No products in the cart.
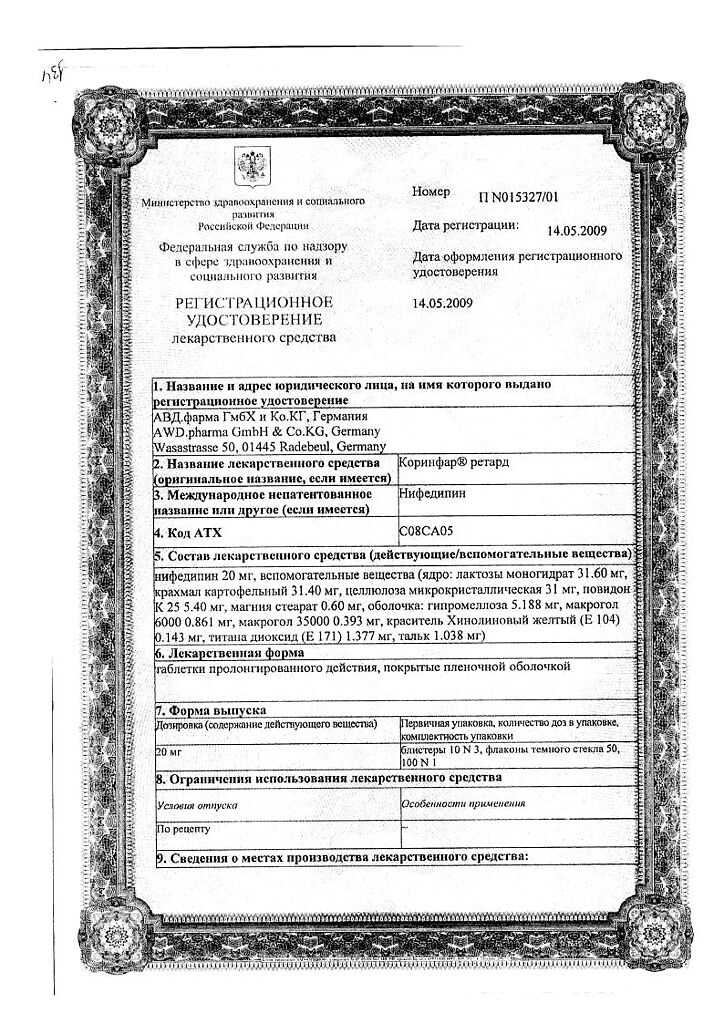
Corinfar retard, 20 mg 30 pcs
€4.55 €3.80
Description
Pharmacotherapeutic group: slow calcium channel blockers
ATX code: C08CA05
Pharmacological action
Pharmacodynamics
Nifedipine is a selective slow calcium channel blocker (BMCC), a 1,4-dihydropyridine derivative. It dilates coronary and peripheral arteries, reduces myocardial oxygen demand by reducing the post-load on the heart and oxygen delivery. Increases coronary blood flow, improves blood supply to ischemic areas without development of the “bypass” phenomenon, activates collaterals. By dilating peripheral arteries, it reduces total peripheral vascular resistance (TPR), myocardial tone, afterload, oxygen demand and increases duration of left ventricular (LV) diastolic relaxation. It has almost no effect on sinoatrial and atrioventricular nodes. Does not have antiarrhythmic and proarrhythmic effects. Does not affect the tone of the veins. Nifedipine increases renal blood flow, causes moderate natriuresis.
It has negative chrono-, dromo- and inotropic effects accompanied by reflex activation of the sympathoadrenal system and increased heart rate (HR) in response to peripheral vasodilation. Predominantly at the beginning of therapy, heart rate and cardiac output may decrease as a result of baroreceptor reflex activation. With prolonged therapy with nifedipine, heart rate and cardiac output return to the values they had before the start of therapy.
Nifedipine has antihypertensive and antianginal effects.
In arterial hypertension, the drug reduces blood pressure (BP) due to peripheral vasodilation and reduction of PPS. Nifedipine once daily provides 24-hour control of elevated BP. In patients with normal BP, nifedipine has little or no effect on BP.
