No products in the cart.
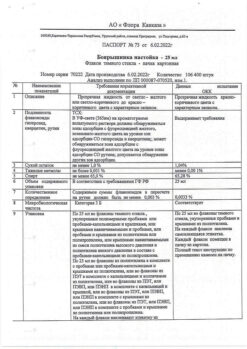
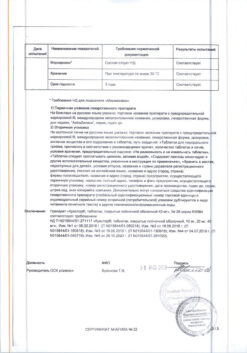
Corinfar, 10 mg 50 pcs
€2.84 €2.58
Description
Pharmacotherapeutic group: slow calcium channel blocker (BMCC).
Code ATX: C08CA05
Pharmacological properties
Pharmacodynamics.
Nifedipine is a selective slow calcium channel blocker (CMCB), a 1,4-dihydropyridine derivative. It dilates coronary and peripheral arteries, reduces myocardial oxygen demand by reducing the post-load on the heart and oxygen delivery. Increases coronary blood flow, improves blood supply to ischemic zones without development of the “bypass” phenomenon, activates collaterals. By dilating peripheral arteries, it reduces total peripheral vascular resistance (TPR), myocardial tone, afterload, myocardial oxygen demand and increases duration of left ventricular (LV) diastolic relaxation. It has almost no effect on the sinoatrial and atrioventricular nodes. Does not have antiarrhythmic and proarrhythmogenic effects. Does not affect the tone of the veins. Nifedipine increases renal blood flow, causing moderate natriuresis.
It has negative chrono-, dromo- and inotropic effects accompanied by reflex activation of the sympathoadrenal system and increased heart rate (HR) in response to peripheral vasodilation. Predominantly at the beginning of therapy, heart rate and cardiac output may decrease as a result of baroreceptor reflex activation. With prolonged therapy with nifedipine, heart rate and cardiac output return to the values they had before the start of therapy.
Nifedipine has antihypertensive and antianginal effects.
In arterial hypertension, the drug reduces blood pressure (BP) due to peripheral vasodilation and reduction of PPS. Nifedipine once daily provides 24-hour control of elevated BP. In patients with normal BP, nifedipine has little or no effect on BP.
In angina, nifedipine reduces peripheral and coronary vascular resistance, which leads to increased coronary blood flow, cardiac output and stroke volume, and decreased afterload. In addition, nifedipine dilates both intact and atherosclerotically altered coronary arteries, prevents coronary artery spasm, and improves perfusion of ischemic myocardium. Nifedipine reduces the frequency of angina attacks and ischemic ECG changes, whether caused by coronary artery spasm or atherosclerosis.
Pharmacokinetics
Absorption is high (over 90%). Bioavailability is 50-70%. Simultaneous intake of food does not affect absorption. It has the effect of “first passage” through the liver.
Distribution. Maximum concentration of nifedipine (Cmax) in plasma after a single oral administration of 2 tablets (corresponding to 20 mg nifedipine) is reached after 1-3 hours and its value averages 28.3 ng/ml.
It penetrates through the blood-brain and placental barriers, is excreted with breast milk. Binding with blood plasma proteins (albumin) is 95%.
In patients with impaired hepatic or renal function a significant decrease of nifedipine binding to plasma proteins is possible.
Metabolism. It is completely metabolized in the liver.
The metabolism of nifedipine is mainly carried out by the CYP3A4 isoenzyme, but also by the CYP1A2 and CYP2A6 isoenzymes.
Elimation. It is excreted by the kidneys as an inactive metabolite (60-80% of the dose taken). 20% with bile. The elimination half-life (T1/2) is 2-5 hours.
There is no cumulative effect. Chronic renal failure, hemodialysis and peritoneal dialysis do not affect pharmacokinetics.
In patients with hepatic impairment, total clearance is decreased and T1/2 is increased.
Special patient groups
Patients of advanced age
. When using nifedipine preparations in the form of prolonged/modified-release tablets, elderly patients (age > 60 years) showed increased Cmax and T1/2 compared to younger patients.
Patients with impaired liver function
Pharmacokinetic studies have shown that patients with cirrhosis have significant increases in T1/2 and decreased total clearance of nifedipine. In patients with mild (Child-Pugh class A) and moderate (Child-Pugh class B) hepatic impairment, nifedipine clearance after oral administration was reduced by 48% and 72%, respectively, compared to patients with normal hepatic function, according to a clinical study. There was an increase in the area under the concentration-time curve (AUC) and Cmah by 93% and 64% in patients with mild hepatic impairment (Child-Pugh class A) and by 253% and 171% in patients with moderate hepatic impairment (Child-Pugh class B), respectively, compared to patients with normal hepatic function. The pharmacokinetics of nifedipine have not been studied in patients with severe hepatic impairment (Child-Pugh class C).
