, myopathy (including myositis); in rare cases, rhabdomyolysis with or without acute renal failure.
A dose-dependent increase in CPK activity is observed in a small number of patients taking rosuvastatin. In most cases it was minor, asymptomatic and temporary. If CPK activity increases (more than 5 times compared to ULN), therapy should be suspended.
From the liver: when using rosuvastatin, a dose-dependent increase in the activity of hepatic transaminases is observed in a small number of patients. In most cases it is minor, asymptomatic and temporary.
Laboratory indicators: when using the drug Crestor®, the following changes in laboratory indicators were also observed: increased concentrations of glucose, bilirubin, GGT activity, alkaline phosphatase, thyroid dysfunction.
The following side effects have been reported during post-marketing use of Crestor®:
From the hematopoietic system: unspecified frequency – thrombocytopenia.
From the digestive system: very rarely – jaundice, hepatitis; rarely – increased activity of liver transaminases; unspecified frequency – diarrhea.
From the musculoskeletal system: very rarely – arthralgia; unspecified frequency – immune-mediated necrotizing myopathy.
From the side of the central nervous system: very rarely – loss or decrease in memory; unspecified frequency – peripheral neuropathy.
From the respiratory system: unspecified frequency – cough, shortness of breath.
From the urinary system: very rarely – hematuria.
On the part of the skin and subcutaneous fat: unspecified frequency – Stevens-Johnson syndrome.
From the reproductive system and mammary gland: unspecified frequency – gynecomastia.
Other: unspecified frequency – peripheral edema.
The following side effects have been reported with some statins: depression, sleep disturbances, including insomnia and nightmares, sexual dysfunction, hyperglycemia, increased concentrations of glycosylated hemoglobin. Isolated cases of interstitial lung disease have been reported, especially with long-term use of the drugs.
Interaction
Interaction
Effect of the use of other drugs on rosuvastatin
Transport protein inhibitors: rosuvastatin binds to some transport proteins, in particular OATP1B1 and BCRP. Concomitant use of drugs that are inhibitors of these transport proteins may be accompanied by an increase in plasma concentrations of rosuvastatin and an increased risk of developing myopathy.
Cyclosporine: with simultaneous use of rosuvastatin and cyclosporine, the AUC of rosuvastatin was on average 7 times higher than the value observed in healthy volunteers. Does not affect plasma concentrations of cyclosporine. Crestor® is contraindicated in patients taking cyclosporine.
HIV protease inhibitors: Although the exact mechanism of interaction is unknown, coadministration of HIV protease inhibitors may result in a significant increase in rosuvastatin exposure. A pharmacokinetic study of co-administration of 20 mg rosuvastatin with a combination drug containing two HIV protease inhibitors (400 mg lopinavir/100 mg ritonavir) in healthy volunteers resulted in approximately two-fold and five-fold increases in rosuvastatin AUC0-24 and Cmax, respectively. Therefore, simultaneous use of rosuvastatin and HIV protease inhibitors is not recommended.
Gemfibrozil and other lipid-lowering drugs: the combined use of rosuvastatin and gemfibrozil leads to a 2-fold increase in the Cmax of rosuvastatin in blood plasma and the AUC of rosuvastatin. Based on specific interaction data, no pharmacokinetically significant interaction with fenofibrates is expected; pharmacodynamic interaction is possible.
Gemfibrozil, fenofibrate, other fibrates and lipid-lowering doses of niacin increased the risk of myopathy when used concomitantly with HMG-CoA reductase inhibitors, possibly due to the fact that they can cause myopathy when used as monotherapy. When taking the drug simultaneously with gemfibrozil, fibrates, nicotinic acid in lipid-lowering doses (more than 1 g/day), an initial dose of the drug of 5 mg is recommended for patients; taking a dose of 40 mg is contraindicated when co-administered with fibrates.
Ezetimibe: simultaneous use of Crestor® at a dose of 10 mg and ezetimibe at a dose of 10 mg was accompanied by an increase in the AUC of rosuvastatin in patients with hypercholesterolemia. An increased risk of side effects due to the pharmacodynamic interaction between Crestor® and ezetimibe cannot be excluded.
Antacids: simultaneous use of rosuvastatin and antacid suspensions containing magnesium and aluminum hydroxide leads to a decrease in plasma concentrations of rosuvastatin by approximately 50%. This effect is less pronounced if antacids are used 2 hours after taking rosuvastatin. The clinical significance of this interaction has not been studied.
