No products in the cart.
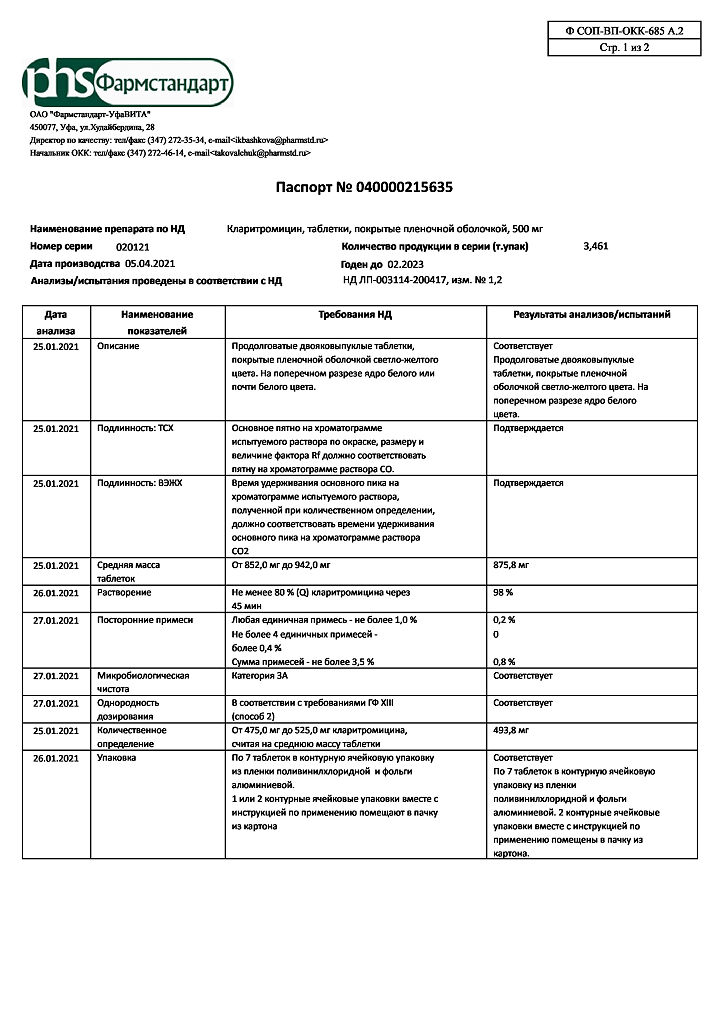
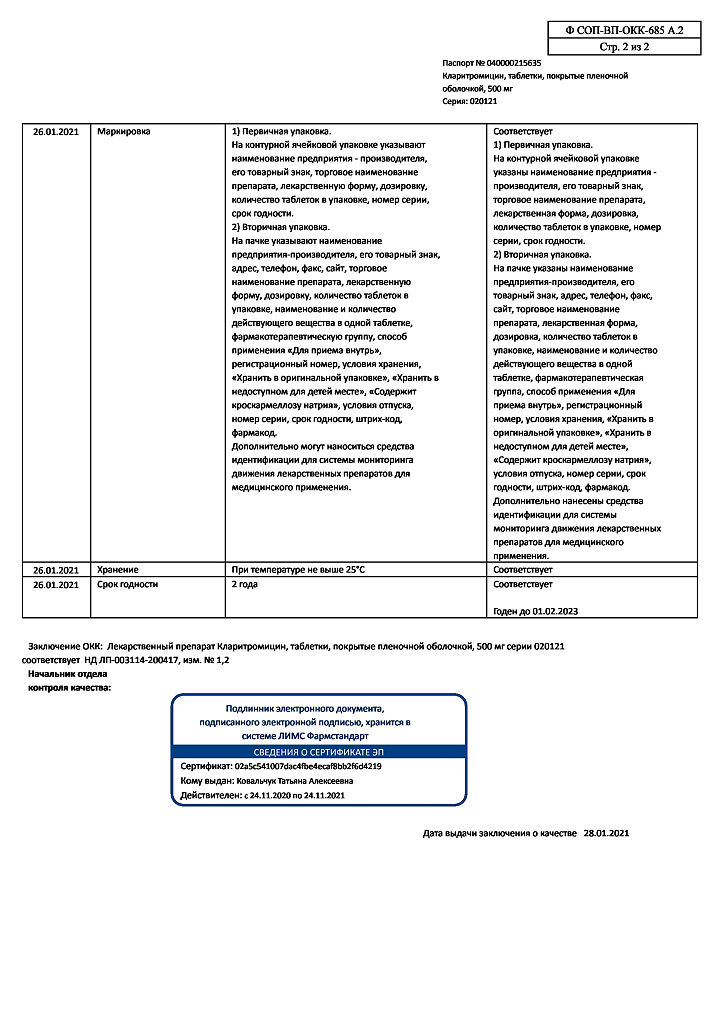
Clarithromycin, 500 mg 14 pcs
€15.12 €12.60
Description
Pharmacotherapeutic group:
Macrolide antibiotic
ATC code: J01FA09
Pharmacological properties
Pharmacodynamics
The semisynthetic antibiotic of the macrolide group. It has antibacterial action, interacting with 50S ribosomal subunit of bacteria and inhibiting protein synthesis in the microbial cell. It acts on extra- and intracellularly located pathogens.
Clarithromycin has demonstrated high in vitro activity against standard and isolated cultures of bacteria. It is highly effective against many aerobic and anaerobic gram-positive and gram-negative microorganisms. In vitro studies confirm high effectiveness of clarithromycin against Legionella pneumophila, Mycoplasma pneumoniae and Helicobacter pylori.
The activity of clarithromycin against most strains of the following microorganisms has been proven in in vitro studies and in clinical practice:
Aerobic Gram-positive microorganisms: Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus pyogenes, Listeria monocytogenes;
aerobic gram-negative microorganisms: Haemophilus influenzae, Haemophilus parainfluenzae, Moraxella catarrhalis, Neisseria gonorrheae, Legionella pneumophila;
other microorganisms: Mycoplasma pneumoniae, Chlamydia pneumoniae (TWAR); Mycobacteria: Mycobacterium leprae, Mycobacterium chelonae, Mycobacterium kansasii, Mycobacterium fortuitum, Mycobacterium avium complex (MAC): Mycobacterium avium, Mycobacterium intracellulare;
