No products in the cart.
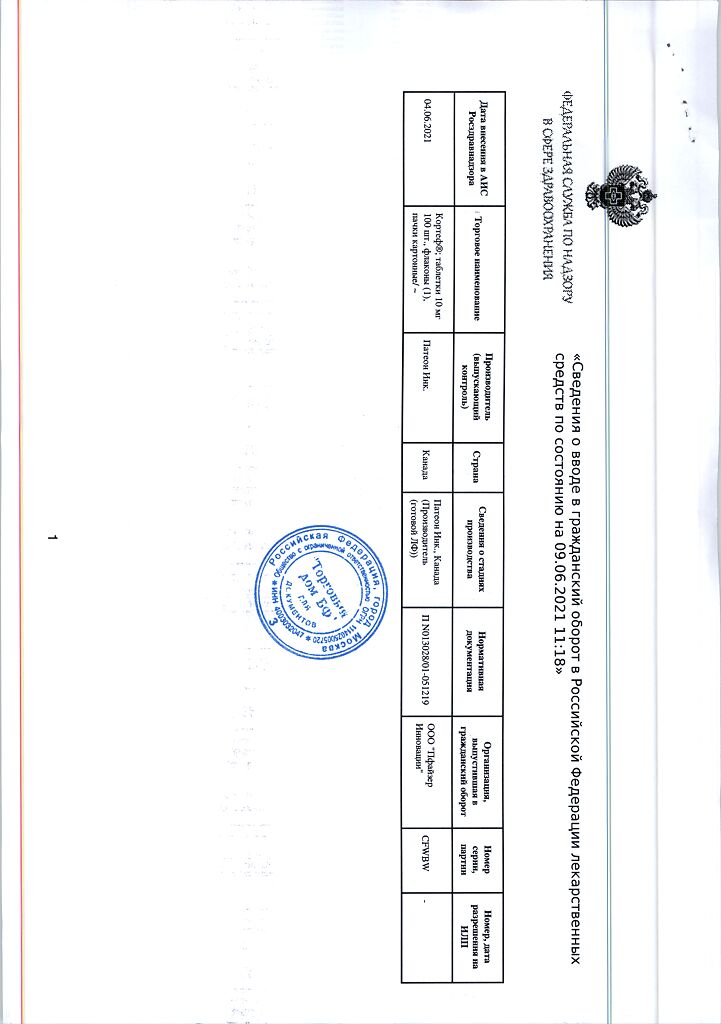
Cortef, tablets 10 mg 100 pcs
€14.86 €12.39
Description
Hydrocortisone, a synthetic analog of the natural glucocorticosteroid (GCS), has anti-inflammatory effects and is used for diseases of various organs and systems. It also has moderate mineralocorticoid properties and can be used for replacement therapy for adrenal cortex hormone deficiency conditions. Like other GCSs, hydrocortisone has a pronounced effect on various metabolic processes. In addition, hydrocortisone suppresses the body’s immune response.
Pharmacokinetics
Hydrocortisone is well absorbed from the gastrointestinal ‑tract (GIT) and reaches maximum concentration in blood approximately 1 hour after taking the drug. The plasma elimination half-life of hydrocortisone is about 100 min. More than 90% of hydrocortisone is bound to plasma proteins.
Hydrocortisone is metabolized in the liver and most body tissues to hydrogenated and degraded forms such as tetrahydrocortisone and tetrahydrocortisol, which are excreted by the kidneys, mainly as glucuronides; in addition, a very small portion of hydrocortisone is excreted unchanged by the kidneys.
Hydrocortisone readily passes through the placenta.
Indications
Indications
In endocrinology
– adrenal insufficiency (hydrocortisone is the drug of choice for replacement therapy): primary (Addison’s disease), usually in combination with mineralocorticoids; secondary (usually without the addition of mineralocorticoids);
— congenital adrenal hyperplasia;
— subacute thyroiditis;
— hypercalcemia in malignant neoplasms.
In rheumatology
As an additional short-term therapy (during an acute attack or exacerbation) for:
— psoriatic arthritis;
– rheumatoid arthritis, including juvenile rheumatoid arthritis (in some cases, low-dose maintenance therapy may be required);
— ankylosing spondylitis;
– acute and subacute bursitis;
— acute nonspecific tenosynovitis;
— acute gouty arthritis;
— post-traumatic osteoarthritis;
— synovitis with osteoarthritis;
– epicondylitis.