Erythromycin: simultaneous use of rosuvastatin and erythromycin leads to a decrease in AUC of rosuvastatin by 20% and Cmax of rosuvastatin by 30%. This interaction may occur as a result of increased intestinal motility caused by erythromycin.
Cytochrome P450 isoenzymes: results of in vivo and in vitro studies have shown that rosuvastatin is neither an inhibitor nor an inducer of cytochrome P450 isoenzymes. In addition, rosuvastatin is a weak substrate for these isoenzymes. Therefore, interaction of rosuvastatin with other drugs at the metabolic level involving cytochrome P450 isoenzymes is not expected. There was no clinically significant interaction of rosuvastatin with fluconazole (an inhibitor of the CYP2C9 and CYP3A4 isoenzymes) and ketoconazole (an inhibitor of the CYP2A6 and CYP3A4 isoenzymes).
Fusidic acid: No studies have been conducted to study the interaction of rosuvastatin and fusidic acid. As with other statins, there have been post-marketing reports of rhabdomyolysis with co-administration of rosuvastatin and fusidic acid. Patients must be closely monitored. If necessary, it is possible to temporarily stop taking rosuvastatin.
Interactions with drugs that require dose adjustment of rosuvastatin
The dose of Crestor® should be adjusted if it is necessary to use it together with drugs that increase exposure to rosuvastatin. You should read the instructions for use of these drugs before prescribing them together with Crestor®. If an increase in exposure by 2 times or more is expected, the initial dose of Crestor® should be 5 mg 1 time / day. The maximum daily dose of Crestor should also be adjusted so that the expected exposure to rosuvastatin does not exceed that for a 40 mg dose taken without concomitant administration of drugs that interact with rosuvastatin. For example, the maximum daily dose of Crestor® when used simultaneously with gemfibrozil is 20 mg (increased exposure by 1.9 times), with ritonavir/atazanavir – 10 mg (increased exposure by 3.1 times).
Effect of rosuvastatin on other drugs
Vitamin K antagonists: Initiating rosuvastatin therapy or increasing the dose of the drug in patients receiving concomitant vitamin K antagonists (eg, warfarin) may lead to an increase in the International Normalized Ratio (IHR). Discontinuation of rosuvastatin or reduction of the drug dose may lead to a decrease in MHO. In such cases, MHO control is recommended.
Oral contraceptives/hormone replacement therapy: Concomitant use of rosuvastatin and oral contraceptives increases ethinyl estradiol AUC and norgestrel AUC by 26% and 34%, respectively. This increase in plasma concentration should be taken into account when selecting the dose; plasma concentration should be taken into account when selecting the dose of oral contraceptives. There are no pharmacokinetic data on the simultaneous use of Crestor® and hormone replacement therapy; therefore, a similar effect cannot be excluded when using this combination. However, this combination was widely used during clinical trials and was well tolerated by patients.
Other medicinal products: No clinically significant interaction between rosuvastatin and digoxin is expected.
Overdose
Overdose
When taking several daily doses simultaneously, the pharmacokinetic parameters of rosuvastatin do not change.
There is no specific treatment for rosuvastatin overdose. In case of overdose, it is recommended to carry out symptomatic treatment and measures aimed at maintaining the functions of vital organs and systems. Monitoring of liver function and CPK levels is necessary. It is unlikely that hemodialysis will be effective.
Storage conditions
Storage conditions
The drug should be stored out of the reach of children at a temperature not exceeding 30°C.
Shelf life
Shelf life
3 years. Do not use after the expiration date stated on the package.