Helicobacter pylori.
The Enterobacteriaceae, Pseudomonas spp. and other non-lactose degrading Gram-negative bacteria are insensitive to clarithromycin.
The production of β-lactamase has no effect on clarithromycin activity. Most staphylococcal strains resistant to methicillin and oxacillin are also resistant to clarithromycin.
Clarithromycin is also effective in vitro against most strains of the microorganisms listed below:
Aerobic Gram-positive microorganisms: Streptococcus agalactiae, Streptococcus spp. (groups C, F, G), Streptococcus spp. Viridans group;
aerobic gram-negative microorganisms: Bordetella pertussis, Pasteurella multocida;
anaerobic gram-positive microorganisms: Clostridium perfringens, Peptococcus niger, Propionibacterium acnes;
anaerobic gram-negative microorganisms: Bacteroides melaninogenicus;
Spirochaetes: Borrelia burgdorferi, Treponema pallidum;
Campylobacter: Campylobacter jejuni.
The main metabolite of clarithromycin in humans is the microbiologically active metabolite 14-hydroxyclarithromycin. The microbiological activity of the metabolite is the same as that of the parent substance, or 1-2 times weaker against most microorganisms. The exception is Naemophilus influenzae, against which the effectiveness of the metabolite is 2 times higher. The starting substance and its main metabolite have either additive or synergistic effect against Naemophilus influenzae under in vitro and in vivo conditions depending on the bacterial culture.