During exacerbations or as maintenance therapy in selected cases with:
— systemic lupus erythematosus;
– systemic dermatomyositis (polymyositis);
— acute rheumatic carditis.
In dermatology
– pemphigus;
— bullous dermatitis herpetiformis;
– severe erythema multiforme (Stevens-Johnson syndrome);
— exfoliative dermatitis;
— mycosis fungoides (Aliber’s disease);
– severe psoriasis;
— severe seborrheic dermatitis.
In allergology
Control of severe or disabling allergic conditions that cannot be adequately treated with appropriate medications:
— seasonal or year-round allergic rhinitis;
— serum sickness;
— bronchial asthma;
— contact dermatitis;
— atopic dermatitis;
— hypersensitivity reactions to drugs.
In ophthalmology
Severe acute and chronic allergic and inflammatory diseases involving the eyeball and its appendages, such as:
— allergic conjunctivitis;
— keratitis;
– allergic corneal ulcers;
– eye damage due to herpes zoster;
– iritis and iridocyclitis;
— chorioretinitis;
– inflammatory diseases of the anterior segment of the eye;
— diffuse posterior uveitis and choroiditis;
– neuritis of the optic nerve;
– sympathetic ophthalmia.
In pulmonology
– symptomatic sarcoidosis;
– Loeffler’s syndrome, not treatable by other means;
— berylliosis;
– fulminant or disseminated pulmonary tuberculosis in combination with appropriate anti-tuberculosis chemotherapy;
— aspiration pneumonia.
In hematology
— idiopathic thrombocytopenic purpura in adults;
– secondary thrombocytopenia in adults;
— acquired (autoimmune) hemolytic anemia;
— erythroblastopenia (erythrocyte anemia);
— congenital (erythroid) hypoplastic anemia.
In oncology
For palliative care:
— leukemia and lymphoma in adults;
— acute leukemia in children.
In nephrology
– to stimulate diuresis or remission of proteinuria in nephrotic syndrome without uremia, idiopathic type or due to systemic lupus erythematosus.
In neuroscience
– exacerbation of multiple sclerosis.
Other indications for use
– tuberculous meningitis with subarachnoid block or when there is a threat of block: the drug is used simultaneously with appropriate anti-tuberculosis chemotherapy.
Pharmacological effect
Pharmacological effect
Hydrocortisone, a synthetic analogue of the natural glucocorticosteroid (GCS), has an anti-inflammatory effect and is used for diseases of various organs and systems. It also has moderate mineralocorticoid properties and can be used for replacement therapy in conditions of adrenal hormone deficiency. Like other corticosteroids, hydrocortisone has a pronounced effect on various metabolic processes. In addition, hydrocortisone suppresses the body’s immune response.
Pharmacokinetics
Hydrocortisone is well absorbed from the gastrointestinal tract (GIT), the maximum concentration in the blood is reached approximately 1 hour after taking the drug. The plasma half-life of hydrocortisone is about 100 minutes. More than 90% of hydrocortisone is bound to plasma proteins.
Hydrocortisone is metabolized in the liver and most body tissues to hydrogenated and degraded forms, such as tetrahydrocortisone and tetrahydrocortisol, which are excreted by the kidneys, mainly in the form of glucuronides, in addition, a very small part of hydrocortisone is excreted unchanged by the kidneys.
Hydrocortisone easily crosses the placenta.
Special instructions
Special instructions
For patients who may be exposed to stress during GCS therapy, fast-acting GCS drugs are indicated in increased doses before, during and after a stressful situation.
During GCS therapy, some infections may occur in an erased form, in addition, new infections may develop. When using GCS, a decrease in resistance to infections is possible, and the body’s ability to localize the infectious process is also reduced. The development of infections caused by various pathogenic organisms, such as viruses, bacteria, fungi, protozoa or helminths, which are localized in various systems of the human body, may be associated with the use of GCS, both as monotherapy and in combination with other immunosuppressants affecting cellular immunity, humoral immunity or neutrophil function. These infections may not be severe, but in some cases they can be severe and even fatal. Moreover, the higher doses of GCS are used, the higher the likelihood of developing infectious complications.
For eye damage caused by the herpes simplex virus, GCS should be prescribed with caution, as this can lead to corneal perforation.
