No products in the cart.
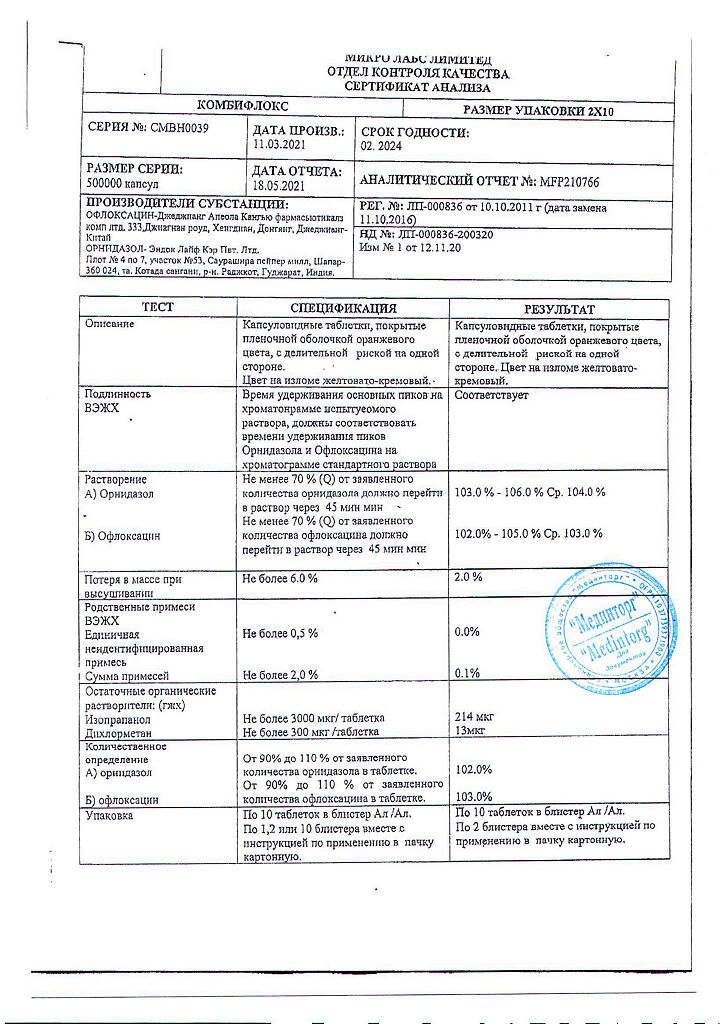
Combiflox, 500 mg+200 mg 10 pcs
€22.55 €18.79
Description
Infectious diseases, Biliary tract infections, Cholecystitis, Urethritis, Urinary tract infections
- mixed bacterial infections caused by sensitive Gram-positive and Gram-negative microorganisms in association with anaerobic microorganisms and/or protozoa;
- infectious inflammatory diseases of the abdominal cavity and biliary tract, kidney (pyelonephritis), lower urinary tract (cystitis, urethritis), genital and pelvic organs (endometritis, salpingitis, oophoritis, cervicitis, parametritis, prostatitis, colpitis, orchitis, epididymitis).
.
Indications
Indications
mixed bacterial infections caused by sensitive gram-positive and gram-negative microorganisms, in association with anaerobic microorganisms and/or protozoa;
infectious and inflammatory diseases of the abdominal cavity and biliary tract, kidneys (pyelonephritis), lower urinary tract (cystitis, urethritis), genital organs and pelvic organs (endometritis, salpingitis, oophoritis, cervicitis, parametritis, prostatitis, colpitis, orchitis, epididymitis).
Pharmacological effect
Pharmacological effect
Pharmacological group: Quinolones/fluoroquinolones in combinations
Special instructions
Special instructions
It is not recommended to be exposed to sunlight or ultraviolet rays (mercury-quartz lamps, solarium).
To prevent urine hyperconcentration and subsequent crystalluria, adequate hydration is recommended during treatment.