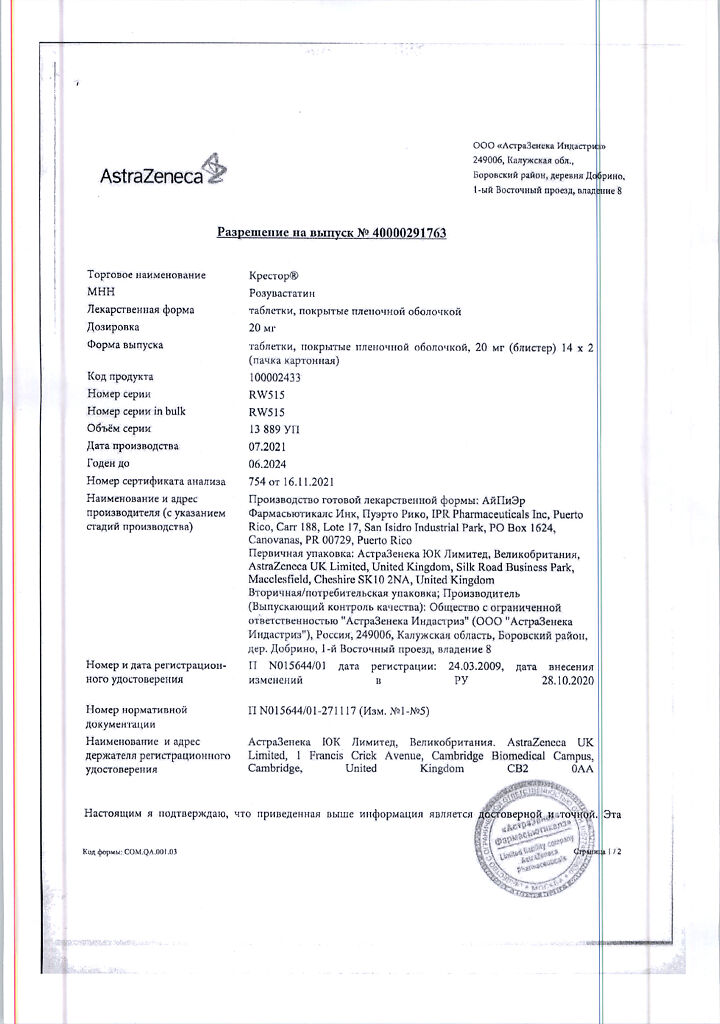
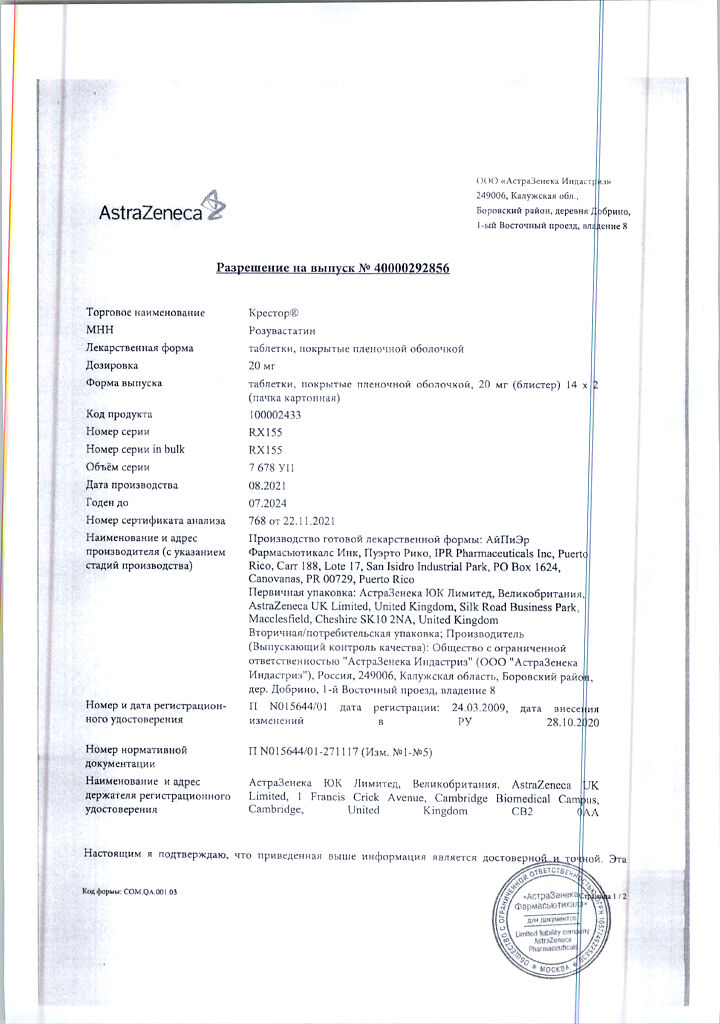
Manufacturer
Manufacturer
IPEr Pharmaceuticals Inc./AstraZeneca UK Limited, Puerto Rico
Additional information
| Shelf life | 3 years. Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | IPEr Pharmaceuticals Inc/AstraZeneca UK Limited, Puerto Rico |
| Medication form | pills |
| Brand | IPEr Pharmaceuticals Inc/AstraZeneca UK Limited |
Other forms…
Related products
Buy Crestor, 20 mg 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.