No products in the cart.
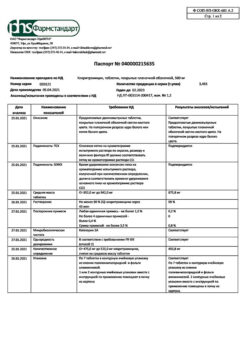
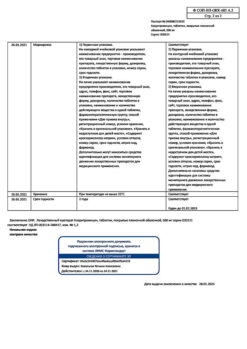
Clarithromycin-Vertex, 250 mg capsules 14 pcs
€6.43 €5.63
Out of stock
(E-mail when Stock is available)
Description
Otitis, Angina, Colds, Gastric and duodenal ulcers, Bronchitis, Respiratory tract infections, Sinusitis, GI infections caused by Helicobacter pylori, Tonsillitis, Boils, Skin infections, Pharyngitis
Infectious and inflammatory diseases caused by clarithromycin-sensitive microorganisms:
– Lower respiratory tract infections (such as bronchitis, pneumonia);
– Upper respiratory tract infections (such as pharyngitis, sinusitis);
– Skin and soft tissue infections (such as folliculitis, subcutaneous inflammation, rust);
– Disseminated or localized mycobacterial infections caused by Mycobacterium avium and Mycobacterium intracellulare; localized infections caused by Mycobacterium chelonae, Mycobacterium fortuitum, and Mycobacterium kansasii;
– Preventing the spread of infection caused by Mycobacterium avium complex (MAC) in HIV-infected patients with CD4 (Tcheloper lymphocyte) counts of 100 or less in 1 mm3;
– Eradication of H. pylori and reduced recurrence rate of duodenal ulcer;
– Odontogenic infections.
Indications
Indications
Infectious and inflammatory diseases caused by microorganisms sensitive to clarithromycin:
– Lower respiratory tract infections (such as bronchitis, pneumonia);
– Upper respiratory tract infections (such as pharyngitis, sinusitis);
– Infections of the skin and soft tissues (such as folliculitis, inflammation of the subcutaneous tissue, erysipelas);
– Disseminated or localized mycobacterial infections caused by Mycobacterium avium and Mycobacterium intracellulare; localized infections caused by Mycobacterium chelonae, Mycobacterium fortuitum and Mycobacterium kansasii;
– Prevention of the spread of infection caused by the Mycobacterium avium complex (MAC) to HIV-infected patients with a CD4 lymphocyte (T-helper lymphocyte) content of no more than 100 per 1 mm3;
– Eradication of H. pylori and reduction in the frequency of relapses of duodenal ulcers;
– Odontogenic infections.
Pharmacological effect
Pharmacological effect
Pharmacokinetics
Special instructions
Special instructions
Liver dysfunction (increased liver enzyme activity in the blood, hepatocellular and/or cholestatic hepatitis with or without jaundice) has been reported with the use of clarithromycin. Liver dysfunction can be severe but is usually reversible. There have been cases of fatal liver failure, mainly associated with the presence of serious concomitant diseases and/or concomitant use of other drugs. If signs and symptoms of hepatitis appear, such as anorexia, jaundice, dark urine, itching, abdominal tenderness on palpation, clarithromycin therapy should be stopped immediately.
In the presence of chronic liver diseases, it is necessary to regularly monitor the activity of serum enzymes.
When treated with almost all antibacterial agents, including clarithromycin, cases of pseudomembranous colitis have been described, the severity of which can range from mild to life-threatening. Clostridium difficile-associated diarrhea has been reported with almost all antibacterial agents, including clarithromycin, and can range in severity from mild diarrhea to life-threatening colitis. Antibacterial drugs can alter the normal intestinal microflora, which can lead to the growth of C. difficile. Pseudomembranous colitis caused by Clostridium difficile should be suspected in any patient who develops diarrhea after taking antibacterial agents. Cases of the development of pseudomembranous colitis 2 months after taking an antibiotic have been described.
Long-term use of antibiotics can lead to the formation of colonies with an increased number of insensitive bacteria and fungi. In case of superinfection, appropriate therapy must be prescribed. After a course of antibiotic therapy, careful medical monitoring of the patient is necessary.
When treated with macrolides, including clarithromycin, prolongation of cardiac repolarization and QT interval was observed, causing the risk of developing cardiac arrhythmia and torsade de pointes (see section “Side effects”). Since the following situations may lead to an increased risk of developing ventricular arrhythmias (including torsade de pointes),
– clarithromycin should not be used in the following categories of patients:
· in patients with hypokalemia (see section “Contraindications”);
· simultaneous administration of clarithromycin with astemizole, cisapride, pimozide and terfenadine is contraindicated (see section “Contraindications”);
· in patients with congenital or acquired registered prolongation of the QT interval or a history of ventricular arrhythmia.