In case of side effects from the central nervous system, allergic reactions, pseudomembranous colitis, or development of symptoms of peripheral neuropathy, discontinuation of the drug is necessary.
Rarely, tendinitis can lead to tendon rupture (mostly the Achilles tendon), especially in older patients. If signs of tendinitis occur, you should immediately stop treatment, immobilize the Achilles tendon and consult an orthopedist. During the treatment period, ethanol should not be consumed.
When using the drug, women are not recommended to use sanitary tampons due to the increased risk of developing thrush.
During treatment, the course of myasthenia gravis may worsen and attacks of porphyria may increase in predisposed patients.
When used simultaneously with drugs that prolong the QT interval, class IA and III antiarrhythmics, tricyclic and tetracyclic antidepressants, antipsychotics, macrolides, antifungals, some antihistamines, incl. astemizole, terfenadine, ebastine) systematic ECG monitoring is necessary.
May lead to false negative results in the bacteriological diagnosis of tuberculosis (prevents the isolation of Mycobacterium tuberculosis).
In patients with impaired liver or kidney function, monitoring of plasma concentrations of ofloxacin is necessary. In severe renal failure, the risk of toxic effects increases (reducing dose adjustment is required).
When using the drug, both while taking it and 2-3 weeks after stopping treatment, diarrhea caused by Clistridium difficile (pseudomembranous colitis) may develop. In mild cases, it is sufficient to discontinue treatment and use ion exchange resins (colestyramine, colestipol); in severe cases, replacement of loss of fluid, electrolytes and protein, and the appointment of vancomcin, bacitracin or metronidazole are indicated.
You should not use medications that inhibit intestinal motility.
Active ingredient
Active ingredient
Ornidazole, Ofloxacin
Composition
Composition
1 tablet contains:
active ingredients:
ornidazole 500 mg,
ofloxacin 200 mg
Pregnancy
Pregnancy
The use of the drug during pregnancy and lactation is contraindicated. If it is necessary to use the drug during lactation, breastfeeding should be stopped.
Contraindications
Contraindications
epilepsy (including history);
decreased seizure threshold (including after traumatic brain injury, stroke or inflammatory processes in the central nervous system;
tendon damage due to previous treatment with fluoroquinolones;
age under 18 years;
pregnancy;
lactation period;
hypersensitivity to ofloxacin, ornidazole, other fluoroquinolones and imidazole derivatives, components of the drug.
With caution: cerebral atherosclerosis, cerebrovascular accidents (history), chronic renal failure, liver disease, liver failure, organic diseases of the central nervous system (including multiple sclerosis), predisposition to convulsive reactions, myasthenia gravis, hepatic porphyria, glucose-6-phosphate dehydrogenase deficiency, diabetes mellitus, congenital long Q-T interval syndrome, diseases heart failure (heart failure, myocardial infarction, bradycardia), history of psychosis and other mental disorders; simultaneous use of drugs that prolong the QT interval (class IA and III antiarrhythmics, tricyclic and tetracyclic antidepressants, neuroleptics, macrolides, antifungals, some antihistamines, including astemizole, terfenadine, ebastine), drugs for general anesthesia from the group of barbiturates, drugs that lower blood pressure; electrolyte imbalance (for example, with hypokalemia, hypomagnesemia), old age, alcoholism.
Side Effects
Side Effects
From the digestive system: gastralgia, loss of appetite, nausea, vomiting, diarrhea, constipation, flatulence, abdominal pain, increased activity of liver transaminases, hyperbilirubinemia, cholestatic jaundice, pseudomembranous colitis, dry oral mucosa, colitis (including hemorrhagic), hepatitis.
From the nervous system: headache, dizziness, insomnia, nervousness, uncertainty of movements, tremors, convulsions, numbness and paresthesia of the extremities, intense dreams, “nightmare” dreams, anxiety, state of excitation, phobias, depression, confusion, hallucinations, increased intracranial pressure, insomnia, nervousness, drowsiness, epileptic seizures, extrapyramidal disorders, psychotic reactions with suicidal tendencies, sensory or sensorimotor peripheral neuropathy, impaired motor coordination, temporary loss of consciousness.