Patients with impaired renal function
The elimination of nifedipine may be delayed in patients with impaired renal function. Chronic renal failure, hemodialysis and peritoneal dialysis have no significant effect on the pharmacokinetics of nifedipine. There is no cumulative effect.
Children and adolescents
Pharmacokinetic studies have not been performed.
Indications
Indications
Arterial hypertension.
Stable angina and vasospastic angina (Prinzmetal’s angina, variant angina).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: blocker of “slow” calcium channels (SCBC).
ATX code: C08CA05
Pharmacological properties
Pharmacodynamics
Nifedipine is a selective blocker of “slow” calcium channels (SCCC), a derivative of 1,4-dihydropyridine. Dilates coronary and peripheral arteries, reduces myocardial oxygen demand by reducing afterload on the heart and oxygen delivery. Strengthens coronary blood flow, improves blood supply to ischemic areas without developing the “steal” phenomenon, and activates the functioning of collaterals. By dilating peripheral arteries, it reduces total peripheral vascular resistance (TPVR), myocardial tone, afterload, myocardial oxygen demand and increases the duration of diastolic relaxation of the left ventricle (LV). It has virtually no effect on the sinoatrial and atrioventricular nodes. Does not have antiarrhythmic or proarrhythmic effects. Does not affect the tone of the veins. Nifedipine increases renal blood flow, causing moderate natriuresis.
It has a negative chrono-, dromo- and inotropic effect, which is accompanied by reflex activation of the sympathoadrenal system and an increase in heart rate (HR) in response to peripheral vasodilation. Mainly at the beginning of therapy, heart rate and cardiac output may decrease as a result of activation of the baroreceptor reflex. With long-term therapy with nifedipine, heart rate and cardiac output return to the values they had before the start of therapy.
Nifedipine has antihypertensive and antianginal effects.
For arterial hypertension, the drug reduces blood pressure (BP) due to peripheral vasodilation and a decrease in peripheral vascular resistance. Nifedipine, when taken once daily, provides 24-hour control of high blood pressure. In patients with normal blood pressure, nifedipine has no or only a slight effect on it.
In angina pectoris, nifedipine reduces peripheral and coronary vascular resistance, which leads to an increase in coronary blood flow, cardiac output and stroke volume, as well as a decrease in afterload. In addition, nifedipine dilates both intact and atherosclerotic coronary arteries, prevents spasm of the coronary arteries and improves perfusion of ischemic myocardium. Nifedipine reduces the frequency of angina attacks and ischemic ECG changes, regardless of whether they are caused by spasm or atherosclerosis of the coronary arteries.
Pharmacokinetics
Absorption is high (more than 90%). Bioavailability – 50-70%. Concomitant food intake does not affect absorption. Has a “first pass” effect through the liver.
Distribution. The maximum concentration of nifedipine (Cmax) in the blood plasma after a single oral dose of 2 tablets (corresponding to 20 mg of nifedipine) is reached after 1-3 hours and its value averages 28.3 ng/ml.
Penetrates through the blood-brain and placental barriers and is excreted in breast milk. Communication with blood plasma proteins (albumin) – 95%.
In patients with impaired liver or kidney function, a significant decrease in the binding of nifedipine to plasma proteins is possible.
Metabolism. Completely metabolized in the liver.
Nifedipine is metabolized primarily by the CYP3A4 isoenzyme, as well as the CYP1A2 and CYP2A6 isoenzymes.
Excretion. It is excreted by the kidneys in the form of an inactive metabolite (60-80% of the dose taken). 20% with bile. The half-life (T1/2) is 2-5 hours.
There is no cumulative effect. Chronic renal failure, hemodialysis and peritoneal dialysis do not affect pharmacokinetics.
In patients with liver failure, total clearance decreases and T1/2 increases.
Special patient groups
Elderly patients
When using nifedipine preparations in the form of extended/modified release tablets in elderly patients (age > 60 years), an increase in Cmax and T1/2 was observed compared to younger patients.
Patients with liver dysfunction
Pharmacokinetic studies have shown that patients with liver cirrhosis experience a significant increase in T1/2 and a decrease in the total clearance of nifedipine. According to a clinical study in patients with mild (Child-Pugh class A) and moderate (Child-Pugh class B) hepatic impairment, nifedipine clearance after oral administration was reduced by 48% and 72%, respectively, compared with patients with normal liver function. There was an increase in the area under the concentration-time curve (AUC) and Cmax by 93% and 64%, respectively, in patients with mild hepatic impairment (Child-Pugh class A) and by 253% and 171%, respectively, in patients with moderate hepatic impairment (Child-Pugh class B) compared with patients with normal liver function. The pharmacokinetics of nifedipine have not been studied in patients with severe hepatic impairment (Child-Pugh class C).
