No products in the cart.
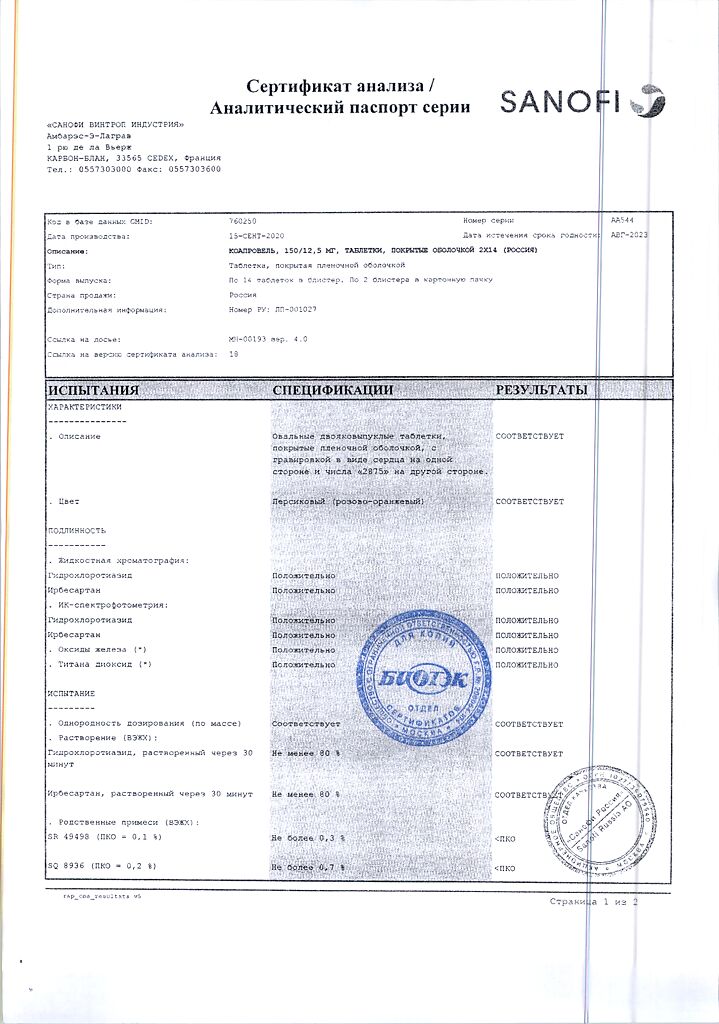
Coaprovel, 12.5 mg+150 mg 28 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Arterial hypertension.
Active ingredient
Active ingredient
Composition
Composition
1 tablet contains irbesartan 150 mg, hydrochlorothiazide 12.5 mg,
excipients:
microcrystalline cellulose,
sodium croscarmellose,
lactose monohydrate,
magnesium stearate,
Colloidal silicon dioxide hydrated,
Pregelatinized corn starch,
Red iron oxide,
Yellow iron oxide.
How to take, the dosage
How to take, the dosage
Coaprovelle can be used once daily before or with meals in patients whose BP is not adequately controlled with irbesartan or hydrochlorothiazide alone.
Coaprovelle150/12.5 mg is indicated for patients whose BP is not well controlled with hydrochlorothiazide or irbesartan (150 mg/day) when taken alone.
The use of the drug in doses greater than 300 mg of irbesartan/25 mg of hydrochlorothiazide once daily is not recommended.
Interaction
Interaction
Other antihypertensive drugs: The antihypertensive effect of COAPROVEL may be enhanced by the use of other antihypertensive drugs. Irbesartan and hydrochlorothiazide (at doses: 300 mg irbesartan/25 hydrochlorothiazide) should be used with caution together with other antihypertensive agents, including calcium channel blockers and beta-adrenoblockers. Pretreatment with high-dose diuretics may lead to hypovolemia and risk of arterial hypotension (see section “Special warnings and precautions for use”).
Lithium: Reversible increases in serum lithium concentrations and toxic effects have been noted with concomitant use of lithium with angiotensin-converting enzyme inhibitors (ARIs). For irbesartan, similar effects have been extremely rare to date. In addition, the renal clearance of lithium is reduced by thiazides, so the risk of lithium toxic effects may be increased with COAPROVEL. Therefore, the combination of lithium and COAPROVEL is not recommended. If the combination is necessary, close monitoring of serum lithium levels is recommended.
Drugs affecting blood potassium levels: the hypokalemic effect of hydrochlorothiazide is attenuated by the potassium-saving effect of irbesartan. However, this effect of hydrochlorothiazide may be enhanced by other drugs that cause potassium loss and hypokalemia (e.g., diuretics, laxatives, amphotericin, carbenoxolone, sodium salt of penicillin G, salicylic acid derivatives). In contrast, based on experience with other drugs that reduce renin-angiotensin system activity, concomitant use of potassium-saving diuretics, potassium supplements, potassium-containing salt substitutes, or other drugs that can increase serum potassium levels (e.g., heparin sodium salt) may result in an increase in serum potassium. Adequate monitoring of serum potassium levels is recommended in patients at risk.
