No products in the cart.
Coronal, 5 mg 100 pcs
€8.38 €7.33
Description
A selective beta1-adrenoblocker. Reduces plasma renin activity, reduces myocardial oxygen demand, reduces HR (at rest and under load). It has antihypertensive, antiarrhythmic and antianginal effects. In low doses it blocks β1-adrenoceptors of heart, reduces catecholamine-stimulated formation of cAMP from ATP, decreases intracellular calcium ion current, produces negative chrono-, dromo-, batmo- and inotropic effect (decreases heart rate, inhibits conduction and excitability, reduces myocardial contractility). With increasing dose has beta2-adrenoblocking effect.
The HRP at the beginning of the drug administration, in the first 24 hours after oral administration, increases (as a result of reciprocal increase of α-adrenoreceptor activity and elimination of β2-adrenoreceptor stimulation) which returns to baseline after 1-3 days, and decreases with prolonged administration.
The antihypertensive effect is associated with the reduction of the minute blood volume, sympathetic stimulation of peripheral vessels, reduction of the RAAS activity (of greater importance for patients with initial renin hypersecretion) and CNS, restoration of aortic arch baroreceptors sensitivity (their activity in response to BP decrease is not increased) and finally reduction of peripheral sympathetic effects. In arterial hypertension hypotensive effect develops in 2-5 days, stable effect – in 1-2 months.
The antianginal effect is caused by decrease of myocardial oxygen demand as a result of HR shortening and decrease of contractility, prolongation of diastole, improvement of myocardial perfusion and decrease of myocardial sensitivity to sympathetic innervation. It reduces the number and severity of angina attacks and increases exercise tolerance. By increasing left ventricular end-diastolic pressure and increasing ventricular muscle fiber stretch, oxygen demand may increase, especially in patients with chronic heart failure.
. Antiarrhythmic action is caused by the removal of arrhythmogenic factors (tachycardia, increased activity of the sympathetic nervous system, increased content of CAMF, arterial hypertension), the decrease of spontaneous excitation rate of sinus and ectopic pacemakers and slowing of AV conduction (mainly in antegrade and, to a lesser extent, in retrograde direction through AV node) and conduction through additional pathways.
When used in medium therapeutic doses, unlike non-selective beta-adrenoblockers, it has less pronounced effect on organs containing β2-adrenoreceptors (pancreas, skeletal muscles, smooth muscles of peripheral arteries, bronchi and uterus) and on carbohydrate metabolism, does not cause retention of sodium ions in the body. When used in high doses (200 mg and more) it has a blocking effect on both subtypes of β-adrenoreceptors, mainly in the bronchi and vascular smooth muscle.
Indications
Indications
– arterial hypertension;
— IHD: prevention of angina attacks.
Pharmacological effect
Pharmacological effect
Selective beta1-blocker. Reduces plasma renin activity, reduces myocardial oxygen demand, and reduces heart rate (at rest and during exercise). It has antihypertensive, antiarrhythmic and antianginal effects. By blocking β1-adrenergic receptors of the heart in low doses, it reduces the formation of cAMP from ATP stimulated by catecholamines, reduces the intracellular current of calcium ions, has a negative chrono-, dromo-, bathmo- and inotropic effect (reduces heart rate, inhibits conductivity and excitability, reduces myocardial contractility). With increasing dose, it has a beta2-adrenergic blocking effect.
OPSS at the beginning of the drug use, in the first 24 hours after oral administration, increases (as a result of a reciprocal increase in the activity of α-adrenergic receptors and the elimination of stimulation of β2-adrenergic receptors), which returns to the original level after 1-3 days, and decreases with long-term administration.
The antihypertensive effect is associated with a decrease in minute blood volume, sympathetic stimulation of peripheral vessels, a decrease in the activity of the RAAS (more important for patients with initial hypersecretion of renin) and the central nervous system, restoration of the sensitivity of the baroreceptors of the aortic arch (there is no increase in their activity in response to a decrease in blood pressure) and, ultimately, a decrease in peripheral sympathetic influences. In arterial hypertension, the hypotensive effect develops after 2-5 days, a stable effect – after 1-2 months.
The antianginal effect is due to a decrease in myocardial oxygen demand as a result of a decrease in heart rate and decreased contractility, prolongation of diastole, improved myocardial perfusion, as well as a decrease in the sensitivity of the myocardium to the effects of sympathetic innervation. Reduces the number and severity of angina attacks and increases exercise tolerance. Due to increased end-diastolic pressure in the left ventricle and increased stretch of ventricular muscle fibers, oxygen demand may increase, especially in patients with chronic heart failure.