– Clarithromycin should be used with caution in the following categories of patients:
· in patients with coronary heart disease (CHD), severe heart failure, conduction disorders or clinically significant bradycardia;
· in patients with electrolyte disturbances such as hypomagnesemia;
· in patients simultaneously taking other drugs associated with prolongation of the QT interval (see section “Interaction with other drugs”).
It is possible to develop cross-resistance to clarithromycin and other macrolide antibiotics, as well as lincomycin and clindamycin.
Given the increasing resistance of Streptococcus pneumoniae to macrolides, it is important to perform susceptibility testing when prescribing clarithromycin to patients with community-acquired pneumonia. For hospital-acquired pneumonia, clarithromycin should be used in combination with appropriate antibiotics.
Mild to moderate skin and soft tissue infections are most often caused by Staphylococcus aureus and Streptococcus pyogenes. Moreover, both pathogens can be resistant to macrolides. Therefore, it is important to conduct a sensitivity test.
Macrolides can be used for infections caused by Corynebacterium minutissimum (erythrasma), acne vulgaris and erysipelas, as well as in situations where penicillin cannot be used.
If acute hypersensitivity reactions occur, such as anaphylactic reaction, Stevens-Johnson syndrome, toxic epidermal necrolysis, drug rash with eosinophilia and systemic symptoms (DRESS syndrome), you should immediately stop taking clarithromycin and begin appropriate therapy.
In case of combined use with warfarin or other indirect anticoagulants, it is necessary to monitor the INR and prothrombin time.
Impact on the ability to drive vehicles and machinery
There are no data regarding the effect of clarithromycin on the ability to drive a car or use machinery.
Caution should be exercised when operating vehicles and machinery, given the potential for dizziness, vertigo, confusion and disorientation that may occur while using this drug.
Active ingredient
Active ingredient
Clarithromycin
Composition
Composition
Composition per tablet
Active ingredient:
Clarithromycin in terms of 100% anhydrous substance – 250.0 mg.
Excipients: potato starch – 46.0 mg, microcrystalline cellulose – 75.0 mg, povidone K-17 (low molecular weight medical polyvinylpyrrolidone 12600 ± 2700) – 40.0 mg, pregelatinized starch (starch-1500) – 30.0 mg, colloidal silicon dioxide (aerosil) – 4.5 mg, magnesium stearate – 4.5 mg.
Shell: opadry II (polyvinyl alcohol, partially hydrolyzed – 8,000 mg, macrogol (polyethylene glycol 3350) – 4,040 mg, talc – 2,960 mg, titanium dioxide E171 – 4,374 mg, aluminum varnish based on yellow quinoline E104 – 0,602 mg, iron dye oxide II E172 – 0.006 mg, aluminum varnish based on sunset yellow E110 – 0.014 mg, aluminum varnish based on indigo carmine E132 – 0.004 mg).
Pregnancy
Pregnancy
The safety of clarithromycin during pregnancy and breastfeeding has not been established.
The use of clarithromycin during pregnancy (especially in the first trimester) is possible only when there is no alternative therapy and the potential benefit to the mother outweighs the potential risk to the fetus.
Clarithromycin is excreted in breast milk. If it is necessary to take it during lactation, breastfeeding should be stopped.
Contraindications
Contraindications
Simultaneous use of clarithromycin with colchicine (see section “Interaction with other drugs”).
– Concomitant use of clarithromycin with ticagrelor or ranolazine.
– History of QT interval prolongation (congenital or acquired recorded QT interval prolongation) or ventricular arrhythmia, including torsade de pointes (see sections “Special Instructions” and “Interaction with Other Drugs”).
– Hypokalemia (risk of QT interval prolongation).
– Severe liver failure occurring simultaneously with renal failure.
– A history of cholestatic jaundice/hepatitis that developed during the use of clarithromycin (see section “Special Instructions”).
– Porfiria.
– Breastfeeding period.
– Age up to 12 years (efficacy and safety have not been established).
With caution
– Moderate to severe renal failure.
– Moderate to severe liver failure.
– Concomitant use of clarithromycin with benzodiazepines such as alprazolam, triazolam, midazolam for intravenous use or for application to the oral mucosa (see section “Interaction with other drugs”).
– Concomitant use with drugs that are metabolized by the CYP3A isoenzyme, for example, carbamazepine, cilostazol, cyclosporine, disopyramide, methylprednisolone, omeprazole, indirect anticoagulants (for example, warfarin), quinidine, rifabutin, sildenafil, tacrolimus, vinblastine (see section “Interaction with other drugs”).