Medications affected by serum potassium imbalance: Periodic monitoring of serum potassium levels is recommended in case of co-administration of COAPROVEL and medications affected by serum potassium imbalance (e.g. foxglove glycosides, antiarrhythmic agents).
Non-steroidal anti-inflammatory drugs: simultaneous use of angiotensin II antagonists and non-steroidal anti-inflammatory drugs (e.g., selective COX-2 inhibitors, acetylsalicylic acid (>3 g/day) and non-selective NSAIDs) may decrease the hypotensive effect.
As with ACE inhibitors, co-administration of angiotensin II antagonists and NSAIDs may increase the risk of renal dysfunction, including the possibility of acute renal failure, and lead to increased serum potassium levels, especially in patients with already impaired renal function. Precautions should be observed when administering this combination, especially in elderly patients. Patients should not be dehydrated. Renal function monitoring should be performed after initiation of combination therapy and periodically thereafter.
Further information on irbesartan interactions: The pharmacokinetics of irbesartan are not affected when combined with hydrochlorothiazide. Irbesartan is primarily metabolized by CYP2C9 and, to a lesser extent, by glucuronidation. No significant pharmacokinetic and pharmacodynamic interactions have been observed when irbesartan is coadministered with warfarin, a drug that is metabolized by CYP2C9. The effects of CYP2C9 inducers, such as rifampicin, on the pharmacokinetics of irbesartan have not been evaluated. The pharmacokinetics of digoxin were not altered when co-administered with irbesartan.
Additional information on hydrochlorothiazide interactions: The following drugs may interact with thiazide diuretics:
Alcohol, barbiturates, or narcotic drugs: increased orthostatic hypotension may be observed;
Hypoglycemic drugs (oral agents and insulin): hypoglycemic drug dose adjustment may be required (see Special Warnings and Precautions for Use);
Colestyramine and colestyrol resins: Absorption of hydrochlorothiazide is reduced in the presence of anion-exchange resins;
Glucocorticosteroids, ACTH: more severe electrolyte disturbances are possible, particularly increased hypokalemia;
Foxglove glycosides: Hypokalemia and hypomagnesemia caused by a thiazide diuretic contribute to foxglove-induced arrhythmias (see Special Warnings and Precautions for Use);
Non-steroidal anti-inflammatory drugs: The use of nonsteroidal anti-inflammatory drugs may reduce the effects of thiazide diuretics in some patients;
Catecholamines (e.g., noradrenaline): the effects of these agents may be impaired;
Nondepolarizing myorelaxants : The effects of nondepolarizing myorelaxants may be enhanced by hydrochlorothiazide;
Antipodagretic agents: dosages of antipodagretic agents may need to be adjusted because hydrochlorothiazide may increase serum uric acid levels. It may be necessary to increase the dosage of probenecid or sulfinpyrazone. Co-administration with thiazide diuretics may increase the incidence of allopurinol allergic reactions;
Calcium salts: Thiazide diuretics may increase serum calcium levels due to reduced excretion. If calcium supplements or medicines which influence calcium level (for example, in case of vitamin D therapy) should be administered, it is necessary to control the calcium levels in serum and to correct the dose of calcium preparation accordingly.
Other interactions: hyperglycemic effect of beta-adrenoblockers and diazoxide can be enhanced by thiazides.
The anticholinergic agents (e.g., atropine) may increase the bioavailability of thiazide-type diuretics by reducing gastrointestinal motility. Thiazides may increase the risk of amantadine-induced side effects. Thiazides may decrease urinary excretion of cytotoxic drugs (e.g., cyclophosphamide, methotrexate) and increase their myelosuppressive effects.
Special Instructions
Special Instructions
The risk of significant BP decrease is increased with decreased blood pressure and hyponatremia caused by diuretics, low Na+ diet, diarrhea, vomiting, therefore these conditions should be corrected before the start of therapy with the drug. In patients with CKD during therapy with thiazide diuretics azotemia may occur. Periodic monitoring of serum K+, creatinine and uric acid concentrations is recommended.
There is no experience of using the drug in patients with recent kidney transplantation. Therapy with thiazide diuretics may cause minifestation of latent diabetes mellitus and also decrease glucose tolerance. In patients with diabetes mellitus, doses of insulin or oral hypoglycemic drugs may need to be adjusted. Therapy with hydrochlorthiazide at a dose of 12.5 mg contained in the drug has almost no effect on the concentration of cholesterol and triglycerides. When therapy with thiazide diuretics, hyperuricemia or aggravation of gout may be observed.