The antiarrhythmic effect is due to the elimination of arrhythmogenic factors (tachycardia, increased activity of the sympathetic nervous system, increased cAMP content, arterial hypertension), a decrease in the rate of spontaneous excitation of sinus and ectopic pacemakers and a slowdown in AV conduction (mainly in the antegrade and, to a lesser extent, in the retrograde directions through the AV node) and conduction along additional pathways.
When used in average therapeutic doses, in contrast to non-selective beta-blockers, it has a less pronounced effect on organs containing β2-adrenergic receptors (pancreas, skeletal muscles, smooth muscles of peripheral arteries, bronchi and uterus) and on carbohydrate metabolism, does not cause sodium ion retention in the body. When used in high doses (200 mg or more), it has a blocking effect on both subtypes of β-adrenergic receptors, mainly in the bronchi and vascular smooth muscles.
Special instructions
Special instructions
When prescribing Coronal, you should regularly monitor heart rate and blood pressure (at the beginning of treatment – daily, then once every 3-4 months), perform an ECG, and determine the blood glucose level in patients with diabetes (once every 4-5 months). In elderly patients, it is recommended to monitor renal function (once every 4-5 months).
The patient should be trained in the method of calculating heart rate and instructed about the need for medical consultation if the heart rate is less than 50 beats/min.
Before starting treatment, it is recommended to conduct a study of external respiratory function in patients with a burdened bronchopulmonary history.
It should be taken into account that in approximately 20% of patients with angina, beta-blockers are ineffective due to severe coronary atherosclerosis with a low ischemic threshold (heart rate less than 100 beats/min) and increased end-diastolic volume of the left ventricle, which impairs subendocardial blood flow.
In smoking patients, the effectiveness of beta-blockers is reduced.
Patients using contact lenses should take into account that during treatment the production of tear fluid may decrease.
When using Coronal in patients with pheochromocytoma, there is a risk of developing paradoxical arterial hypertension (if effective alpha-blockade is not previously achieved).
Bisoprolol may mask certain clinical signs of thyrotoxicosis (eg, tachycardia). Abrupt withdrawal of Coronal in patients with thyrotoxicosis is contraindicated, as it can increase the symptoms of the disease.
In diabetes mellitus, bisoprolol can mask tachycardia caused by hypoglycemia. Unlike non-selective beta-blockers, it practically does not enhance insulin-induced hypoglycemia and does not delay the restoration of blood glucose concentrations to normal levels.
When used simultaneously with clonidine, the latter can be discontinued only a few days after discontinuation of the drug Coronal.
It is possible that the severity of the hypersensitivity reaction may increase and there will be no effect from usual doses of epinephrine against the background of a burdened allergic history.
If planned surgical treatment is necessary, the drug should be discontinued 48 hours before the start of general anesthesia. If the patient took the drug before surgery, he should select a drug for general anesthesia with minimal negative inotropic effect.
Reciprocal activation of the vagus nerve can be eliminated by intravenous atropine (1-2 mg).
Medicines that reduce the supply of catecholamines (including reserpine) can enhance the effect of beta-blockers, so patients taking such combinations of drugs should be under constant medical supervision to detect a pronounced decrease in blood pressure or bradycardia.
Patients with concomitant bronchospastic diseases can be prescribed cardioselective adrenergic blockers in case of intolerance and/or ineffectiveness of other antihypertensive drugs. An overdose is dangerous due to the development of bronchospasm.
If increasing bradycardia (less than 50 beats/min), a pronounced decrease in blood pressure (systolic blood pressure below 100 mm Hg), or AV blockade occurs in elderly patients, it is necessary to reduce the dose or stop treatment.
It is recommended to discontinue therapy if depression develops.
The drug should be discontinued before testing the content of catecholamines, normetanephrine, vanillinmandelic acid, and antinuclear antibody titers in the blood and urine.
Treatment should not be abruptly interrupted due to the risk of developing severe arrhythmias and myocardial infarction. Cancellation is carried out gradually, reducing the dose over 2 weeks or more (the dose is reduced by 25% in 3-4 days).
Use in pediatrics
The use of the drug Coronal in children and adolescents under the age of 18 is contraindicated, because efficacy and safety have not been established.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Bisoprolol
Composition
Composition
1 tab.:
Pregnancy
Pregnancy
During pregnancy, Coronal is prescribed only for strict indications if the expected benefit to the mother outweighs the potential risk to the fetus.
72 hours before birth, taking Coronal should be stopped due to the possible development of bradycardia, arterial hypotension, hypoglycemia and respiratory depression in the fetus/newborn.