Patients with impaired renal function
Elimination of nifedipine may be delayed in patients with impaired renal function. Chronic renal failure, hemodialysis and peritoneal dialysis do not have a significant effect on the pharmacokinetics of nifedipine. There is no cumulative effect.
Children and teenagers
Pharmacokinetic studies have not been conducted.
Special instructions
Special instructions
Cardiovascular diseases
Arterial hypotension
Nifedipine dilates peripheral arteries, reduces blood pressure and can in some cases cause severe arterial hypotension. The drug should be used with caution in patients prone to arterial hypotension, especially in patients with coronary heart disease or cerebrovascular diseases, in whom an excessive decrease in blood pressure can lead to the development of myocardial infarction or stroke. In case of severe arterial hypotension, reduce the dose or temporarily stop taking nifedipine.
The risk of developing arterial hypotension is higher in patients taking beta-blockers. The simultaneous use of nifedipine and beta-blockers must be carried out under conditions of careful medical supervision, as this may cause an excessive decrease in blood pressure, and in some cases, aggravation of symptoms of chronic heart failure.
Severe hypotension and/or high fluid requirements have been reported in patients receiving nifedipine and beta-blocker therapy during coronary artery bypass graft surgery under general anesthesia with high doses of fentanyl. If during therapy the patient requires surgical intervention under general anesthesia, then it is necessary to inform the anesthesiologist about the nature of the therapy being performed. If surgery is planned under general anesthesia using high doses of fentanyl, it is recommended to stop taking Corinfar® at least 36 hours before surgery.
Arterial hypertension
There is no experience in the clinical use of nifedipine drugs for malignant arterial hypertension.
The drug Corinfar® should not be used to lower blood pressure during a hypertensive crisis.
Chronic ischemic heart disease
The drug Corinfar® should not be used for the relief of angina attacks and for the secondary prevention of cardiovascular complications in patients who have suffered a myocardial infarction.
Unstable angina and/or myocardial infarction
In rare cases, in patients with coronary heart disease (especially with severe obstructive lesions of the coronary arteries), an increase in the frequency, duration and/or severity of angina attacks was observed, as well as, in isolated cases, the development of myocardial infarction after starting the use of BMCC (including nifedipine) or after increasing their dosage. The mechanism of development of this phenomenon has not been studied.
Nifedipine immediate-release tablets are contraindicated in acute myocardial infarction.
There is no experience in the clinical use of nifedipine preparations in the form of extended-release tablets for acute myocardial infarction and unstable angina, and therefore their use in these diseases is contraindicated.
Chronic heart failure (CHF)
BMCC (including nifedipine) should be used with extreme caution in patients with CHF. In case of decompensated CHF, the use of Corinfar® is not recommended.
Beta-blocker withdrawal syndrome
In patients with angina, stopping beta-blockers may lead to a withdrawal syndrome (increased frequency, duration and/or severity of angina attacks), possibly due to increased sensitivity to catecholamines. Prescribing nifedipine does not prevent the development of beta-blocker withdrawal syndrome, and may even lead to its intensification due to the reflex release of catecholamines in response to peripheral vasodilation.
Nifedipine does not have an antiarrhythmic effect and does not prevent the occurrence of cardiac arrhythmias when beta-blockers are abruptly discontinued. If it is necessary to discontinue beta-blocker therapy, the dose should be gradually reduced before nifedipine is prescribed.
Aortic stenosis/ mitral stenosis/ hypertrophic obstructive cardiomyopathy
As with all drugs that have a vasodilating effect, nifedipine should be used with caution in patients with aortic stenosis, mitral stenosis or hypertrophic obstructive cardiomyopathy. In patients with hemodynamically significant obstruction of the left ventricular outflow tract (for example, with severe aortic stenosis), the use of the drug is contraindicated.
Patients with obstructive cardiomyopathy are at risk of increased frequency, severity, and duration of angina attacks after taking nifedipine. In this case, discontinuation of the drug is necessary.
Peripheral edema
When using nifedipine drugs, mild or moderate peripheral edema associated with dilatation of peripheral arteries was observed. Edema is usually localized in the lower extremities and sometimes decreases with the use of diuretics. In patients with concomitant chronic heart failure, peripheral edema associated with the use of nifedipine should be carefully differentiated from symptoms of progression of left ventricular dysfunction.
Diabetes mellitus
In patients with diabetes mellitus, when using nifedipine preparations, it may be necessary to monitor the concentration of glucose in the blood plasma.
Liver dysfunction
In rare cases, when using nifedipine preparations, an increase in the activity of certain enzymes, such as alkaline phosphatase, creatine phosphokinase, lactate dehydrogenase, aspartate aminotransferase (ACT) and alanine aminotransferase (AJIT), was observed, which is usually transient, but can sometimes be significant. A cause-and-effect relationship with nifedipine is uncertain in most cases, but is highly likely in some cases. These changes in laboratory parameters are rarely accompanied by clinical symptoms. However, cases of cholestasis with or without jaundice, as well as rare cases of autoimmune hepatitis, have been described.
