No products in the cart.
Cortisone, tablets 25 mg 80 pcs
€33.52 €29.05
Description
GCS. It has a significant effect on carbohydrate metabolism and, to a lesser extent, on water and electrolyte metabolism. It has mineralocorticoid activity: sodium retention, potassium loss, fluid retention in the body. Promotes glycogen accumulation in the liver, increases blood glucose content, increases urinary excretion of nitrogen. It has anti-inflammatory, desensitizing and anti-allergic effects, has immunosuppressive activity.
Inflammatory activity is caused by inhibition of phospholipase A2 which leads to inhibition of prostaglandin synthesis, decrease of macrophage chemotactic factor release, decrease of macrophages and lymphocytes migration to inflammation focus, stabilization of lysosomal membranes and prevention of lysosomal enzymes release.
The immunosuppressive action is associated with decrease of the number of immunocompetent cells, decrease of immunoglobulin binding to cell receptors, suppression of blast-transformation of B-lymphocytes, decrease of interleukins, lymphokines, circulating immunocomplexes, complement fractions.
increases excretion of calcium with urine, activates bone tissue lysis by mediated increase of calcitonin amount, increases osteoclast activity, decreases osteoblast function.
It has a catabolic effect, increases protein breakdown. Has a lipolytic effect and increases the content of fatty acids in the blood. It reduces the production of ACTH in the anterior pituitary lobe, which leads to suppression of activity and subsequent atrophy of the adrenal cortex.
Indications
Indications
Addison’s disease, secondary chronic insufficiency of the adrenal cortex (with hypopituitarism).
Allergic, inflammatory, infectious-allergic, autoimmune diseases.
Pharmacological effect
Pharmacological effect
GCS. It has a significant effect on carbohydrate metabolism and, to a lesser extent, on water and electrolyte metabolism. Has mineralocorticoid activity: sodium retention, potassium loss, fluid retention in the body. Promotes the accumulation of glycogen in the liver, increases blood glucose levels, and increases the excretion of nitrogen in the urine. It has anti-inflammatory, desensitizing and antiallergic effects, and has immunosuppressive activity.
The anti-inflammatory effect is due to inhibition of phospholipase A2, which leads to inhibition of prostaglandin synthesis, decreased release of macrophage chemotactic factor, decreased migration of macrophages and lymphocytes to the site of inflammation, stabilization of lysosome membranes and prevention of the release of lysosomal enzymes.
The immunosuppressive effect is associated with a decrease in the number of immunocompetent cells, with a decrease in the binding of immunoglobulins to cellular receptors, suppression of blast transformation of B-lymphocytes, a decrease in the number of interleukins, lymphokines, circulating immunocomplexes, and complement fractions.
Increases the excretion of calcium in the urine, activates bone tissue lysis by indirectly increasing the amount of calcitonin, increases the activity of osteoclasts, and reduces the function of osteoblasts.
It has a catabolic effect, increases the breakdown of proteins. Providing a lipolytic effect, it increases the content of fatty acids in the blood. Reduces the production of ACTH by the anterior pituitary gland, which leads to suppression of activity and subsequent atrophy of the adrenal cortex.
Special instructions
Special instructions
During treatment with Cortisone (especially long-term), observation by an ophthalmologist, monitoring of blood pressure, water and electrolyte balance, as well as peripheral blood patterns and blood glucose levels are necessary.
In order to reduce side effects, antacids can be prescribed, as well as increasing the intake of K + into the body (diet, potassium supplements). Food should be rich in proteins, vitamins, and limit the content of fats, carbohydrates and table salt.
The effect of the drug is enhanced in patients with hypothyroidism and liver cirrhosis.
The drug may worsen existing emotional instability or psychotic disorders. If a history of psychosis is indicated, cortisone in high doses is prescribed under the strict supervision of a physician.
In stressful situations during maintenance treatment (for example, surgery, trauma or infectious diseases), the dose of the drug should be adjusted due to an increased need for glucocorticosteroids.
With sudden withdrawal, especially in the case of previous use of high doses, it is possible to develop a “withdrawal syndrome” (Anorexia, nausea, lethargy, generalized musculoskeletal pain, general weakness), as well as an exacerbation of the disease for which Cortisone was prescribed.
During treatment with Cortisone, vaccination should not be carried out due to a decrease in its effectiveness (immune response).
When prescribing for intercurrent infections, septic conditions and tuberculosis, it is necessary to simultaneously treat with bactericidal antibiotics.
In children during long-term treatment with Cortisone, careful monitoring of the dynamics of growth and development is necessary. Children who during the treatment period were in contact with patients with measles or chickenpox are prescribed specific immunoglobulins prophylactically.
Due to the insufficiently expressed mineralocorticoid effect, cortisone is used in combination with mineralocorticoids for replacement therapy for adrenal insufficiency.