Pharmacokinetics
Absorption and distribution
On oral administration, clarithromycin is rapidly and actively absorbed in the gastrointestinal tract. Absolute bioavailability is 50%. No cumulation is found when multiple doses of the drug are administered, and the metabolic pattern in the human body does not change. Food slows down absorption; taking food immediately before taking the drug increases bioavailability by 25% on average. Maximum equilibrium concentrations (Cmax) of clarithromycin and 14-hydroxyclarithromycin were achieved after the fifth dose at a dose of 500 mg twice daily, averaging 2.7-2.9 µg/ml and 0.83-0.88 µg/ml, respectively.
Clarithromycin binds to plasma proteins by 70% at concentrations ranging from 0.45 µg/ml to 4.5 µg/ml. At a concentration of 45 µg/ml, the degree of binding decreases to 41%, probably as a result of saturation of the binding sites. This is observed only at concentrations many times higher than the therapeutic concentration.
Clarithromycin and 14-hydroxyclarithromycin are well distributed to all tissues and body fluids. After oral administration of clarithromycin, its content in cerebrospinal fluid remains low (with normal GEB permeability
1-2% of serum levels). Its content in tissues is usually several times its content in serum.
Metabolism and excretion
Clarithromycin is metabolized in cytochrome P450 system with participation of CYP3A4, CYP3A5, CYP3A7 isoenzymes to form the main microbiologically active metabolite 14-hydroxyclarithromycin. When multiple doses of the drug are administered, the nature of metabolism in the human body does not change.
At equilibrium concentrations of 14-hydroxyclarithromycin do not increase in proportion to clarithromycin doses, and the elimination half-lives (T1/2) of clarithromycin and its main metabolite increase with increasing doses. The nonlinear nature of clarithromycin pharmacokinetics is associated with decreased formation of 14-hydroxylated and N-demethylated metabolites at higher doses, indicating nonlinearity of clarithromycin metabolism when taken at high doses.
The T1/2 of clarithromycin and 14-hydroxyclarithromycin are 4.5-4.8 hours and 6.9-8.7 hours, respectively, when taken at a dose of 500 mg twice daily.
Extracted by the kidneys and intestines (20-30% unchanged, the rest as metabolites). In a single dose of 250 mg and 1200 mg is excreted by the kidneys 37.9 % and 46 %, the intestines 40.2 % and 29.1 %, respectively.
Pharmacokinetics in special clinical cases
Hepatic disorders
. No clarithromycin dose adjustment is required in patients with moderate to severe hepatic impairment but with preserved renal function; equilibrium concentrations (Csas) and systemic clearance of clarithromycin do not differ from these in healthy patients. The Cs of 14-hydroxyclarithromycin is lower in people with hepatic impairment than in healthy subjects.
Kidney disease
In patients with impaired renal function, plasma Cmax and Cmin, T1/2, area under the concentration-time curve (AUC) of clarithromycin and 14-hydroxyclarithromycin are increased. The elimination constant and renal excretion decreases. The degree of change in these parameters depends on the degree of renal impairment.
Elderly patients
In elderly patients, blood concentrations of clarithromycin and 14-hydroxyclarithromycin were higher and excretion slower than in younger adults. Changes in pharmacokinetics in elderly patients are thought to be primarily related to changes in creatinine clearance and renal functional status rather than to patient age.
HIV infection
The Cs of clarithromycin and 14-hydroxyclarithromycin in patients with HIV infection who received clarithromycin in usual doses (500 mg twice daily) were similar to those in healthy subjects. However, when clarithromycin is used and at higher doses that may be required for the treatment of mycobacterial infections, concentrations of the antibiotic may be significantly higher than usual. In HIV-infected patients who received clarithromycin at a dose of 1 g per day and 2 g per day in 2 doses, Cmax was typically 2-4 mcg/ml and 5-10 mcg/ml, respectively. When using the drug in higher doses, a prolongation of the T1/2 was observed compared to that in healthy subjects receiving clarithromycin in usual doses. The increased plasma concentrations and longer half-life when using clarithromycin at higher doses are consistent with the known non-linearity of the drug’s pharmacokinetics.