Patients with impaired liver function are closely monitored and, if necessary, the dose of the drug is reduced and/or other dosage forms of nifedipine are used.
Renal dysfunction
The use of nifedipine drugs in patients with impaired renal function is safe; No dose adjustment of nifedipine is required. In some cases, patients with chronic renal failure experienced a transient increase in serum urea nitrogen and creatinine concentrations. A cause-and-effect relationship with nifedipine is uncertain in most cases, but is highly likely in some cases.
In patients with malignant hypertension undergoing hemodialysis, hypovolemia (decrease in circulating blood volume) after the dialysis procedure may enhance the antihypertensive effect of nifedipine and lead to a sharp decrease in blood pressure. In such patients, Corinfar® should be used with extreme caution; if necessary, the dose of the drug should be reduced.
Drug interactions
Nifedipine is metabolized by the CYP3A4 isoenzyme. Medicines that inhibit or induce CYP3A4 may affect the hepatic first-pass effect or clearance of nifedipine.
Medicines that are weak or moderate inhibitors of the CYP3A4 isoenzyme that increase the concentration of nifedipine in the blood plasma include:
macrolides (for example, erythromycin);
HIV protease inhibitors (eg, ritonavir);
azole antifungals (for example, ketoconazole);
antidepressants (nefazodone and fluoxetine),
quinupristin/dalfopristin;
valproic acid;
cimetidine
When using nifedipine and these drugs simultaneously, it is necessary to monitor blood pressure and, if necessary, adjust the dose of nifedipine. Surgery/general anesthesia
Inhalational anesthetics may enhance the reduction in blood pressure. If during therapy the patient requires surgery under general anesthesia, the anesthesiologist must be informed that the patient is taking nifedipine.
Diagnostic tests
During treatment, positive results are possible with direct Coombs test (with or without hemolytic anemia) and laboratory tests for antinuclear antibodies.
Nifedipine, like other BMCCs, inhibits platelet aggregation in vitro. A small number of clinical studies support data on a statistically significant decrease in platelet aggregation and an increase in bleeding time.
Presumably, the cause of such changes is the blockade of calcium transport across the platelet membrane. The clinical significance of this effect is unknown.
Nifedipine may cause a false increase in the concentration of vanillylmandelic acid in urine when determined by the spectrophotometric method, but does not affect the measurement results when using the high-performance liquid chromatography (HPLC) method.
Alcohol
During the treatment period, it is not recommended to drink alcoholic beverages due to the risk of an excessive decrease in blood pressure.
Use in elderly patients
Caution should be exercised when using nifedipine drugs in elderly patients due to the high likelihood of age-related renal dysfunction.
Discontinuation of therapy
The use of nifedipine should be discontinued gradually (there is a risk of developing withdrawal syndrome).
Impact on the ability to drive vehicles and machinery
In some patients, especially at the beginning of treatment, nifedipine may cause dizziness, which reduces the ability to drive vehicles or use other machinery. In the future, the degree of restrictions depends on the individual tolerance of nifedipine.
During the treatment period, especially at the beginning of treatment or when changing the dose, care must be taken when driving, engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Nifedipine
Composition
Composition
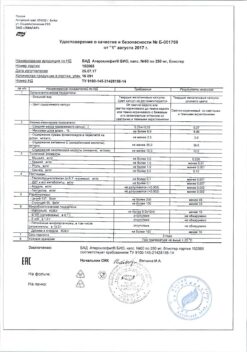
1 tablet contains: active ingredient: nifedipine 10.00 mg; excipients (tablet core): lactose monohydrate 15.80 mg, potato starch 15.70 mg, microcrystalline cellulose 15.50 mg, povidone K25 2.70 mg, magnesium stearate 0.30 mg; excipients (tablet shell): hypromellose 2.88 mg, macrogol 6000 0.48 mg, macrogol 35000 0.22 mg, quinoline yellow dye (E104) 0.27 mg, titanium dioxide 0.77 mg, talc 0.38 mg.
Pregnancy
Pregnancy
Pregnancy
The use of nifedipine during pregnancy up to 20 weeks is contraindicated. The use of nifedipine during pregnancy over 20 weeks is possible as a means of “reserve therapy” for severe arterial hypertension, in cases where the expected benefit to the mother outweighs the possible risk to the fetus.
There are no adequate controlled studies in pregnant women. The available information is insufficient to exclude the possibility of side effects that pose a danger to the fetus and newborn.
In animal studies, nifedipine has been shown to be embryotoxic, fetotoxic and teratogenic. Based on clinical data, no specific prenatal risk was identified. However, an increase in the incidence of perinatal asphyxia, cesarean section, as well as preterm birth and intrauterine growth restriction was noted. The relationship of these reports to existing hypertension, its treatment, or the specific effect of the drug is unclear.