Long-term use of GCS can lead to posterior subcapsular cataracts, glaucoma with possible damage to the optic nerve and provoke the addition of a secondary ocular fungal or viral infection.
Moderate to large doses of hydrocortisone may cause increased blood pressure, electrolyte and fluid retention, and increased potassium excretion. These effects are less likely to occur with synthetic analogues, unless used in high doses. It is necessary to limit salt intake from food and prescribe potassium supplements. All corticosteroids increase calcium excretion.
In patients receiving treatment with corticosteroids in doses that have an immunosuppressive effect, the administration of live or live attenuated vaccines is contraindicated, but killed or inactivated vaccines can be administered, however, the response to the introduction of such vaccines may be reduced. Patients receiving treatment with GCS in doses that do not have an immunosuppressive effect can be immunized according to appropriate indications.
The use of the drug in active tuberculosis should be limited to cases of fulminant and disseminated tuberculosis, when GCS are used to treat the disease in combination with appropriate anti-tuberculosis chemotherapy.
If the drug is prescribed to patients with latent tuberculosis or with positive tuberculin tests, then treatment should be carried out under strict medical supervision, since reactivation of the disease is possible. During long-term drug therapy, such patients should receive appropriate preventive treatment.
Patients receiving drugs that suppress the immune system are more susceptible to infections than healthy individuals. For example, chickenpox and measles can be more severe, even fatal, in unimmunized children or in adults receiving corticosteroids. In such children or adults who do not yet have the disease, measures should be taken to prevent contact with sick people. It is unknown how the dosage, route of administration and duration of treatment with GCS affect the risk of developing disseminating infection. The role of the underlying disease and/or prior treatment with corticosteroids in the risk of infection is also unknown. For chickenpox infection, prophylactic administration of VZIG (varicella zoster serotherapy immunoglobulin) may be indicated. If exposed to measles, intramuscular immunoglobulin (IgG) may be given (see VZIG and IgG instructions for more complete information). If chickenpox develops, treatment with antiviral drugs should be considered. GCS should also be prescribed with great caution to patients with confirmed or suspected strongyloidiasis. Immunosuppression caused by GCS in such patients leads to strongyloid hyperinfection and dissemination of the process with widespread migration of larvae, often with the development of severe forms of enterocolitis and gram-negative septicemia with possible death.
Information for patients: persons receiving corticosteroids in immunosuppressive doses should avoid contact with patients with chickenpox or measles; patients should be informed that if exposed they should seek immediate medical attention.
Secondary adrenal insufficiency caused by the drug can be minimized by gradually reducing the dose. This type of relative insufficiency can continue for several months after the end of treatment, therefore, in any stressful situations during this period, GCS should be re-prescribed. Since mineralocorticoid secretion may be impaired, concomitant administration of electrolytes and/or mineralocorticoids is necessary.
In patients with hypothyroidism and liver cirrhosis, the effect of GCS is enhanced. To control the condition after treatment, the minimum possible doses of GCS should be prescribed, and the dose reduction should be carried out gradually.
During GCS therapy, the development of various mental disorders is possible: from euphoria, insomnia, mood instability, personality changes and severe depression to acute psychotic manifestations. In addition, existing emotional instability or psychotic tendencies may be exacerbated.
When prescribing long-term treatment with GCS, newborns and children should carefully monitor their growth and development.
Kaposi’s sarcoma has been reported in patients receiving GCS therapy. When GCS is discontinued, clinical remission may occur.
Despite the fact that controlled clinical studies have shown the effectiveness of GCS for the rapid relief of exacerbation of multiple sclerosis, the effect of GCS on the course of the disease or disease outcome has not been identified. Studies have shown that in these cases, in order to achieve a pronounced therapeutic effect, it is necessary to prescribe high doses of GCS drugs (see section “Method of administration and doses”).
Since the complications of GCS therapy depend on the dose and duration of treatment, in each specific case, based on an analysis of the risk/benefit ratio, a decision is made on the need for such treatment, and the duration of treatment and frequency of administration are determined.
Impact on the ability to drive vehicles and machinery
Due to the possibility of dizziness, convulsions and a decrease in blood pressure, Cortef® should be prescribed with caution to persons driving vehicles and engaged in activities that require increased concentration and rapid motor response.