If taking Coronal is necessary during lactation, breastfeeding should be stopped.
When taking bisoprolol during pregnancy, the fetus may experience intrauterine growth retardation, hypoglycemia, and bradycardia.
Contraindications
Contraindications
— shock (including cardiogenic);
– acute heart failure;
— chronic heart failure in the stage of decompensation;
— AV blockade II and III degrees (without artificial pacemaker);
– sinoatrial blockade;
— SSSU;
– severe bradycardia;
– cardiomegaly (without signs of heart failure);
– arterial hypotension (systolic blood pressure below 100 mm Hg, especially during myocardial infarction);
– history of bronchial asthma and chronic obstructive pulmonary disease;
– simultaneous use of MAO inhibitors (with the exception of MAO type B inhibitors);
– concomitant use of floctafenine and sultopride;
— late stages of peripheral circulatory disorders;
– Raynaud’s disease;
– lactation period;
– age under 18 years (efficacy and safety have not been established);
– hypersensitivity to the components of the drug and other beta-blockers.
The drug should be prescribed with caution in case of liver failure, renal failure (creatinine clearance less than 20 ml/min), metabolic acidosis, pheochromocytoma (with concomitant use of alpha-blockers), diabetes mellitus in the stage of decompensation, AV blockade of the first degree, Prinzmetal’s angina, restrictive cardiomyopathy, congenital heart defects or heart valve defects with severe hemodynamic disorders, chronic heart failure with myocardial infarction within the last 3 months, psoriasis, depression (including a history), history of severe allergic reactions, during pregnancy, following a strict diet, desensitizing immunotherapy with allergens and allergen extracts, as well as in elderly patients.
Side Effects
Side Effects
The incidence of side effects is determined as follows: very often (≥1/10), often (≥1/100 and
From the side of the central nervous system: infrequently – increased fatigue, asthenia, dizziness, headache, drowsiness or insomnia, depression; rarely – hallucinations, nightmares, convulsions.
From the senses: rarely – blurred vision, decreased secretion of tear fluid, dry and sore eyes, hearing impairment; very rarely – conjunctivitis.
From the cardiovascular system: very often – sinus bradycardia; often – decreased blood pressure, manifestation of vasospasm (increased peripheral circulatory disorders, coldness of the lower extremities, paresthesia); uncommon – impaired AV conduction, orthostatic hypotension, decompensation of chronic heart failure, peripheral edema.
From the digestive system: often – dryness of the oral mucosa, nausea, vomiting, diarrhea, constipation; rarely – hepatitis, increased activity of liver transaminases.
From the respiratory system: infrequently – difficulty breathing when prescribed in high doses (loss of selectivity) and/or in predisposed patients – laryngo- and bronchospasm; rarely – nasal congestion, allergic rhinitis.
From the endocrine system: rarely – hyperglycemia (in patients with type 2 diabetes mellitus), hypoglycemia (in patients receiving insulin).
Allergic reactions: rarely – itching, rash, urticaria.
From the skin: rarely – increased sweating, skin hyperemia; very rarely – psoriasis-like skin reactions, exacerbation of psoriasis symptoms, alopecia.
From the musculoskeletal system: infrequently – muscle weakness, cramps in the calf muscles, arthralgia.
From the hematopoietic organs: in some cases – thrombocytopenia, agranulocytosis.
Other: very rarely – impaired potency; rarely – hypertriglyceridemia, withdrawal syndrome (increased angina attacks, increased blood pressure).
Interaction
Interaction
Allergens used for immunotherapy or allergen extracts for skin testing increase the risk of severe systemic allergic reactions or anaphylaxis in patients receiving bisoprolol.
When used simultaneously with Coronal, iodine-containing radiopaque drugs for intravenous administration increase the risk of developing anaphylactic reactions.
When used simultaneously with Coronal, phenytoin for intravenous administration and drugs for inhalation general anesthesia (hydrocarbon derivatives) increase the severity of the cardiodepressive effect and the likelihood of lowering blood pressure.
When used simultaneously, Coronal changes the effectiveness of insulin and oral hypoglycemic drugs, masks the symptoms of developing hypoglycemia (tachycardia, increased blood pressure).
With simultaneous use, Coronal reduces the clearance of lidocaine and xanthines (except diphylline) and increases their concentration in plasma, especially in patients with initially increased clearance of theophylline under the influence of smoking.
NSAIDs (due to the retention of sodium ions and blockade of prostaglandin synthesis by the kidneys), corticosteroids and estrogens (due to the retention of sodium ions) weaken the antihypertensive effect of Coronal.