In angina, nifedipine reduces peripheral and coronary vascular resistance, resulting in increased coronary blood flow, cardiac output and stroke volume, and decreased afterload. In addition, nifedipine dilates both intact and atherosclerotically altered coronary arteries, prevents coronary artery spasm, and improves perfusion of ischemic myocardium. Nifedipine reduces the frequency of angina attacks and ischemic ECG changes, regardless of whether they are caused by coronary artery spasm or atherosclerosis.
Pharmacokinetics
Absorption – high (more than 90%). Bioavailability is 50-70%. Simultaneous intake of food does not affect absorption. It has the effect of “first passage” through the liver.
Distribution. It penetrates through the blood-brain and placental barriers and is excreted with breast milk. Binding with blood plasma proteins (albumin) is 95%. Metabolism. It is completely metabolized in the liver. The metabolism of nifedipine is mainly carried out by the CYP3A4 isoenzyme, but also by the CYP1A2 and CYP2A6 isoenzymes. Evolution. There is no cumulative effect. Chronic renal failure, hemodialysis and peritoneal dialysis have no effect on pharmacokinetics. In patients with hepatic impairment, total clearance is decreased and T1/2 is increased. Long-term use (2-3 months) develops tolerance to the effects of the drug. Patient special groups Elderly patients . When nifedipine preparations are used in the form of sustained-release/modified-release tablets, increased Cmax and T1/2 have been noted in elderly patients (age > 60 years) compared to younger patients. Patients with impaired liver function Pharmacokinetic studies have shown that patients with cirrhosis have significantly increased T1/2 and decreased total clearance of nifedipine. In patients with mild (Child-Pugh class A) and moderate (Child-Pugh class B) hepatic impairment, clearance of nifedipine after oral administration was decreased by 48% and 72%, respectively, compared to patients with normal liver function, according to a clinical study. There was observed 93% and 64% increase of area under “concentration-time” curve (AUC) and Cmax, respectively, in patients with mild hepatic impairment (Child-Pugh class A) and 253% and 171% in patients with moderate hepatic impairment (Child-Pugh class B) compared with patients with normal hepatic function. The pharmacokinetics of nifedipine have not been studied in patients with severe hepatic impairment (Child-Pugh class C). Patients with impaired renal function The elimination of nifedipine may be delayed in patients with impaired renal function. Chronic renal failure, hemodialysis and peritoneal dialysis have no significant effect on the pharmacokinetics of nifedipine. There is no cumulative effect. Children and adolescents Pharmacokinetic studies have not been performed.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Overly after a meal, without chewing and with plenty of liquid.
The dose of the drug is adjusted by the physician individually according to the severity of the disease and the patient’s sensitivity to the drug. For patients with concomitant severe cerebrovascular disease and in elderly patients, the dose should be reduced.
Concomitant ingestion delays, but does not decrease, absorption of the active ingredient from the gastrointestinal tract.
The recommended dosing regimen for adults:
Stable angina and vasospastic angina (Prinzmetal angina, variant angina)
The drug is prescribed at 20 mg (1 tablet) 2 times daily. If the clinical effect is not sufficiently pronounced, the dose is gradually increased to 40 mg (2 tablets) 2 times a day. The maximum daily dose is 80 mg (4 tablets daily).
Arterial hypertension
The drug is prescribed 20 mg (1 tablet) 2 times a day. If the clinical effect is not sufficiently pronounced, the dose of the drug is gradually increased to 40 mg (2 tablets) 2 times a day. The maximum daily dose is 80 mg (4 tablets daily).
When prescribing the drug 2 times a day, the interval between doses should be on average 12 hours. The minimum interval between doses is at least 4 hours.
The duration of treatment is determined by the physician.
In cases where the drug is taken in high doses and/or for a long time, treatment should be stopped gradually to avoid withdrawal syndrome.