The treatment with hydrochlorothiazide may lead to disorders of water-electrolyte balance (hypokalemia, hyponatremia and hypochloremic alkalosis). Concomitant use of irbesartan may decrease hypokalemia caused by the diuretic. The risk of hypokalemia increases with concomitant treatment with GCS or ACTH. Irbesartan may lead to hyperkalemia, especially in the presence of renal failure and/or CHF or diabetes mellitus.
Periodic monitoring of serum K+ concentrations is recommended during treatment. There is no evidence that irbesartan can reduce or prevent diuretic-induced hyponatremia. Cl- deficiency is usually minor and does not require treatment. Thiazide diuretics may cause hypomagnesemia and also reduce renal calcium excretion and cause minor hypercalcemia provided there is no impairment of Ca2+ metabolism. Hypercalcemia may be a sign of latent hyperparathyroidism; in this case the drug should be discontinued until parathyroid function tests are performed.
Hydrochlorothiazide may cause a positive doping test. In patients whose vascular tone and renal function depends mainly on the activity of the renin-angiotensin-aldosterone system (including CHF, renal disease, including renal artery stenosis), therapy with angiotensin II receptor antagonists may cause marked BP decrease, azotemia, oliguria or, in rare cases, acute renal failure.
The excessive reduction of BP in CHD or other cardiovascular diseases may lead to myocardial infarction or stroke. Development of allergic reactions to hydrochlorothiazide is more likely in patients with such reactions in the history. When using thiazide diuretics, exacerbation of SLE has been reported. It should be taken into account that in rare cases during the treatment dizziness and increased fatigability may be observed, therefore caution should be exercised while exercising potentially dangerous activities, requiring increased concentration and quick psychomotor reaction (including driving).
Contraindications
Contraindications
– II and III trimesters of pregnancy;
– hypersensitivity to the components of Coaprovel;
– hypersensitivity to other sulfonamide derivatives.
For the use of hydrochlorothiazide:
– severe renal failure (CK < 30 ml/min);
– refractory hypokalemia, hypercalcemia;
– severe hepatic insufficiency;
– biliary cirrhosis;
– cholestasis.
Side effects
Side effects
Blood system disorders: aplastic anemia, bone marrow depression, hemolytic anemia, leukopenia, neutropenia/agranulocytosis, thrombocytopenia.
CNS and peripheral nervous system disorders: depression, sleep disturbances, dizziness, paresthesias, anxiety.
Visually: transient blurred vision, xanthopsia.
Cardiovascular system: arrhythmia, postural hypotension.
Respiratory system: respiratory distress syndrome (including pneumonitis and pulmonary edema).
Digestive system disorders: jaundice (intrahepatic cholestatic jaundice).
Allergic reactions: anaphylactic reactions, toxic necrosis of the epidermis, skin reactions such as lupus erythematosus, necrotizing angiitis (vasculitis, cutaneous vasculitis), photosensitivity reactions, rash, exacerbation of skin manifestations of lupus erythematosus, urticaria.
Muscular system disorders: muscle cramps, weakness.
Urinary system: interstitial nephritis, renal dysfunction.
Others: increase in body temperature.
Laboratory disorders: electrolyte balance disorders (including hypokalemia and hyponatremia), glucosuria, hyperglycemia, hyperuricemia, elevated cholesterol and TG levels.
Overdose
Overdose
There is no specific information on overdose during therapy with COAPROVEL. In case of overdose, close monitoring of the patient’s condition is required and therapy should be symptomatic and supportive. The type of care depends on the time since the medication was taken and the severity of the symptoms. Recommended measures include inducing vomiting and/or gastric lavage. In overdose, the use of activated charcoal may be helpful. Frequent monitoring of serum electrolyte and creatinine levels should be performed. In case of arterial hypotension, the patient should be laid on his back with elevation of the lower extremities and as soon as possible to carry out reimbursement of salts and fluids.
The most likely manifestations of irbesartan overdose are arterial hypotension and tachycardia; bradycardia may also occur.
Hydrochlorothiazide overdose is accompanied by a decrease in electrolytes in the body (hypokalemia, hyponatremia) and dehydration due to excessive diuresis. The most common signs and symptoms of overdose are nausea and drowsiness. Hypokalemia may lead to seizures and/or increased arrhythmias in case of concomitant use of foxglove glycosides and antiarrhythmic drugs.
Irbesartan is not excreted by hemodialysis. The degree of excretion of hydrochlorothiazide by hemodialysis has not been determined.
Additional information
| Weight | 0.020 kg |
|---|---|
| Shelf life | 3 years |
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Sanofi Winthrop Industry, France |
| Medication form | pills |
| Brand | Sanofi Winthrop Industry |
Related products
Buy Coaprovel, 12.5 mg+150 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.