In patients with diabetes mellitus, blood glucose levels should be monitored and therapy adjusted if necessary.
X-ray monitoring of the osteoarticular system (images of the spine, hand) is indicated.
Cortisone in patients with latent infectious diseases of the kidneys and urinary tract can cause leukocyturia, which may have diagnostic value.
Cortisone increases the content of 11- and 17-hydroxyketocorticosteroid metabolites.
Active ingredient
Active ingredient
Cortisone
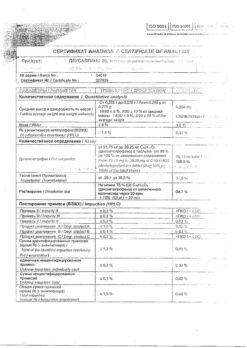
Composition
Composition
Active ingredient:
cortisone acetate 25 mg.
Excipients:
sugar,
potato starch,
stearic acid.
Contraindications
Contraindications
For short-term use for health reasons, the only contraindication is hypersensitivity to cortisone acetate or the components of the drug.
In children during the growth period, GCS should be used only for absolute indications and under the careful supervision of the attending physician. The drug should be prescribed with caution for the following diseases and conditions:
Diseases of the gastrointestinal tract – peptic ulcer of the stomach and duodenum, esophagitis, gastritis, acute or latent peptic ulcer, recently created intestinal anastomosis, ulcerative colitis with the threat of perforation or abscess formation, diverticulitis.
Parasitic and infectious diseases of a viral, fungal or bacterial nature (current or recently suffered, including recent contact with a patient) – herpes simplex, herpes zoster (viremic phase), chicken pox, measles; amebiasis, strongyloidiasis; systemic mycosis; active and latent tuberculosis. Use for severe infectious diseases is permissible only against the background of specific therapy.
Pre- and post-vaccination period (8 weeks before and 2 weeks after vaccination), lymphadenitis after BCG vaccination. Immunodeficiency conditions (including AIDS or HIV infection).
Diseases of the cardiovascular system, incl. recent myocardial infarction (in patients with acute and subacute myocardial infarction, the necrosis focus may spread, the formation of scar tissue may slow down and, as a result, the heart muscle will rupture), severe chronic heart failure, arterial hypertension, hyperlipidemia.
Endocrine diseases – diabetes mellitus (including impaired carbohydrate tolerance), thyrotoxicosis, hypothyroidism, Itsenko-Cushing’s disease, obesity (III-IV stage).
Severe chronic renal and/or liver failure, nephrourolithiasis. Hypoalbuminemia and conditions predisposing to its occurrence.
Systemic osteoporosis, myasthenia gravis, acute psychosis, poliomyelitis (except for the form of bulbar encephalitis), open- and closed-angle glaucoma.
Pregnancy.
Side Effects
Side Effects
The incidence and severity of side effects depends on the duration of use, the size of the dose used and the ability to comply with the circadian rhythm of Cortisone administration.
From the endocrine system:
Decreased glucose tolerance, steroid diabetes mellitus or manifestation of latent diabetes mellitus, suppression of adrenal function, Itsenko-Cushing syndrome (moon-shaped face, pituitary-type obesity, hirsutism, increased blood pressure, dysmenorrhea, amenorrhea, muscle weakness, stretch marks), delayed sexual development in children.
From the digestive system:
Nausea, vomiting, pancreatitis, steroid ulcer of the stomach and duodenum, erosive esophagitis, bleeding and perforation of the gastrointestinal tract, increased or decreased appetite, indigestion, flatulence, hiccups. In rare cases, increased activity of liver transaminases and alkaline phosphatase.
From the cardiovascular system:
Arrhythmias, bradycardia (up to cardiac arrest), development (in predisposed patients) or increased severity of heart failure, ECG changes characteristic of hypokalemia, increased blood pressure, hypercoagulation, thrombosis. In patients with acute and subacute myocardial infarction – the spread of necrosis, slowing down the formation of scar tissue, which can lead to rupture of the heart muscle.
From the nervous system:
Delirium, disorientation, euphoria, hallucinations, manic-depressive psychosis, Depression, paranoia, increased intracranial pressure, nervousness or anxiety, Insomnia, Dizziness, Vertigo, pseudotumor of the cerebellum, headache, convulsions.
From the senses:
Posterior subcapsular cataract, increased intraocular pressure with possible damage to the optic nerve, a tendency to develop secondary bacterial, fungal or viral eye infections, trophic changes in the cornea, exophthalmos.
From the side of metabolism:
Increased calcium excretion, hypocalcemia, weight gain, negative nitrogen balance (increased protein breakdown), increased sweating.