Some patients may require higher doses of nifedipine. Increasing the daily dose of nifedipine beyond 120 mg is not recommended.
When a daily dose of nifedipine in excess of 40 mg is required for the treatment of arterial hypertension or angina pectoris, administration of nifedipine preparations in the form of sustained release tablets in doses of 40 mg or 60 mg is recommended.
Patient special groups
Elderly patients
The pharmacokinetics of nifedipine are altered in elderly patients (over 65 years of age); therefore, the maintenance dose of the drug may be reduced compared with younger patients.
Patients with hepatic impairment
In patients with mild hepatic impairment, the dose of nifedipine should be reduced. The drug is contraindicated in patients with moderate to severe hepatic impairment (Child-Pugh grades B and C).
Patients with impaired renal function
In patients with impaired renal function no dose adjustment of nifedipine is required.
Interaction
Interaction
Pharmacokinetic interactions
Drugs affecting the metabolism of nifedipine
Nifedipine is metabolized by CYP3A4/5 isoenzymes, which are located in the intestinal mucosa and liver. Drugs that inhibit or induce this enzyme system may affect the effect
“primary passage” through the liver (after ingestion) or clearance of nifedipine.
Inductors of CYP3A4 isoenzyme Rifampicin
Rifampicin is a potent inducer of the CYP3A4 isoenzyme. Concomitant use with rifampicin significantly reduces the bioavailability of nifedipine and, accordingly, its effectiveness decreases. Therefore, concomitant use of nifedipine with rifampicin is contraindicated.
Antioepileptic drugs inducing CYP3A4 isoenzyme (e.g. phenytoin, carbamazepine, phenobarbital)
Phenytoin induces CYP3A4 isoenzyme. Concomitant use of nifedipine and phenytoin decreases the bioavailability of nifedipine and reduces its effectiveness. When concomitant use of this combination it is necessary to monitor the clinical response to nifedipine therapy and increase its dose, if necessary. If the dose of nifedipine is increased with concomitant use of both drugs, the dose of nifedipine should be reduced after phenytoin withdrawal.
Clinical studies on the potential interaction of nifedipine and carbamazepine or phenobarbital have not been conducted. Since both drugs decrease plasma concentrations of nimodipine, a structurally similar BMCC, the possibility of decreased plasma concentrations of nifedipine and decreased efficacy cannot be excluded.
Inhibitors of CYP3A4 isoenzyme
Antibiotics of macrolide group (e.g. erythromycin)
Special Instructions
Special Instructions
Cardiovascular disease
Arterial hypotension
Nifedipine dilates the peripheral arteries, reduces blood pressure and may in some cases cause severe arterial hypotension. It is necessary to use the drug with caution in patients who are prone to arterial hypotension, especially in patients with coronary heart disease or with cerebrovascular diseases in whom excessive reduction of BP may lead to myocardial infarction or stroke. In case of severe arterial hypotension, the dose should be reduced or nifedipine should be temporarily stopped.
The risk of arterial hypotension is higher in patients taking beta-adrenoblockers. Concomitant use of nifedipine and beta-adrenoblockers should be performed under close medical supervision, as it may cause excessive BP reduction and in some cases aggravation of chronic heart failure symptoms.
Severe arterial hypotension and/or high need for fluid replacement have been noted in patients treated with nifedipine and beta-adrenoblockers during aortocoronary bypass surgery under general anesthesia with high-dose fentanyl. If the patient requires surgery under general anesthesia during therapy, it is necessary to inform the anesthesiologist about the nature of the therapy. If surgery under general anesthesia with high doses of fentanyl is planned, it is recommended to discontinue Corinfar® retard at least 36 hours prior to surgery.
Arterial hypertension
There is no clinical experience with the use of nifedipine in malignant arterial hypertension.
The drug Corinfar® retard should not be used to lower blood pressure in a hypertensive crisis.
Chronic Coronary Heart Disease
The Corinfar® retard drug retard should not be used to relieve angina attacks and for secondary prevention of cardiovascular complications in patients who have had a myocardial infarction.