When using BMCC, including nifedipine, as a tocolytic agent during pregnancy, especially multiple pregnancies (twins or more), with intravenous administration of the drug and/or with the simultaneous use of beta2-adrenergic agonists, cases of acute pulmonary edema were observed.
Nifedipine should not be used during pregnancy, unless the woman’s clinical condition requires treatment with nifedipine. Nifedipine may be considered as a “back-up therapy” for women with severe hypertension who do not respond to standard therapy.
Breastfeeding period
Nifedipine is excreted into breast milk. The concentration of nifedipine in breast milk is comparable to its concentration in maternal serum. The effect of the drug, which is excreted in breast milk, on the child’s body is unknown. Therefore, if it is necessary to use nifedipine during lactation, it is recommended to stop breastfeeding.
Fertility
In isolated cases during in vitro fertilization, the use of BMCC, including nifedipine, was associated with reversible biochemical changes in the head of the sperm, which could lead to impaired sperm function. In case of unsuccessful attempts at in vitro fertilization and when other causes of infertility are excluded, the possibility of the influence of BMCC, including nifedipine, on the condition of sperm should be considered
Contraindications
Contraindications
Hypersensitivity to nifedipine, other dihydropyridine derivatives or any other component of the drug.
Moderate and severe liver failure (classes B and C according to the Child-Pugh classification).
Cardiogenic shock.
Collapse.
Severe arterial hypotension (systolic blood pressure below 90 mm Hg).
Acute period of myocardial infarction (during the first 4 weeks).
Unstable angina.
Hemodynamically significant obstruction of the left ventricular outflow tract (including severe aortic stenosis).
Concomitant use with rifampicin (due to the inability to achieve effective levels of nifedipine in the blood plasma due to enzyme induction).
Pregnancy (up to 20 weeks).
Breastfeeding period.
Age up to 18 years (efficacy and safety have not been established).
Rare hereditary galactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome (the drug contains lactose).
With caution
Arterial hypotension, malignant arterial hypertension (no experience of clinical use), coronary heart disease (especially with severe obstructive lesions of the coronary arteries) or cerebrovascular diseases, chronic heart failure; simultaneous use with beta-blockers and other antihypertensive drugs; simultaneous use with cardiac glycosides; aortic stenosis, mitral stenosis, hypertrophic obstructive cardiomyopathy; diabetes mellitus; mild liver dysfunction (class A according to the Child-Pugh classification); hemodialysis in patients with malignant hypertension (risk of developing severe arterial hypotension); simultaneous use with inhibitors and/or inducers of the CYP3A4 isoenzyme (for example, phenytoin, carbamazepine, phenobarbital, macrolide antibiotics, HIV protease inhibitors, ketoconazole, antidepressants, fluoxetine, valproic acid, etc.); pregnancy for more than 20 weeks (the drug can be used as a means of “backup therapy”); old age.
Side Effects
Side Effects
Adverse reactions are systematized for each organ system depending on the frequency of occurrence using the World Health Organization (WHO) classification as follows: very often (≥1/10); often (≥1/100, <1/10); uncommon (≥1/1000, <1/100); rare (≥1/10000, <1/1000); very rare (< 1/10000); frequency unknown (cannot be determined from available data).
Disorders of the blood and lymphatic system: rarely – thrombocytopenia, thrombocytopenic purpura; very rarely – anemia; frequency unknown – leukopenia, agranulocytosis.
Immune system disorders: uncommon – allergic reactions, edema due to the development of an allergic reaction/angioedema (Quincke’s edema) (including laryngeal edema*); rarely – itching, skin rash, urticaria; very rarely – autoimmune hepatitis; frequency unknown – anaphylactic/anaphylactoid reactions.
Metabolic and nutritional disorders: very rarely – hyperglycemia, weight gain.
Mental disorders: infrequently – anxiety, sleep disorders.
Nervous system disorders: often – headache, weakness; infrequently – migraine, dizziness; rarely – paresthesia, dysesthesia; frequency unknown – hypoesthesia, drowsiness, increased fatigue. With long-term use in high doses – paresthesia of the limbs, depression, anxiety, extrapyramidal (parkinsonian) disorders (ataxia, “mask-like” face, shuffling gait, stiffness in the movements of the arms and legs, tremor of the hands and fingers, difficulty swallowing).
Violations of the organ of vision: infrequently – visual impairment (including transient loss of vision against the background of the maximum concentration of nifedipine in the blood plasma); frequency unknown – pain in the eyes.
Cardiac disorders: uncommon – tachycardia, palpitations; rarely – in some patients, especially at the beginning of treatment, angina attacks may occur, which requires discontinuation of the drug; Isolated cases of myocardial infarction have been described; frequency unknown – arrhythmia, chest pain.