Caused by mineralocorticoid activity – fluid and sodium retention (peripheral edema), hypernatremia, hypokalemic syndrome (hypokalemia, arrhythmia, myalgia or muscle spasm, unusual weakness and fatigue).
From the musculoskeletal system:
Slowing of growth and ossification processes in children (premature closure of epiphyseal growth zones), osteoporosis (very rarely – pathological bone fractures, aseptic necrosis of the head of the humerus and femur), rupture of muscle tendons, steroid myopathy, decrease in muscle mass (atrophy).
From the skin and mucous membranes:
Delayed wound healing, petechiae, ecchymoses, skin thinning, hyper- or hypopigmentation, acne, stretch marks, tendency to develop pyoderma and candidiasis.
Allergic reactions:
Skin rash, itching, anaphylactic shock.
Others:
Development or exacerbation of infections (the appearance of this side effect is facilitated by jointly used immunosuppressants and vaccination), leukocyturia, withdrawal syndrome.
Interaction
Interaction
Simultaneous administration of Cortisone with:
Inducers of “liver” microsomal enzymes (phenobarbital, rifampicin, phenytoin, theophylline, ephedrine) lead to a decrease in its concentration.
Diuretics (especially thiazide and carbonic anhydrase inhibitors) and amphotericin B can lead to increased excretion of K + from the body, with sodium-containing drugs – edema and increased blood pressure.
Amphotericin B increases the risk of developing heart failure.
Cardiac glycosides impair their tolerability and increase the likelihood of developing ventricular extrasystole (due to hypokalemia caused).
Indirect anticoagulants weaken (less often enhance) their effect (dose adjustment required).
Anticoagulants and thrombolytics increase the risk of bleeding from ulcers in the gastrointestinal tract.
Ethanol and nonsteroidal anti-inflammatory drugs (NSAIDs) increase the risk of ulcerative lesions in the gastrointestinal tract and the development of bleeding (in combination with NSAIDs in the treatment of arthritis, it is possible to reduce the dose of glucocorticosteroids due to the summation of the therapeutic effect).
Paracetamol increases the risk of developing hepatotoxicity (induction of liver enzymes and the formation of a toxic metabolite of paracetamol).
Acetylsalicylic acid accelerates its elimination and reduces its concentration in the blood (when Cortisone is discontinued, the level of salicylates in the blood increases and the risk of side effects increases).
Insulin and oral hypoglycemic drugs, antihypertensive drugs reduce their effectiveness.
Vitamin D reduces its effect on the absorption of Ca 2+ in the intestine.
Growth hormone reduces the effectiveness of the latter, and praziquantel reduces its concentration.
M-anticholinergics (including antihistamines and tricyclic antidepressants) and nitrates increase intraocular pressure.
Isoniazid and mexelitine increases their metabolism (especially in “slow” acetylators), which leads to a decrease in their plasma concentrations.
Carbonic anhydrase inhibitors and loop diuretics may increase the risk of osteoporosis.
Indomethacin, displacing Cortisone from its connection with albumin, increases the risk of developing its side effects.
ACTH enhances the effect of Cortisone.
Ergocalciferol and parathyroid hormone prevent the development of osteopathy caused by Cortisone.
Cyclosporine and ketoconazole, by slowing down the metabolism of Cortisone, can in some cases increase its toxicity.
The simultaneous administration of androgens and steroidal anabolic drugs with Cortisone promotes the development of peripheral edema and hirsutism, and the appearance of acne.
Estrogens and oral contraceptives containing estrogen reduce the clearance of Cortisone, which may be accompanied by an increase in the severity of its action.
Mitotane and other inhibitors of adrenal function may necessitate an increase in the dose of cortisone.
When used simultaneously with live antiviral vaccines and against the background of other types of immunization, it increases the risk of viral activation and the development of infections.
Antipsychotics (neuroleptics) and azathioprine increase the risk of developing cataracts when cortisone is prescribed.
Simultaneous administration of antacids reduces the absorption of Cortisone.
When used simultaneously with antithyroid drugs, the clearance of Cortisone decreases and with thyroid hormones increases.
Overdose
Overdose
Symptoms: increased side effects.
Treatment: symptomatic.
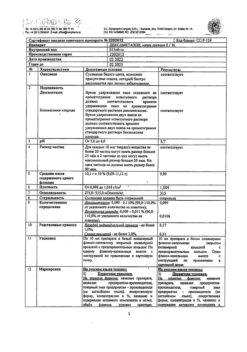
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
5 years
Manufacturer
Manufacturer
Akrikhin JSC, Russia
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | Akrihin HFC JSC, Russia |
| Medication form | pills |
| Brand | Akrihin HFC JSC |
Other forms…
Related products
Buy Cortisone, tablets 25 mg 80 pcs with delivery to USA, UK, Europe and over 120 other countries.