Indications
Indications
Infectious and inflammatory diseases caused by organisms sensitive to clarithromycin:
– upper respiratory tract infections (such as pharyngitis, sinusitis);
– lower respiratory tract infections (such as bronchitis, pneumonia);
– uncomplicated infections of the skin and soft tissues (such as folliculitis, inflammation of the subcutaneous tissue, erysipelas);
– disseminated and localized mycobacterial infections caused by Mycobacterium avium and Mycobacterium intracellulare. Localized infections caused by Mycobacterium chelonae, Mycobacterium fortuitum and Mycobacterium kansasii;
– prevention of the spread of infection caused by the Mycobacterium avium complex (MAC) in HIV-infected patients with a CD4 lymphocyte count (T-helper lymphocyte) of no more than 100/mm3;
– to eradicate Helicobacter pylori and reduce the frequency of relapses of duodenal ulcers.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group:
macrolide antibiotic
ATX code: J01FA09
Pharmacological properties
Pharmacodynamics
Semi-synthetic antibiotic of the macrolide group. It has an antibacterial effect by interacting with the 50S ribosomal subunit of bacteria and inhibiting protein synthesis in the microbial cell. Acts on extra- and intracellularly located pathogens.
Clarithromycin has demonstrated high in vitro activity against standard and isolated bacterial cultures. Highly effective against many aerobic and anaerobic gram-positive and gram-negative microorganisms. In vitro studies confirm the high effectiveness of clarithromycin against Legionella pneumophila, Mycoplasma pneumoniae and Helicobacter pylori.
The activity of clarithromycin against most strains of the following microorganisms has been proven in in vitro studies and in clinical practice:
aerobic gram-positive microorganisms: Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus pyogenes, Listeria monocytogenes;
aerobic gram-negative microorganisms: Haemophilus influenzae, Haemophilus parainfluenzae, Moraxella catarrhalis, Neisseria gonorrheae, Legionella pneumophila;
other microorganisms: Mycoplasma pneumoniae, Chlamydia pneumoniae (TWAR); mycobacteria: Mycobacterium leprae, Mycobacterium chelonae, Mycobacterium kansasii, Mycobacterium fortuitum, Mycobacterium avium complex (MAC): Mycobacterium avium, Mycobacterium intracellulare;
Helicobacter pylori.
Enterobacteriaceae, Pseudomonas spp., as well as other gram-negative bacteria that do not degrade lactose are insensitive to clarithromycin.
The production of β-lactamase does not affect the activity of clarithromycin. Most strains of staphylococci resistant to methicillin and oxacillin are also resistant to clarithromycin.
Clarithromycin is effective in vitro against most strains of the following microorganisms:
aerobic gram-positive microorganisms: Streptococcus agalactiae, Streptococcus spp. (groups C, F, G), Streptococcus spp. Viridans groups;
aerobic gram-negative microorganisms: Bordetella pertussis, Pasteurella multocida;
anaerobic gram-positive microorganisms: Clostridium perfringens, Peptococcus niger, Propionibacterium acnes;
anaerobic gram-negative microorganisms: Bacteroides melaninogenicus;
spirochetes: Borrelia burgdorferi, Treponema pallidum;
Campylobacter: Campylobacter jejuni.
The main metabolite of clarithromycin in the human body is the microbiologically active metabolite 14-hydroxyclarithromycin. The microbiological activity of the metabolite is the same as that of the parent substance, or 1-2 times weaker against most microorganisms. The exception is Haemophilus influenzae, for which the effectiveness of the metabolite is 2 times higher. The parent substance and its main metabolite have either an additive or synergistic effect against Haemophilus influenzae in vitro and in vivo, depending on the bacterial culture.