From the musculoskeletal system: tendonitis, myalgia, arthralgia, tenosynovitis, tendon rupture, pain in the limbs, muscle rigidity, rhabdomyolysis, muscle weakness.
From the senses: impaired color perception, diplopia, taste disturbances, perversion of taste sensations, disturbances of smell, hearing and balance.
From the cardiovascular system: tachycardia, increase or decrease in blood pressure, collapse, prolongation of the QT interval, ventricular arrhythmia, incl. ventricular tachysystolic arrhythmia of the “pirouette” type.
Allergic reactions: skin rash, itching, urticaria, allergic pneumonitis, allergic nephritis, eosinophilia, fever, angioedema, bronchospasm; exudative erythema multiforme (including Stevens-Johnson syndrome) and toxic epidermal necrolysis (Lyell’s syndrome), photosensitivity, vasculitis, anaphylactic shock, itching of the external genitalia in women.
From the skin: pinpoint hemorrhages (petechiae), bullous hemorrhagic dermatitis, papular rash with crust, indicating vascular damage (vasculitis).
From the hematopoietic organs: leukopenia, agranulocytosis, anemia (including aplastic and hemolytic), thrombocytopenia, pancytopenia.
From the urinary system: acute interstitial nephritis, impaired renal function, hypercreatininemia, increased urea concentration, dysuria, urinary retention, acute renal failure.
Other: intestinal dysbiosis, superinfection, hypoglycemia (in patients with diabetes), vaginitis, chest pain, fatigue, asthenia, general weakness, photosensitivity, vaginal discharge, nosebleeds, thirst, weight loss, pharyngitis, rhinitis, dry cough, acute attack of porphyria (in patients with porphyria).
Interaction
Interaction
Ofloxacin
Antacids containing aluminum hydroxide, sucralfate, magnesium hydroxide, aluminum phosphate or drugs containing zinc, iron. Reduces the absorption of ofloxacin. When using the above drugs and ofloxacin, an approximately two-hour interval should be observed between their doses.
Vitamin K antagonists. An increase in PT/INR values and/or the development of bleeding (including severe bleeding) was observed in patients with simultaneous use of ofloxacin and vitamin K antagonists (for example, warfarin). With the simultaneous use of vitamin K antagonists, control of the blood coagulation system is necessary.
Glibenclamide. Ofloxacin may slightly increase serum concentrations of glibenclamide when administered concomitantly. When using ofloxacin and glibenclamide simultaneously, it is recommended to carefully monitor the patient’s condition and blood glucose concentrations.
Other hypoglycemic drugs for oral administration and insulin. Ofloxacin increases the risk of hypoglycemia; more careful monitoring of blood glucose concentrations is required.
Probenecid, cimetidine, furosemide or methotrexate. When quinolones are used together with drugs that are eliminated from the body by renal tubular secretion (such as probenecid, cimetidine, furosemide, methotrexate), a mutual slowdown in elimination and an increase in serum concentrations are possible (especially in the case of high doses).
Drugs that can lower the threshold for seizure activity in the brain, such as theophylline, fenbufen and other similar NSAIDs. Clinical studies have not established any pharmacokinetic interactions of ofloxacin with theophylline. However, a significant decrease in the threshold of convulsive activity of the brain is possible with the simultaneous use of quinolones with drugs that reduce the threshold of convulsive activity of the brain (theophylline, fenbufen and other similar NSAIDs).
GCS. When used simultaneously with GCS, the risk of tendon rupture increases, especially in elderly patients.
Drugs that can prolong the QT interval. Ofloxacin, like other fluoroquinolones, should be used with caution in patients receiving drugs that can prolong the QT interval (class IA and III antiarrhythmic drugs, tricyclic antidepressants, macrolides, antipsychotics).