– Concomitant use with drugs that induce the CYP3A4 isoenzyme, for example, rifampicin, phenytoin, carbamazepine, phenobarbital, St. John’s wort (see section “Interaction with other drugs”).
– Concomitant use of clarithromycin with statins that do not depend on the metabolism of the CYP3A isoenzyme (for example, fluvastatin) (see section “Interaction with other drugs”).
– Concomitant use with blockers of “slow” calcium channels that are metabolized by the CYP3A4 isoenzyme (for example, verapamil, amlodipine, diltiazem).
– Patients with coronary heart disease (CHD), severe heart failure, hypomagnesemia, conduction disturbances or clinically significant bradycardia, as well as patients simultaneously taking class IA (quinidine, procainamide) and class III antiarrhythmic drugs (dofetilide, amiodarone, sotalol).
– Pregnancy.
Side Effects
Side Effects
Classification of adverse reactions by frequency (number of reported cases/number of patients): very common (≥1/10), common (≥1/100, <1/10), uncommon (≥1/1000, <1/100), frequency unknown (side effects from post-marketing experience; frequency cannot be estimated based on available data).
Allergic reactions
Common: rash.
Uncommon: hypersensitivity, itching, urticaria.
Not known: anaphylactic reaction, angioedema, Stevens-Johnson syndrome, toxic epidermal necrolysis, drug rash with eosinophilia and systemic symptoms (DRESS syndrome).
From the nervous system
Common: headache, insomnia.
Uncommon: dizziness, drowsiness, tremor, restlessness.
Frequency unknown: seizures, psychotic disorders, confusion, depersonalization, depression, disorientation, hallucinations, dream disturbances (nightmare dreams), paresthesia, mania.
From the skin
Common: intense sweating.
Frequency unknown: acne.
From the urinary system
Frequency unknown: renal failure, interstitial nephritis.
Metabolism and nutrition
Uncommon: anorexia, decreased appetite.
From the musculoskeletal system
Frequency unknown: myopathy.
From the digestive system
Common: diarrhea, vomiting, dyspepsia, nausea, abdominal pain.
Uncommon: gastritis, stomatitis, glossitis, bloating, constipation, dry mouth, belching, flatulence, cholestasis, hepatitis, etc. cholestatic or hepatocellular.
Frequency unknown: acute pancreatitis, discoloration of the tongue and teeth, liver failure, cholestatic jaundice.
From the senses
Common: dysgeusia, taste perversion.
Uncommon: vertigo, hearing loss, tinnitus.
Frequency unknown: deafness, ageusia (loss of taste), parosmia, anosmia.
From the cardiovascular system
Uncommon: prolongation of the QT interval on the electrocardiogram, palpitations.
Frequency unknown: ventricular tachycardia, including pirouette type, ventricular fibrillation, bleeding.
Laboratory indicators
Common: abnormal liver function test.
Uncommon: leukopenia, neutropenia, eosinophilia, increased activity of: alanine aminotransferase (ALT), aspartate aminotransferase (AST), gammaglutamyltransferase (GGTP), alkaline phosphatase, lactate dehydrogenase (LDH).
Frequency unknown: agranulocytosis, thrombocytopenia, increased international normalized ratio (INR), prolongation of prothrombin time, change in urine color, increased bilirubin concentration in the blood.
General disorders
Uncommon: malaise, asthenia, chest pain, chills, fatigue.
Infectious and parasitic diseases
Uncommon: candidiasis.
Frequency unknown: pseudomembranous colitis, erysipelas.
Immunosuppressed patients
In patients with AIDS and other immunodeficiencies receiving clarithromycin in higher doses over a long period of time for the treatment of mycobacterial infections, it is often difficult to distinguish adverse effects of the drug from symptoms of HIV infection or concomitant disease.
The most common adverse events in patients taking a daily dose of clarithromycin of 1000 mg were: nausea, vomiting, taste disturbance, abdominal pain, diarrhea, rash, flatulence, headache, constipation, hearing loss, increased AST and ALT activity in the blood. Low incidence adverse events such as shortness of breath, insomnia and dry mouth were also reported.
In patients with suppressed immunity, laboratory parameters were assessed, analyzing their significant deviations from the norm (sharp increase or decrease). Based on this criterion, significant increases in AST and ALT levels, as well as decreases in white blood cell and platelet counts, were reported in 2–3% of patients receiving clarithromycin 1000 mg daily. In a small number of patients, an increase in the concentration of residual nitrogen and urea was also recorded.