Pharmacokinetics
Suction and distribution
When taken orally, clarithromycin is rapidly and actively absorbed from the gastrointestinal tract. Absolute bioavailability is 50%. With repeated doses of the drug, no accumulation was detected, and the nature of metabolism in the human body does not change. Food slows down absorption; eating immediately before taking the drug increases bioavailability by an average of 25%. When taking the drug at a dose of 500 mg 2 times a day, the maximum equilibrium concentrations (Cmax) of clarithromycin and 14-hydroxyclarithromycin were achieved after taking the fifth dose and averaged 2.7-2.9 mcg/ml and 0.83-0.88 mcg/ml, respectively.
Clarithromycin is 70% bound to plasma proteins at concentrations ranging from 0.45 mcg/ml to 4.5 mcg/ml. At a concentration of 45 μg/ml, the degree of binding decreases to 41%, probably as a result of saturation of binding sites. This is observed only at concentrations many times higher than the therapeutic value.
Clarithromycin and 14-hydroxyclarithromycin are well distributed into all tissues and fluids of the body. After oral administration of clarithromycin, its content in the cerebrospinal fluid remains low (with normal BBB permeability
1-2% of the serum level). The content in tissues is usually several times higher than its content in blood serum.
Metabolism and excretion
Clarithromycin is metabolized in the cytochrome P450 system with the participation of isoenzymes CYP3A4, CYP3A5, CYP3A7 with the formation of the main microbiologically active metabolite 14-hydroxyclarithromycin. With repeated doses of the drug, the nature of metabolism in the human body does not change.
At steady state, the concentration of 14-hydroxyclarithromycin does not increase in proportion to clarithromycin doses, and the half-lives (T1/2) of clarithromycin and its main metabolite increase with increasing dose. The non-linear nature of the pharmacokinetics of clarithromycin is associated with a decrease in the formation of 14-hydroxylated and N-demethylated metabolites at higher doses, indicating non-linearity in the metabolism of clarithromycin when taken in high doses.
When taken at a dose of 500 mg 2 times a day, T1/2 of clarithromycin and 14-hydroxyclarithromycin are 4.5-4.8 hours and 6.9-8.7 hours, respectively.
It is excreted by the kidneys and intestines (20-30% in unchanged form, the rest in the form of metabolites). With a single dose of 250 mg and 1200 mg, 37.9% and 46% are excreted by the kidneys, 40.2% and 29.1%, respectively, by the intestines.
Pharmacokinetics in special clinical situations
Liver diseases
In patients with moderate to severe liver dysfunction, but with preserved renal function, no dose adjustment of clarithromycin is required; steady-state concentrations (Css) and systemic clearance of clarithromycin do not differ from those in healthy patients. Css of 14-hydroxyclarithromycin in people with impaired liver function is lower than in healthy people.
Kidney diseases
In patients with impaired renal function, Cmax and Cmin in blood plasma, T1/2, and the area under the concentration-time curve (AUC) of clarithromycin and 14-hydroxyclarithromycin increase. The elimination constant and renal excretion decrease. The degree of changes in these parameters depends on the degree of renal dysfunction.
Elderly patients
In elderly patients, the concentration of clarithromycin and 14-hydroxyclarithromycin in the blood was higher, and elimination was slower than in young people. It is believed that changes in pharmacokinetics in elderly patients are associated primarily with changes in creatinine clearance and renal function, and not with the age of the patients.