Vascular disorders: often – including peripheral edema, manifestations of excessive vasodilation (asymptomatic decrease in blood pressure, development or aggravation of heart failure (usually aggravation of an existing one), “flushes” of blood to the facial skin, flushing of the facial skin, feeling of heat); infrequently – pronounced decrease in blood pressure, fainting.
Disorders of the respiratory system, chest and mediastinal organs: infrequently – nosebleeds, nasal congestion; rarely – difficulty breathing, cough; very rarely – bronchospasm; frequency unknown – shortness of breath, pulmonary edema**.
Gastrointestinal disorders: often – constipation; uncommon – gastrointestinal and abdominal pain, dyspepsia (nausea, diarrhea or constipation), flatulence, dry oral mucosa; rarely – gum hyperplasia (bleeding, pain, swelling); frequency unknown – vomiting, gastroesophageal sphincter insufficiency, increased appetite.
Disorders of the liver and biliary tract: infrequently – increased activity of “liver” transaminases; rarely – with long-term use, liver dysfunction (intrahepatic cholestasis).
Disorders of the skin and subcutaneous tissues: infrequently – erythema; rarely – exfoliative dermatitis, photodermatitis; frequency unknown – toxic epidermal necrolysis (Lyell’s syndrome), purpura.
Musculoskeletal and connective tissue disorders: uncommon – muscle cramps, joint swelling; rarely – arthralgia, myalgia, frequency unknown – arthritis.
Renal and urinary tract disorders: uncommon – polyuria, dysuria; frequency unknown – deterioration of renal function (in patients with renal failure).
Disorders of the genital organs and mammary gland: infrequently – erectile dysfunction; very rarely – gynecomastia (in elderly patients, completely disappearing after discontinuation of the drug), galactorrhea.
General disorders and disorders at the injection site: often – asthenia, weakness; infrequently – nonspecific pain, chills.
*may lead to life-threatening conditions
**cases have been reported when used as a tocolytic during pregnancy (see section “Use during pregnancy and breastfeeding”)
In patients on hemodialysis, with malignant arterial hypertension or with a reduced circulating blood volume, a pronounced decrease in blood pressure may occur as a result of vasodilation.
Interaction
Interaction
Pharmacokinetic interactions
Medicines that affect the metabolism of nifedipine
Nifedipine is metabolized by CYP3A4/5 isoenzymes, which are located in the intestinal mucosa and liver. Drugs that inhibit or induce this enzyme system may affect the first pass effect through the liver (after oral administration) or the clearance of nifedipine.
Inducers of the CYP3A4 isoenzyme
Rifampicin
Rifampin is a potent inducer of the CYP3A4 isoenzyme. When used simultaneously with rifampicin, the bioavailability of nifedipine is significantly reduced and, accordingly, its effectiveness is reduced. Therefore, the simultaneous use of nifedipine with rifampicin is contraindicated.
Antiepileptic drugs that induce CYP3A4 (eg, phenytoin, carbamazepine, phenobarbital)
Phenytoin induces the CYP3A4 isoenzyme. With the simultaneous use of nifedipine and phenytoin, the bioavailability of nifedipine is reduced and its effectiveness is reduced. When using this combination simultaneously, it is necessary to monitor the clinical response to nifedipine therapy and, if necessary, increase its dose. If the dose of nifedipine is increased with simultaneous use of both drugs, the dose of nifedipine should be reduced after discontinuation of phenytoin.
Clinical studies examining the potential interaction between nifedipine and carbamazepine or phenobarbital have not been conducted. Since both drugs reduce the concentration of nimodipine in the blood plasma, which is structurally similar to BMCC, the possibility of a decrease in the concentration of nifedipine in the blood plasma and a decrease in its effectiveness cannot be excluded.
CYP3A4 isoenzyme inhibitors
Macrolide antibiotics (for example, erythromycin)
Clinical studies on the interaction of nifedipine and macrolide antibiotics have not been conducted. Some macrolides are known to inhibit the CYP3A4 isoenzyme. As a result, the possibility of an increase in the concentration of nifedipine in the blood plasma cannot be excluded with the simultaneous use of nifedipine and macrolide antibiotics.
Azithromycin, a macrolide antibiotic, does not inhibit the CYP3A4 isoenzyme.
HIV protease inhibitors (eg, ritonavir)
Clinical studies examining the interaction of nifedipine and HIV protease inhibitors have not been conducted. It is known that drugs of this class inhibit the CYP3A4 isoenzyme. In addition, drugs of this class have been shown to suppress the metabolism of nifedipine mediated by the CYP3A4 isoenzyme in vitro. When used simultaneously with nifedipine, a significant increase in the concentration of nifedipine in the blood plasma cannot be ruled out due to a decrease in the effect of “first pass” through the liver and slower elimination.