Unstable angina and/or myocardial infarction
.In rare cases, patients with coronary artery disease (especially those with severe obstructive coronary artery disease) have reported increased frequency, duration and/or severity of angina attacks and, in isolated cases, the development of myocardial infarction after initiation of BMCCs (including nifedipine) or after increasing their dosage. The mechanism of this phenomenon is not known.
Nifedipine in immediate-release tablet form is contraindicated in acute myocardial infarction.
There is no clinical experience with nifedipine in sustained release tablet form in acute myocardial infarction and unstable angina pectoris; therefore, their use is contraindicated in these diseases.
Chronic Heart Failure (CHF)
BMCs (including nifedipine) should be used with extreme caution in patients with CHF. In decompensated CHF the use of Corinfar® retard is not recommended.
Withdrawal syndrome of beta-adrenoblockers
.In patients with angina pectoris, discontinuation of beta-adrenoblockers may lead to development of withdrawal syndrome (increased frequency, duration and/or severity of angina attacks), possibly due to hypersensitivity to catecholamines. Administration of nifedipine does not prevent the development of “withdrawal” syndrome of beta-adrenoblockers, and may even lead to its enhancement due to reflex release of catecholamines in response to peripheral vasodilation.
Nifedipine has no antiarrhythmic effect and does not prevent the occurrence of cardiac rhythm disturbances during abrupt withdrawal of beta-adrenoblockers. If therapy with a beta-adrenoblocker needs to be discontinued, the dose should be gradually reduced until nifedipine is prescribed.
Aortic stenosis/ mitral stenosis/hypertrophic obstructive cardiomyopathy
As with all drugs with vasodilatory effects, nifedipine should be used with caution in patients with aortic stenosis, mitral stenosis or hypertrophic obstructive cardiomyopathy. In patients with hemodynamically significant left ventricular outflow tract obstruction (e.g., severe aortic stenosis) the drug is contraindicated.
In patients with obstructive cardiomyopathy there is a risk of increased frequency, severity and duration of angina attacks after nifedipine administration. In this case, withdrawal of the drug is necessary.
Peripheral edema
Slight to moderate peripheral edema associated with peripheral arterial dilatation has been reported with nifedipine. Swelling is usually localized in the lower extremities, sometimes reduced with the use of diuretics. In patients with concomitant chronic heart failure, peripheral edema associated with nifedipine use should be carefully differentiated from symptoms of progressive left ventricular dysfunction.
Diabetes
In patients with diabetes, plasma glucose concentration monitoring may be required when using nifedipine preparations.
Liver function impairment
In rare cases, when using nifedipine preparations, increased activity of some enzymes, such as: alkaline phosphatase, creatine phosphokinase, lactate dehydrogenase, aspartate aminotransferase (ACT) and alanine aminotransferase (AJIT) – which are usually transient but can sometimes be significantly pronounced. The causal relationship with nifedipine intake is uncertain in most cases, but in some cases it is very likely. These changes in laboratory parameters are rarely accompanied by clinical symptomatology. However, cases of cholestasis with or without jaundice have been described, as well as rare cases of autoimmune hepatitis.
Patients with impaired liver function are closely monitored, and if necessary, the drug dose is reduced and/or other dosage forms of nifedipine are used.
In patients with impaired renal function
The use of nifedipine in patients with impaired renal function is safe; no dose adjustment of nifedipine is required. In some cases, transient increase in serum urea nitrogen and creatinine concentrations has been observed in patients with chronic renal insufficiency. Causal relationship with nifedipine intake is uncertain in most cases, but in some cases it is very probable.
In patients with malignant hypertension on hemodialysis, hypovolemia (decreased circulating blood volume) after dialysis procedure may enhance antihypertensive effect of nifedipine and lead to a sharp decrease of BP. In such patients Corinfar® retard should be used with extreme caution, if necessary, the drug dose should be reduced.
Drug interactions
Nifedipine is metabolized by CYP3A4 isoenzyme. Drugs that inhibit or induce CYP3A4 may affect the effect
The “primary passage” through the liver or clearance of nifedipine.