HIV infection
Css of clarithromycin and 14-hydroxyclarithromycin in patients with HIV infection who received clarithromycin in usual doses (500 mg 2 times a day) were similar to those in healthy people. However, when clarithromycin is used and at higher doses, which may be required to treat mycobacterial infections, antibiotic concentrations may be significantly higher than usual. In patients with HIV infection taking clarithromycin at a dose of 1 g per day and 2 g per day in 2 divided doses, Cmax was usually 2-4 mcg/ml and 5-10 mcg/ml, respectively. When using the drug in higher doses, a prolongation of T1/2 was observed compared with that in healthy people receiving clarithromycin in usual doses. The increase in plasma concentrations and half-life when clarithromycin is administered at higher doses is consistent with the known nonlinearity of the drug’s pharmacokinetics.
Special instructions
Special instructions
Long-term use of antibiotics can lead to the formation of colonies with an increased number of insensitive bacteria and fungi. In case of superinfection, appropriate therapy must be prescribed.
Cases of liver dysfunction (increased concentrations of liver enzymes in the blood, hepatocellular and/or cholestatic hepatitis with or without jaundice) have been reported with the use of clarithromycin. Liver dysfunction can be severe but is usually reversible. There have been cases of fatal liver failure, mainly associated with the presence of serious concomitant diseases and/or concomitant use of other drugs. If signs and symptoms of hepatitis appear, such as anorexia, jaundice, dark urine, itching, abdominal tenderness on palpation, clarithromycin therapy should be stopped immediately.
In the presence of chronic liver diseases, it is necessary to regularly monitor serum enzymes.
When treated with almost all antibacterial agents, including clarithromycin, cases of pseudomembranous colitis have been described, the severity of which can range from mild to life-threatening. Antibacterial drugs can change the normal intestinal microflora, which can lead to the growth of Clostridium difficile. Pseudomembranous colitis caused by Clostridium difficile should be suspected in all patients who experience diarrhea after using antibacterial agents. After a course of antibiotic therapy, careful medical monitoring of the patient is necessary. Cases of the development of pseudomembranous colitis 2 months after taking antibiotics have been described.
Clarithromycin should be used with caution in patients with coronary heart disease, severe heart failure, hypomagnesemia, severe bradycardia (less than 50 beats/min), as well as when used simultaneously with class IA (quinidine, procainamide) and class III antiarrhythmic drugs (dofetilide, amiodarone, sotalol). In these conditions and when taking the drug simultaneously with these drugs, ECG should be regularly monitored for an increase in the QT interval.
It is possible to develop cross-resistance to clarithromycin and other macrolide antibiotics, as well as lincomycin and clindamycin.
Given the increasing resistance of Streptococcus pneumoniae to macrolides, it is important to perform susceptibility testing when prescribing clarithromycin to patients with community-acquired pneumonia. For hospital-acquired pneumonia, clarithromycin should be used in combination with appropriate antibiotics.
Mild to moderate skin and soft tissue infections are most often caused by Staphylococcus aureus and Streptococcus pyogenes. Moreover, both pathogens can be resistant to macrolides. Therefore, it is important to conduct a sensitivity test.
Macrolides can be used for infections caused by Corynebacterium minutissimum (erythrasma), acne vulgaris and erysipelas, as well as in situations where penicillin cannot be used.
If acute hypersensitivity reactions occur, such as anaphylactic reaction, Stevens-Johnson syndrome, toxic epidermal necrolysis, drug rash with eosinophilia and systemic symptoms (DRESS syndrome), you should immediately stop taking clarithromycin and begin appropriate therapy.
In case of combined use with warfarin or other indirect anticoagulants, it is necessary to monitor MHO and prothrombin time.
Impact on the ability to drive vehicles and machinery
Caution should be exercised when driving and engaging in other potentially hazardous activities, as some side effects of clarithromycin, such as dizziness, drowsiness, may adversely affect the ability to drive and perform potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Clarithromycin
Composition
Composition
Composition per tablet:
Active substance:
clarithromycin ̶ 500.00 mg.
Excipients:
croscarmellose sodium ‒ 42.50 mg,
microcrystalline cellulose ‒ 222.50 mg,
colloidal silicon dioxide ‒ 25.50 mg,
pregelatinized starch – 34.00 mg,
stearic acid ̶ 8.50 mg,
sodium stearyl fumarate – 17.00 mg.