Active ingredient
Active ingredient
Hydrocortisone
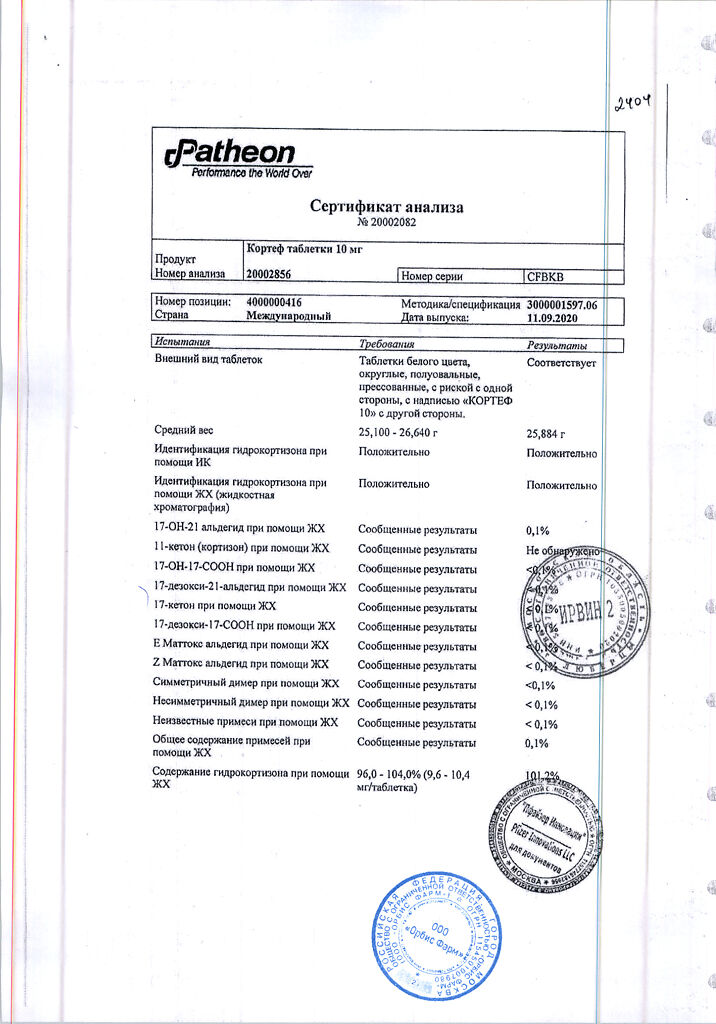
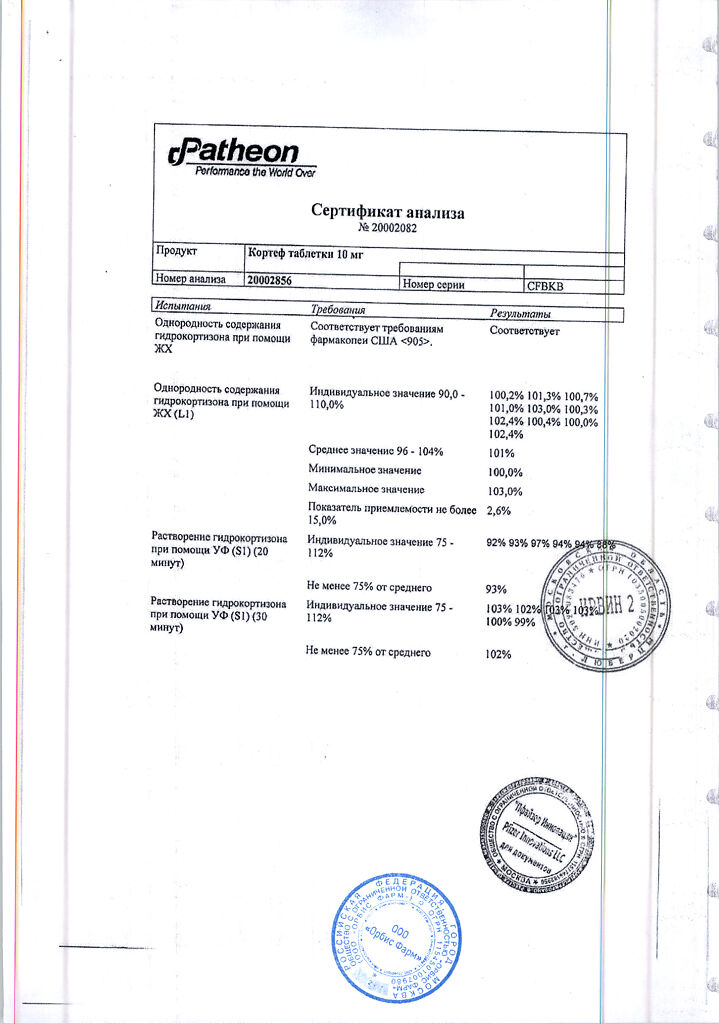
Composition
Composition
1 tab. contains hydrocortisone 10 mg.