Drugs that are mild to moderate inhibitors of the CYP3A4 isoenzyme that increase the plasma concentration of nifedipine include:
When nifedipine and the above drugs are used concomitantly, BP should be monitored and the dose of nifedipine should be adjusted if necessary. Surgical interventions/general anesthesia
Inhalational anesthetics may increase BP reduction. If a patient requires surgery under general anesthesia during therapy, it is necessary to inform the anesthesiologist that the patient is taking nifedipine.
Diagnostic tests
At the time of treatment, positive results are possible with direct Coombs reaction (with or without hemolytic anemia) and laboratory tests for antinuclear antibodies.
Nifedipine, like other DMARDs, inhibits platelet aggregation under in vitro conditions. A small number of clinical studies support data on statistically significant decrease in platelet aggregation and increase in bleeding time.
Presumably, the cause of these changes is blockade of calcium transport across the platelet membrane. The clinical significance of this effect is unknown.
Nifedipine can cause false increases in urinary concentrations of vanillylmindalic acid when determined by spectrophotometric method, but does not affect the results of measurements when using high performance liquid chromatography (HPLC).
Alcohol
Alcoholic beverages are not recommended during treatment because of the risk of excessive lowering of blood pressure.
The use in elderly patients
Cautious use of nifedipine in elderly patients must be observed because of the high likelihood of age-related renal dysfunction.
Cessation of therapy
Cessation of nifedipine should be done gradually (there is a risk of withdrawal).
Influence on ability to drive vehicles, machinery
In some patients, especially at the beginning of treatment, nifedipine may cause dizziness, which reduces the ability to drive vehicles or other mechanisms. Thereafter, the degree of restriction depends on the individual tolerability of nifedipine.
At the time of treatment, especially at the beginning of treatment or when changing the dose, caution should be exercised when driving vehicles and engaging in potentially hazardous activities that require increased concentration and rapid psychomotor reactions.
Synopsis
Synopsis
Contraindications
Contraindications
With caution
Arterial hypotension, malignant arterial hypertension (no experience in clinical use), coronary heart disease (especially with severe obstructive coronary artery disease) or cerebrovascular disease, chronic heart failure; concomitant use with beta-adrenoblockers and other hypotensive drugs; concomitant use with cardiac glycosides; aortic stenosis, mitral stenosis, hypertrophic obstructive cardiomyopathy; diabetes mellitus; mild hepatic impairment (class A according to Child-Pugh classification); hemodialysis in patients with malignant hypertension (risk of severe arterial hypotension); concomitant use with CYP3A4 isoenzyme inhibitors and/or inducers (e.g., phenytoin, carbamazepine, phenobarbital, macrolide antibiotics, HIV protease inhibitors, ketoconazole, antidepressants, fluoxetine, valproic acid, etc.
Pregnancy of more than 20 weeks (the drug may be used as “backup therapy”); older age.
Side effects
Side effects
Unwanted reactions are systematized relative to each of the organ systems according to frequency of occurrence using the World Health Organization (WHO) classification as follows: Very common (â¥1/10); common (â¥1/100, < 1/10); infrequent (â¥1/1000, < 1/100); rare (â¥1/10000, < 1/1000); very rare (< 1/10000); frequency unknown (cannot be determined from available data).
Blood and lymphatic system disorders: rare – thrombocytopenia, thrombocytopenic purpura; very rare – anemia; frequency unknown – leukopenia, agranulocytosis.
Disorders of the immune system: infrequent – allergic reactions, edema due to the development of an allergic reaction/angioedema (Quincke’s edema) (including laryngeal edema*); rare – skin itching, skin rash, urticaria; very rare – autoimmune hepatitis, photodermatitis; frequency unknown – anaphylactic/anaphylactoid reactions.
Disorders of metabolism and nutrition: very rare – hyperglycemia, weight gain.
Mental disorders: infrequent – anxiety, sleep disorders.