Medicines that alkalinize urine (carbonic anhydrase inhibitors, citrates, sodium bicarbonate). When prescribed with drugs that alkalinize urine (carbonic anhydrase inhibitors, citrates, sodium bicarbonate), the risk of developing crystalluria and nephrotoxic effects increases.
Ornidazole
Enhances the effect of indirect coumarin anticoagulants, which requires appropriate dose adjustment.
Extends the muscle relaxant effect of vecuronium bromide.
Compatible with ethanol (does not inhibit acetaldehyde dehydrogenase) unlike other imidazole derivatives (metronidazole).
Phenobarbital or other inducers of microsomal liver enzymes reduce T1/2 of ornidazole from blood plasma.
Inhibitors of microsomal liver enzymes (for example, cimetidine) increase the concentration of ornidazole in the blood plasma.
Overdose
Overdose
Symptoms: dizziness, confusion, lethargy, disorientation, drowsiness, vomiting, epileptiform convulsions, depression, peripheral neuritis.
Treatment: gastric lavage, symptomatic therapy (diazepam for seizures).
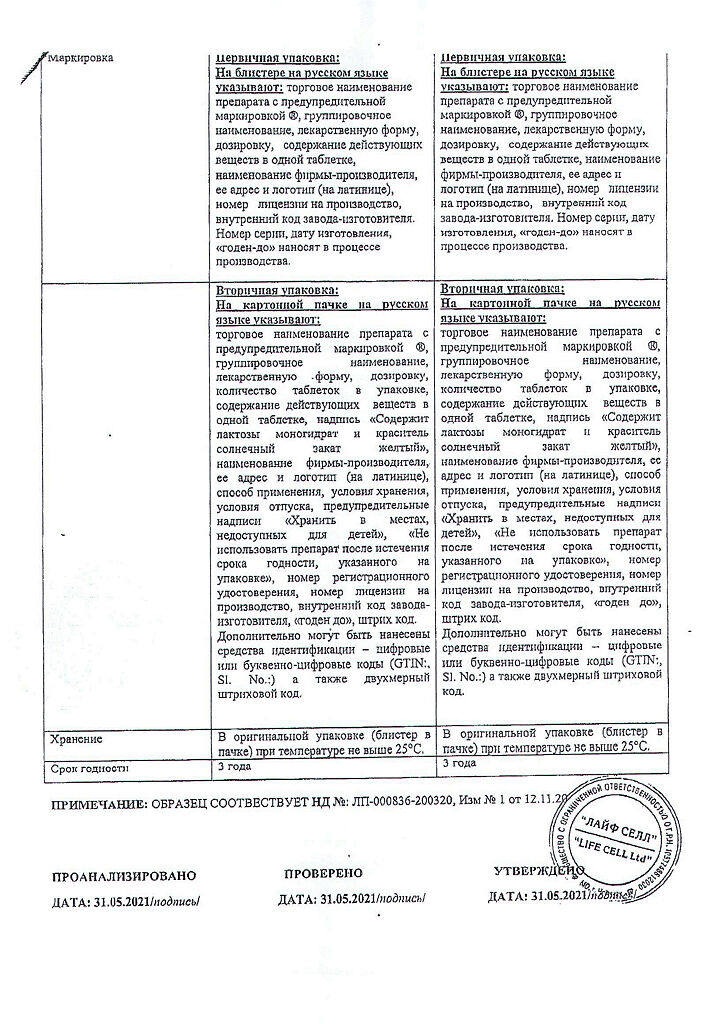
Storage conditions
Storage conditions
In a place protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Micro Labs Ltd, India
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a light-protected place, at a temperature not exceeding 25 °C |
| Manufacturer | Micro Labs Ltd, India |
| Medication form | pills |
| Brand | Micro Labs Ltd |
Other forms…
Related products
Buy Combiflox, 500 mg+200 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.