Azole antifungals (eg, ketoconazole)
Clinical studies examining the interaction of nifedipine and azole antifungals have not been conducted. It is known that drugs of this class inhibit the CYP3A4 isoenzyme. When used simultaneously with nifedipine, a significant increase in the systemic bioavailability of nifedipine is possible by reducing the effect of “first pass” through the liver.
Cimetidine and ranitidine
It has been established that cimetidine and ranitidine inhibit the CYP3A4 isoenzyme and cause an increase in the concentration of nifedipine in the blood plasma (by 80% and 70%, respectively), thereby enhancing its antihypertensive effect.
Diltiazem
Diltiazem reduces the clearance of nifedipine. This combination should be used with caution. A dose reduction of nifedipine may be required.
Fluoxetine
Clinical studies examining the interaction of nifedipine and fluoxetine have not been conducted. It is known that fluoxetine in vitro suppresses the metabolism of nifedipine, mediated by the action of the CYP3A4 isoenzyme. Therefore, the possibility of an increase in the concentration of nifedipine in the blood plasma cannot be excluded with the simultaneous use of nifedipine and fluoxetine.
Nefazodone
Clinical studies examining the interaction between nifedipine and nefazodone have not been conducted. Nefazodone is known to inhibit the metabolism of other drugs mediated by the CYP3A4 isoenzyme. Therefore, the possibility of an increase in the concentration of nifedipine in the blood plasma cannot be excluded when nifedipine and nefazodone are used simultaneously.
Quinidine
Increased plasma concentrations of nifedipine have been reported when administered concomitantly with quinidine. Therefore, careful monitoring of blood pressure is necessary when using quinidine and nifedipine simultaneously. If necessary, the dose of nifedipine should be reduced.
Quinupristin/dalfopristin
Concomitant use of quinupristin/dalfopristin may lead to increased plasma concentrations of nifedipine.
Valproic acid
Clinical studies examining the interaction of nifedipine and valproic acid have not been conducted. Since valproic acid increases the concentration of nimodipine in the blood plasma, which is structurally similar to BMCC, the possibility of increasing the concentration of nifedipine in the blood plasma and enhancing its effectiveness cannot be excluded.
Grapefruit juice
Grapefruit juice inhibits the CYP3A4 isoenzyme and suppresses the metabolism of nifedipine. The simultaneous use of the drug with grapefruit juice leads to an increase in the concentration of nifedipine in the blood plasma and a prolongation of its action due to a decrease in the effect of “primary passage” through the liver and a decrease in clearance. This may enhance the antihypertensive effect of nifedipine. With regular consumption of grapefruit juice, this effect can last for 3 days after the last consumption of the juice. Consumption of grapefruit/grapefruit juice during treatment with nifedipine is contraindicated.
CYP3A4 isoenzyme substrates
Substrates of the CYP3A4 isoenzyme (for example, cisapride, tacrolimus, benzodiazepines, imipramine, propafenone, terfenadine, warfarin), when used simultaneously with nifedipine, may act as CYP3A4 inhibitors and increase the concentration of nifedipine in the blood plasma.
Cisapride
Concomitant use of cisapride and nifedipine may lead to increased plasma concentrations of nifedipine.
Effect of nifedipine on other drugs
Quinidine
Nifedipine causes a decrease in the concentration of quinidine in the blood plasma. After discontinuation of nifedipine, a sharp increase in the concentration of quinidine in the blood plasma may occur. Therefore, when using nifedipine as additional therapy or discontinuing nifedipine, the concentration of quinidine in the blood plasma should be monitored and, if necessary, its dose should be adjusted.
Digoxin
The simultaneous use of nifedipine and digoxin may lead to a decrease in the clearance of digoxin and, consequently, to an increase in the concentration of digoxin in the blood plasma. The patient should be carefully monitored for symptoms of glycoside overdose and, if necessary, reduce the dose of digoxin, taking into account its concentration in the blood plasma.
Theophylline
Nifedipine increases the concentration of theophylline in the blood plasma, and therefore the concentration of theophylline in the blood plasma should be monitored. The clinical effect of both drugs when used together does not change.
Tacrolimus
Tacrolimus is metabolized with the participation of the CYP3A4 isoenzyme. Recently published data indicate the possibility of increased tacrolimus concentrations in selected cases when administered concomitantly with nifedipine. When using tacrolimus and nifedipine simultaneously, the concentration of tacrolimus in the blood plasma should be monitored and, if necessary, its dose should be reduced.
Vincristine
Nifedipine slows down the elimination of vincristine from the body and may cause increased side effects of vincristine. If simultaneous use is necessary, reduce the dose of vincristine.
Drugs that bind to blood proteins
Nifedipine can displace drugs characterized by a high degree of binding from protein binding (including indirect anticoagulants – coumarin and indanedione derivatives, anticonvulsants, non-steroidal anti-inflammatory drugs, quinine, salicylates, sulfinpyrazone), as a result of which their concentration in the blood plasma may increase.