Nervous system disorders: frequently – headache, weakness; infrequently – migraine, dizziness; rarely – paresthesia, dysesthesia; frequency unknown – hypoesthesia, increased fatigue, drowsiness. When taking the drug in high doses for a long time – paresthesia of extremities, anxiety, extrapyramidal (parkinsonian) disorders (ataxia, mask-like face, shuffling gait, tremor of hands and fingers, difficulty in swallowing), depression.
Visual disorders: infrequent – visual impairment (including transient loss of vision at maximum plasma concentration of nifedipine); frequency unknown – eye pain.
Chronic disorders: infrequent – tachycardia, palpitations; rare – in some patients, especially at the beginning of treatment or when increasing the dose, angina attacks may occur, and in single cases – development of myocardial infarction, which requires stopping the drug; frequency is unknown – arrhythmia, chest pain.
vascular disorders: often – peripheral edema, manifestations of excessive vasodilation (asymptomatic BP decrease, development or aggravation of the course of heart failure (often aggravation of already existing), “rushes” of blood to the face, facial skin hyperemia, feeling of heat); infrequent – pronounced BP decrease, fainting.
Relatory system, chest and mediastinum disorders: infrequent – nasal bleeding, stuffy nose; rare – difficulty in breathing, cough; very rare – bronchospasm; frequency unknown – shortness of breath, pulmonary edema**.
Gastrointestinal tract disorders: Frequent – constipation; infrequent – astrointestinal and abdominal pain, dyspepsia (nausea, diarrhea or constipation), dry mouth mucosa, flatulence; rare – gum hyperplasia (bleeding, painfulness, swelling); frequency unknown – vomiting, gastroesophageal sphincter failure, increased appetite.
Hepatic and biliary tract disorders: infrequent – increased activity of “hepatic” transaminases; rarely – in long-term use – hepatic dysfunction (intrahepatic cholestasis).
Dermatological and subcutaneous tissue disorders: infrequent erythema; rare – exfoliative dermatitis, photodermatitis; frequency unknown – toxic epidermal necrolysis (Lyell’s syndrome), purpura.
Muscular and connective tissue disorders: infrequent – muscle cramps, joint swelling; rare – arthralgia, myalgia; frequency unknown – arthritis.
Kidney and urinary tract disorders: infrequent – polyuria, dysuria; frequency unknown – worsening of renal function (in patients with renal failure).
Gender and mammary gland disorders: infrequent – erectile dysfunction; very rare – gynecomastia (in elderly patients, disappearing completely after discontinuation of the drug), galactorrhea.
General disorders and disorders at the site of administration: often – asthenia, weakness; infrequently – nonspecific pain, chills.
* may lead to a life-threatening condition
** cases have been reported when used as a tocolytic agent during pregnancy (see Use in pregnancy and during breastfeeding)
In patients on hemodialysis, with malignant arterial hypertension, or with reduced circulating blood volume, a marked decrease in BP may occur as a result of vasodilation.
Overdose
Overdose
Symptoms
Nifedipine causes peripheral vasodilation with severe and possibly prolonged systemic arterial hypotension: headache, facial hyperemia, prolonged marked BP decrease, sinus node suppression, bradycardia and/or tachycardia, bradyarrhythmia. In severe poisoning – loss of consciousness, coma.
Treatment
The treatment of overdose consists of standard procedures for eliminating the drug from the body. Administration of activated charcoal, gastric lavage (if necessary – small bowel lavage), restoration of stable hemodynamic parameters is indicated.
In case of overdose with prolonged nifedipine it is necessary to ensure the most complete elimination of the drug from the body, if possible – small intestine lavage in order to prevent further absorption of the active substance. When using laxatives it should be taken into account that PBMC may cause decrease of intestinal muscle tone up to intestinal atony.
The antidote for nifedipine is calcium preparations. Intravenous injection of 10-20 ml of 10% solution of calcium chloride or calcium gluconate is indicated, followed by switching to prolonged infusion. If the administration of calcium preparations failed to achieve a sufficient rise in BP, alpha-adrenomimetics (dopamine, norepinephrine) may be used.