Interaction
Interaction
Liver dysfunction (increased liver enzyme activity in the blood, hepatocellular and/or cholestatic hepatitis with or without jaundice) has been reported with the use of clarithromycin. Liver dysfunction can be severe but is usually reversible. There have been cases of fatal liver failure, mainly associated with the presence of serious concomitant diseases and/or concomitant use of other drugs. If signs and symptoms of hepatitis appear, such as anorexia, jaundice, dark urine, itching, abdominal tenderness on palpation, clarithromycin therapy should be stopped immediately.
In the presence of chronic liver diseases, it is necessary to regularly monitor the activity of serum enzymes.
When treated with almost all antibacterial agents, including clarithromycin, cases of pseudomembranous colitis have been described, the severity of which can range from mild to life-threatening. Clostridium difficile-associated diarrhea has been reported with almost all antibacterial agents, including clarithromycin, and can range in severity from mild diarrhea to life-threatening colitis. Antibacterial drugs can alter the normal intestinal microflora, which can lead to the growth of C. difficile. Pseudomembranous colitis caused by Clostridium difficile should be suspected in any patient who develops diarrhea after taking antibacterial agents. Cases of the development of pseudomembranous colitis 2 months after taking an antibiotic have been described.
Long-term use of antibiotics can lead to the formation of colonies with an increased number of insensitive bacteria and fungi. In case of superinfection, appropriate therapy must be prescribed. After a course of antibiotic therapy, careful medical monitoring of the patient is necessary.
When treated with macrolides, including clarithromycin, prolongation of cardiac repolarization and QT interval was observed, causing the risk of developing cardiac arrhythmia and torsade de pointes (see section “Side effects”). Since the following situations may lead to an increased risk of developing ventricular arrhythmias (including torsade de pointes),
– clarithromycin should not be used in the following categories of patients:
· in patients with hypokalemia (see section “Contraindications”);
· simultaneous administration of clarithromycin with astemizole, cisapride, pimozide and terfenadine is contraindicated (see section “Contraindications”);
· in patients with congenital or acquired registered prolongation of the QT interval or a history of ventricular arrhythmia.
– Clarithromycin should be used with caution in the following categories of patients:
· in patients with coronary heart disease (CHD), severe heart failure, conduction disorders or clinically significant bradycardia;
· in patients with electrolyte disturbances such as hypomagnesemia;
· in patients simultaneously taking other drugs associated with prolongation of the QT interval (see section “Interaction with other drugs”).
It is possible to develop cross-resistance to clarithromycin and other macrolide antibiotics, as well as lincomycin and clindamycin.
Given the increasing resistance of Streptococcus pneumoniae to macrolides, it is important to perform susceptibility testing when prescribing clarithromycin to patients with community-acquired pneumonia. For hospital-acquired pneumonia, clarithromycin should be used in combination with appropriate antibiotics.
Mild to moderate skin and soft tissue infections are most often caused by Staphylococcus aureus and Streptococcus pyogenes. Moreover, both pathogens can be resistant to macrolides. Therefore, it is important to conduct a sensitivity test.
Macrolides can be used for infections caused by Corynebacterium minutissimum (erythrasma), acne vulgaris and erysipelas, as well as in situations where penicillin cannot be used.
If acute hypersensitivity reactions occur, such as anaphylactic reaction, Stevens-Johnson syndrome, toxic epidermal necrolysis, drug rash with eosinophilia and systemic symptoms (DRESS syndrome), you should immediately stop taking clarithromycin and begin appropriate therapy.
In case of combined use with warfarin or other indirect anticoagulants, it is necessary to monitor the INR and prothrombin time.
Impact on the ability to drive vehicles and machinery
There are no data regarding the effect of clarithromycin on the ability to drive a car or use machinery.
Caution should be exercised when operating vehicles and machinery, given the potential for dizziness, vertigo, confusion and disorientation that may occur while using this drug.
When taking saquinavir with ritonavir, consider the potential effect of ritonavir on clarithromycin.
Overdose
Overdose
Symptoms. Taking a large dose of clarithromycin may cause gastrointestinal symptoms.
In one patient with a history of bipolar disorder, changes in mental status, paranoid behavior, hypokalemia, and hypoxemia were described after taking 8 g of clarithromycin.
Treatment. In case of overdose, the unabsorbed drug should be removed from the gastrointestinal tract (gastric lavage, taking activated charcoal, etc.) and symptomatic therapy should be carried out. Hemodialysis and peritoneal dialysis do not have a significant effect on the concentration of clarithromycin in serum, which is also typical for other macrolide drugs.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
Vertex, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | Vertex, Russia |
| Medication form | capsules |
| Brand | Vertex |
Other forms…
Related products
Buy Clarithromycin-Vertex, 250 mg capsules 14 pcs with delivery to USA, UK, Europe and over 120 other countries.