When used simultaneously with Coronal, cardiac glycosides, methyldopa, reserpine and guanfacine, slow calcium channel blockers (verapamil, diltiazem), amiodarone and other antiarrhythmic drugs increase the risk of developing or worsening bradycardia, AV block, cardiac arrest and heart failure.
When used simultaneously with Coronal, nifedipine can lead to a significant decrease in blood pressure.
When used simultaneously with Coronal, diuretics, clonidine, sympatholytics, hydralazine and other antihypertensive drugs can lead to an excessive decrease in blood pressure.
Coronal prolongs the action of non-depolarizing muscle relaxants and the anticoagulant effect of coumarins.
When used simultaneously with Coronal, tricyclic and tetracyclic antidepressants, antipsychotic drugs (neuroleptics), ethanol, sedatives and hypnotics increase central nervous system depression and can provoke cardiac arrhythmias, bradycardia and orthostatic hypotension.
The simultaneous use of Coronal with MAO inhibitors is not recommended due to a significant increase in the hypotensive effect; the break in treatment between taking MAO inhibitors and Coronal should be at least 14 days.
When used simultaneously with Coronal, non-hydrogenated ergot alkaloids and ergotamine increase the risk of developing peripheral circulatory disorders.
When used simultaneously with Coronal, sulfasalazine increases the concentration of bisoprolol in plasma.
When used simultaneously with Coronal, rifampicin shortens the half-life of bisoprolol.
There is a potential risk of additive effects with the development of hypotension and/or significant bradycardia when used together with topical beta-blockers (eye drops).
There is a decrease in the antihypertensive effect of the drug with the use of adrenaline and norepinephrine.
The likelihood of disturbances in the automaticity, conduction and contractility of the heart increases (mutually) during therapy with quinidine drugs (mefloquine, chloroquine).
In case of shock or arterial hypotension caused by floctafenine, when used together, a decrease in compensatory cardiovascular reactions is possible.
When used simultaneously with baclofen or amifostine, an increase in antihypertensive effect is also observed.
Overdose
Overdose
Symptoms: arrhythmia, ventricular extrasystole, severe bradycardia, AV block, decreased blood pressure, acute heart failure, acrocyanosis, difficulty breathing, bronchospasm, dizziness, fainting, convulsions.
Treatment: it is necessary to rinse the stomach and prescribe adsorbent drugs. Symptomatic therapy is carried out: in case of developed AV block – intravenous administration of 1-2 mg of atropine, epinephrine or placement of a temporary pacemaker; for ventricular extrasystole – IV lidocaine (class I A drugs are not used); when blood pressure decreases, the patient should be in the Trendelenburg position; in the absence of symptoms of pulmonary edema – intravenous plasma-substituting solutions, if ineffective – administration of epinephrine, dopamine, dobutamine (to maintain chrono- and inotropic effects and eliminate a pronounced decrease in blood pressure); for heart failure – cardiac glycosides, diuretics, glucagon; for convulsions – intravenous diazepam; for bronchospasm – beta2-adrenergic stimulants by inhalation.
Storage conditions
Storage conditions
The drug should be stored out of the reach of children at a temperature not exceeding 25°C.
Shelf life
Shelf life
3 years.
Manufacturer
Manufacturer
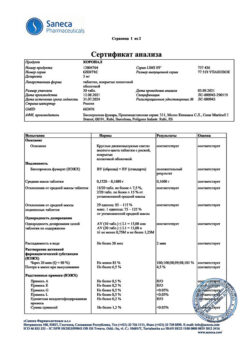
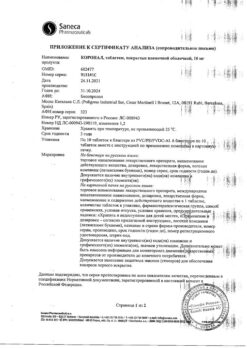
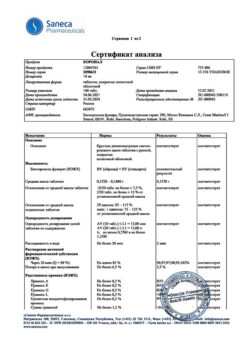
Saneka Pharmaceuticals a.s., Slovakia
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | The drug should be kept out of reach of children at a temperature not exceeding 25 ° C. |
| Manufacturer | Saneka Pharmaceuticals a.s., Slovakia |
| Medication form | pills |
| Brand | Saneka Pharmaceuticals a.s. |
Other forms…
Related products
Buy Coronal, 5 mg 100 pcs with delivery to USA, UK, Europe and over 120 other countries.