In bradyarrhythmia – IV administration of atropine, beta-adrenomimetics. In life-threatening bradyarrhythmias, placement of a temporary pacemaker is recommended. In the development of heart failure – intravenous infusion of strophantine. Infusion therapy is recommended with caution due to the risk of volume overload of the heart.
Careful monitoring of the heart, lungs and excretory system is necessary. It is recommended to monitor glucose concentrations (insulin release may decrease) and electrolytes (potassium, calcium) in the blood.
Hemodialysis is ineffective due to the high degree of binding to plasma proteins and relatively small volume of distribution. Plasmapheresis is possible.
Pregnancy use
Pregnancy use
Pregnancy
The use of nifedipine in pregnancy below 20 weeks is contraindicated. The use of nifedipine at more than 20 weeks’ gestation is possible as a “backup therapy” for severe arterial hypertension in cases where the expected benefit to the mother exceeds the possible risk to the fetus.
There have been no adequately controlled studies involving pregnant women. The available information is insufficient to rule out the possibility of side effects that pose a risk to the fetus and the newborn.
In animal studies, nifedipine has been shown to be embryotoxic, fetotoxic, and teratogenic. No specific prenatal risk has been identified based on clinical data. However, there has been an increased incidence of perinatal asphyxia, cesarean section, as well as preterm birth and intrauterine fetal delay. The relationship of these reports to existing arterial hypertension, its treatment, or the specific effect of the drug is unclear.