Cephalosporins
With the simultaneous administration of cephalosporins (for example, cefixime) and nifedipine in probands, the bioavailability of the cephalosporin increased by 70%.
Pharmacodynamic interactions
Medicines that lower blood pressure
The antihypertensive effect of nifedipine may be enhanced when used simultaneously with antihypertensive drugs, such as diuretics, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists (ARI), other BMCCs, alpha-blockers, phosphodiesterase-5 inhibitors, methyldopa.
When using nifedipine and beta-blockers simultaneously, it is necessary to carefully monitor the patient’s condition, since in some cases the course of chronic heart failure may worsen.
The severity of the decrease in blood pressure increases with the simultaneous use of inhalational anesthetics and tricyclic antidepressants.
Nitrates
When used simultaneously with nitrates, tachycardia increases.
Antiarrhythmic drugs
BMCCs can enhance the negative inotropic effect of antiarrhythmic drugs such as amiodarone and quinidine. Nifedipine should be co-administered with disopyramide and flecainide with caution due to the possible enhancement of the negative inotropic effect.
Magnesium sulfate
It is necessary to carefully monitor blood pressure in pregnant women while using nifedipine with intravenous magnesium sulfate due to the possibility of an excessive decrease in blood pressure, which poses a danger to both the mother and the fetus.
Fentanyl
The simultaneous use of nifedipine and fentanyl can lead to severe arterial hypotension. If possible, it is recommended that nifedipine be discontinued at least 36 hours before fentanyl-based anesthesia.
Calcium preparations
Reduced effectiveness of nifedipine.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs reduce the antihypertensive effect of nifedipine due to suppression of prostaglandin synthesis, as well as sodium and fluid retention in the body.
Sympathomimetics
Sympathomimetic agents reduce the antihypertensive effect of nifedipine.
Estrogens
Estrogens reduce the antihypertensive effect of nifedipine due to fluid retention in the body.
Lithium preparations
When BMCC is used together with lithium drugs, it is possible to increase the manifestation of the neurotoxicity of the latter (nausea, vomiting, diarrhea, ataxia, tremor, tinnitus).
Overdose
Overdose
Symptoms
Nifedipine causes peripheral vasodilation with severe and possibly prolonged systemic arterial hypotension: headache, facial flushing, prolonged pronounced decrease in blood pressure, depression of the sinus node, bradycardia and/or tachycardia, bradyarrhythmia. In case of severe poisoning – loss of consciousness, coma.
Treatment
Treatment of overdose consists of standard procedures for removing the drug from the body. The administration of activated carbon, gastric lavage (if necessary, lavage of the small intestine), and restoration of stable hemodynamic parameters are indicated.
In case of an overdose of long-acting nifedipine preparations, it is necessary to ensure the most complete removal of the drug from the body, and, if possible, lavage of the small intestine in order to prevent further absorption of the active substance. When using laxatives, it should be taken into account that BMCC can cause a decrease in the tone of the intestinal muscles, up to intestinal atony.
The antidote to nifedipine is calcium preparations. Intravenous administration of 10-20 ml of a 10% solution of calcium chloride or calcium gluconate is indicated, followed by switching to a long-term infusion. If the administration of calcium supplements fails to achieve a sufficient increase in blood pressure, it is possible to use alpha-adrenergic agonists (dopamine, norepinephrine).
For bradyarrhythmia – intravenous administration of atropine, beta-adrenergic agonists. For life-threatening bradyarrhythmias, installation of a temporary pacemaker is recommended.
With the development of heart failure – intravenous administration of strophanthin. Infusion therapy is recommended to be carried out with caution due to the risk of volume overload of the heart.
Careful monitoring of the activity of the heart, lungs and excretory system is necessary. It is recommended to monitor the concentration of glucose (insulin release may decrease) and the content of electrolytes (potassium, calcium) in the blood.
Hemodialysis is ineffective due to the high degree of binding to plasma proteins and the relatively small volume of distribution. Plasmapheresis is possible.
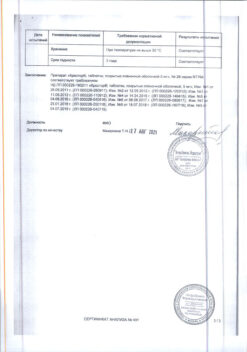
Storage conditions
Storage conditions
Store at a temperature not exceeding 25 ◦C in the original packaging.
Keep out of the reach of children.
Shelf life
Shelf life
5 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Pliva Hrvatska d.o.o., Croatia
Additional information
| Shelf life | 5 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 ◦С in the original packaging. Keep out of the reach of children. |
| Manufacturer | Pliva Hrvatska d.o.o., Croatia |
| Medication form | sustained release tablets |
| Brand | Pliva Hrvatska d.o.o. |
Other forms…
Related products
Buy Corinfar, 10 mg 50 pcs with delivery to USA, UK, Europe and over 120 other countries.