Excipients:
Pregnancy
Pregnancy
Since relevant studies of the effect of GCS on human reproductive function have not yet been conducted, the use of these drugs during pregnancy, nursing mothers or women of childbearing age requires an assessment of the likely positive effect of the drug in comparison with the potential risk to the mother, embryo or fetus.
Children born to mothers who received significant doses of corticosteroids during pregnancy should be carefully examined to identify possible symptoms of adrenal hypofunction.
Contraindications
Contraindications
Systemic fungal infections.
History of hypersensitivity to any component of the drug.
With caution
Nonspecific ulcerative colitis with threat of perforation, abscess, or other purulent infection; diverticulitis; intestinal anastomosis (in immediate history); acute or latent peptic ulcer, gastric or duodenal ulcer, esophagitis, gastritis; osteoporosis; myasthenia gravis; hypoalbuminemia and conditions predisposing to its occurrence, including cirrhosis of the liver; renal failure; diabetes mellitus (including impaired carbohydrate tolerance), thyrotoxicosis, Itsenko-Cushing’s disease, hypothyroidism; acute psychosis; herpes simplex (eye form); strongyloidiasis; chicken pox, measles, active or latent tuberculosis, severe bacterial or viral infectious diseases (increases the risk of developing superinfection, masks the symptoms of the disease, the drug can only be used against the background of specific antimicrobial therapy), glaucoma, AIDS, HIV infection; arterial hypertension; acute and subacute myocardial infarction.
Side Effects
Side Effects
The side effects listed below are typical for all GCS.
The incidence and severity of side effects depend on the duration of use, the size of the dose used and the possibility of taking it in accordance with the circadian rhythm.
From the endocrine system: suppression of adrenal function, secondary areactivity of the adrenal glands and pituitary gland of various origins, development of Cushing’s syndrome, menstrual irregularities, decreased glucose tolerance, manifestation of latent diabetes mellitus, increased need for insulin or oral hypoglycemic agents in patients with diabetes.
From the digestive system: peptic ulcer with possible perforation and bleeding, pancreatitis (nausea, vomiting), bloating, erosive/ulcerative esophagitis.
After treatment with GCS, an increase in the activity of alanine transaminase (ALT), aspartate transaminase (AST) and alkaline phosphatase in the blood serum was observed. Usually these changes are minor, are not associated with any clinical syndromes and are reversible after cessation of treatment.
From the cardiovascular system: chronic heart failure in patients with a corresponding predisposition, increased blood pressure, in patients with acute and subacute myocardial infarction – the spread of necrosis, slowing down the formation of scar tissue, which can lead to rupture of the heart muscle.
From the nervous system: increased intracranial pressure with swelling of the optic disc (pseudotumor cerebri), especially after treatment, convulsions, dizziness, headache, delirium, disorientation, euphoria, hallucinations, manic-depressive psychosis, depression, paranoia.
From the senses: posterior subcapsular cataract, increased intraocular pressure, glaucoma with possible damage to the optic nerve, exophthalmos, tendency to develop secondary bacterial, fungal or viral eye infections.
From the metabolic side: negative nitrogen balance due to protein catabolism.
Caused by MCS activity: sodium and fluid retention in the body, hypokalemic alkalosis, muscle weakness, potassium loss.
From the musculoskeletal system: “steroid” myopathy, decreased muscle mass, osteoporosis, tendon ruptures, especially the Achilles tendon, vertebral compression fractures, aseptic necrosis of the epiphyses of the femur and humerus, pathological fractures of long bones, growth retardation in children.
From the skin: slow wound healing, thinning and decreased strength of the skin, petechiae, ecchymosis, facial erythema, possible suppression of the reaction to skin tests, hirsutism, increased sweating.
Allergic reactions: generalized (skin rash/urticaria).