In the use of PBMCs, including nifedipine, as a tocolytic agent during pregnancy, especially multiple pregnancies (twins or more), cases of acute pulmonary edema have been observed with intravenous administration of the drug and/or with concurrent use of beta2-adrenomimetics.
Nifedipine should not be used during pregnancy unless the woman’s clinical condition requires treatment with nifedipine. Nifedipine may be considered as a “backup therapy” for women with severe arterial hypertension who do not respond to standard therapy.
Period of breastfeeding
Nifedipine is excreted in breast milk. The concentration of nifedipine in breast milk is comparable to its concentration in the blood serum of the mother. The effect of the drug excreted with breast milk on the child is unknown. Therefore, if it is necessary to use nifedipine during lactation, it is recommended to stop breastfeeding.
Fertility
In single cases in in vitro fertilization, the use of BMCCs, including nifedipine, has been associated with reversible biochemical changes in the sperm head, which could lead to impaired sperm function. If in vitro fertilization attempts are unsuccessful and other causes of infertility are excluded, the possibility of effects of BMCCs, including nifedipine, on sperm function should be considered.
Similarities
Similarities
Additional information
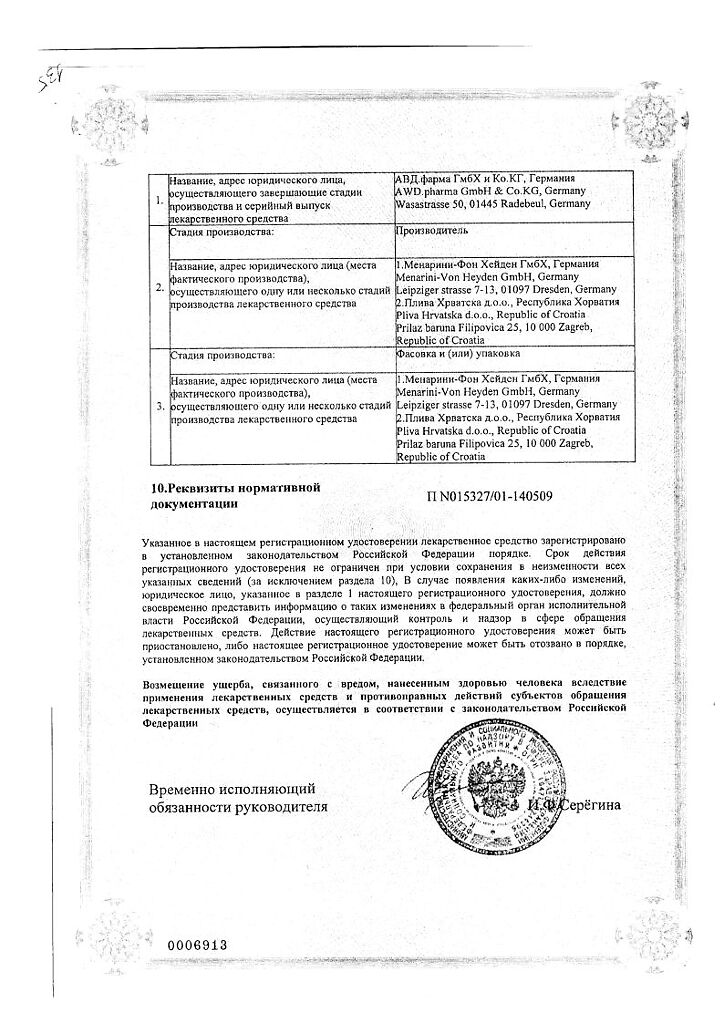
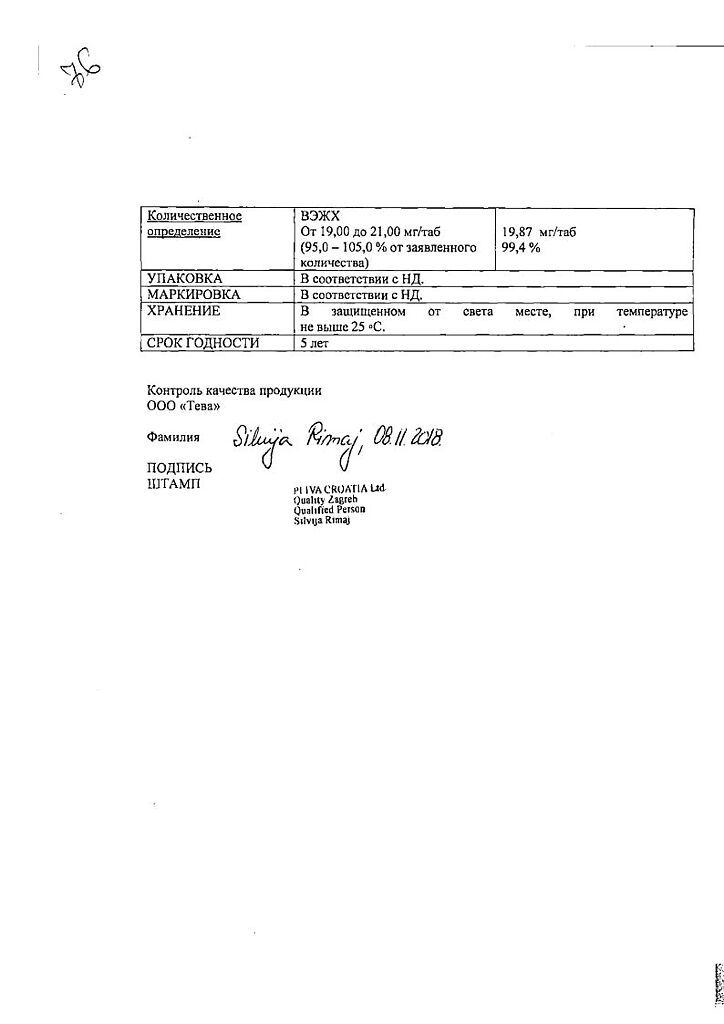
| Shelf life | 5 years |
|---|---|
| Conditions of storage | Store at a temperature not higher than 25 ° C in the original package. KEEP OUT OF REACH OF CHILDREN. |
| Manufacturer | Pliva Hrvatska d.o.o., Croatia |
| Medication form | sustained release tablets |
| Brand | Pliva Hrvatska d.o.o. |
Other forms…
Related products
Buy Corinfar retard, 20 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.