When using other GCS, there are reports of the following side effects: increased appetite, hiccups, arrhythmias, hypercoagulation, thrombosis, trophic changes in the cornea, increased calcium excretion, hypocalcemia, development or exacerbation of infections (the appearance of this side effect is facilitated by jointly used immunosuppressants and vaccination). There are currently no reports of the above side effects when using the drug Cortef®.
Interaction
Interaction
Drugs that activate liver enzymes, such as phenobarbital, phenytoin, and rifampicin, may increase the clearance of hydrocortisone, which may require increasing the drug dose to obtain the desired effect.
Drugs such as troleandomycin and ketoconazole can inhibit the metabolism of GCS and reduce its clearance. In this case, the dose of GCS should be reduced to avoid overdose phenomena.
GCS may increase the clearance of acetylsalicylic acid taken in high doses over a long period, which may lead to a decrease in serum salicylate concentrations or increase the risk of salicylate toxicity when GCS is discontinued. In patients with hypoprothrombinemia, acetylsalicylic acid should be prescribed in combination with GCS with caution.
Both increased and decreased effects of oral anticoagulants taken concomitantly with corticosteroids have been reported. To maintain the required effect of the anticoagulant, constant determination of coagulation parameters is necessary.
When used simultaneously with live antiviral vaccines and against the background of other types of immunization, GCS increases the risk of viral activation and the development of infections.
GCS accelerate the metabolism of isoniazid and mexiletine, which leads to a decrease in their plasma concentrations.
Increases the risk of developing the hepatotoxic effect of paracetamol due to the induction of “liver” enzymes and the formation of a toxic metabolite of paracetamol.
With long-term GCS therapy, higher doses of folic acid may be required.
Hypokalemia caused by GCS can increase the severity and duration of muscle blockade while taking muscle relaxants.
In high doses, GCS reduce the effect of somatropin.
Hydrocortisone reduces the effect of hypoglycemic drugs.
Sodium-containing medications increase the risk of edema and increased blood pressure.
Nonsteroidal anti-inflammatory drugs (NSAIDs) and ethanol increase the risk of developing ulceration of the gastrointestinal mucosa and bleeding, however, when using GCS in combination with NSAIDs for the treatment of arthritis, the therapeutic effect increases, so it is possible to reduce the dose of GCS.
When used together with mitotane and other inhibitors of adrenal cortex function, it may be necessary to increase the dose of GCS.
While taking corticosteroids, immunosuppressants increase the risk of developing infections and lymphoma or other lymphoproliferative disorders caused by the Epstein-Barr virus.
Concomitant use of androgens or anabolic steroids may increase the risk of edema and lead to acne.
Combined use with m-anticholinergics increases intraocular pressure.
GCS increase the toxicity of cardiac glycosides (due to the resulting hypokalemia, the risk of developing arrhythmias increases), weaken the effect of vitamin D on the absorption of calcium in the intestinal lumen.
Thiazide diuretics, carbonic anhydrase inhibitors, other corticosteroids and amphotericin B increase the risk of hypokalemia.
Indomethacin, displacing GCS from its connection with albumin, increases the risk of developing their side effects.
Amphotericin B and carbonic anhydrase inhibitors increase the risk of osteoporosis.
The clearance of GCS increases with the use of drugs – thyroid hormones.
Estrogens (including oral estrogen-containing contraceptives) reduce the clearance of corticosteroids, prolong their half-life and therapeutic and toxic effects.
Tricyclic antidepressants may increase the severity of depression caused by taking corticosteroids (not indicated for the treatment of these side effects).
The risk of developing cataracts increases when used in combination with other corticosteroids, antipsychotic drugs (neuroleptics), carbutamide and azathioprine.
Overdose
Overdose
The clinical syndrome of acute drug overdose has not been described. Reports of cases of acute toxicity following an overdose of GCS are extremely rare. There is no specific antidote. Treatment is symptomatic. Hydrocortisone is eliminated by dialysis.
Storage conditions
Storage conditions
The drug should be stored out of the reach of children at controlled room temperature (20° to 25°C).
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Patheon Inc., Canada
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | The drug should be kept out of reach of children at controlled room temperature (20° to 25°C). |
| Manufacturer | Pateon Inc, Canada |
| Medication form | pills |
| Brand | Pateon Inc |
Related products
Buy Cortef, tablets 10 mg 100 pcs with delivery to USA, UK, Europe and over 120 other countries.