Shell
VIVACOAT® PA-2P-097 [hypromellose (hydroxypropyl methylcellulose 6 cP) – 18.330 mg, titanium dioxide – 15.068 mg, polydextrose (E1200) – 7.050 mg, talc – 3.290 mg, macrogol – 3350 (polyethylene glycol – 3350) – 2.820 mg, quinoline yellow dye (E104) – 0.423 mg, iron oxide yellow dye (E172) – 0.019 mg] – 47.000 mg.
Contraindications
Contraindications
– hypersensitivity to clarithromycin and other components of the drug, as well as hypersensitivity to other macrolide antibiotics;
– simultaneous use of astemizole, cisapride, pimozide, terfenadine, ergotamine, dihydroergotamine, midazolam for oral use (see “Interaction with other drugs”);
– simultaneous use of clarithromycin with HMG-CoA reductase inhibitors (statins), which are largely metabolized by the CYP3A4 isoenzyme (lovastatin, simvastatin), due to an increased risk of myopathy, including rhabdomyolysis;
– simultaneous administration of colchicine;
– renal failure (creatinine clearance less than 30 ml/min);
– simultaneous use with ticagrelor or ranolazine;
– history of QT prolongation, ventricular arrhythmia or ventricular tachycardia of the “torsade de pointes” type;
– severe liver failure occurring simultaneously with renal failure;
– cholestatic jaundice/hepatitis resulting from the use of clarithromycin
(in history);
– porphyria;
– hypokalemia (risk of QT interval prolongation);
– lactation period (breastfeeding);
– children under 12 years of age (efficacy and safety have not been established).
With caution
– pregnancy;
– moderate to severe liver failure;
– coronary heart disease, severe heart failure, severe bradycardia (less than 50 beats/min);
– simultaneous use with benzodiazepines, such as alprazolam, triazolam, midazolam for intravenous use;
– simultaneous use with drugs that are metabolized by the CYP3A isoenzyme, for example, carbamazepine, cilostazol, cyclosporine, disopyramide, methylprednisolone, omeprazole, indirect anticoagulants (for example: warfarin), quinidine, rifabutin, sildenafil, tacrolimus, vinblastine;
– simultaneous use with drugs that induce the CYP3A4 isoenzyme, for example, rifampicin, phenytoin, carbamazepine, phenobarbital, St. John’s wort;
– simultaneous use with blockers of “slow” calcium channels that are metabolized by the CYP3A4 isoenzyme (for example: verapamil, amlodipine, diltiazem);
– simultaneous use of class IA (quinidine, procainamide) and class III antiarrhythmic drugs (dofetilide, amiodarone, sotalol);
– simultaneous use of clarithromycin with other ototoxic drugs, especially aminoglycosides;
– simultaneous use of clarithromycin with statins that do not depend on the metabolism of the CYP3A4 isoenzyme (for example, fluvastatin) (see section “Interaction with other drugs”);
– hypomagnesemia.
Side Effects
Side Effects
Side effects are presented depending on the effect on organs and organ systems.
The following adverse events noted with the use of clarithromycin are distributed according to the frequency of occurrence according to the following gradation: very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1000 to < 1/100), rare (≥ 1/10000 to < 1/1000), very rare (< 1/10000), unspecified frequency (cannot be calculated from available data).
Infectious and parasitic diseases: uncommon – candidiasis of the oral mucosa. As with the use of other antibacterial drugs, secondary infections (development of resistance of microorganisms) are also possible.
From the blood and lymphatic system: rarely – leukopenia, eosinophilia, neutropenia, thrombocytopenia; unspecified frequency – agranulocytosis, hemorrhages.
From the immune system: often – rash; uncommon – allergic reactions (urticaria, itching), anaphylactic/anaphylactoid reactions; unspecified frequency – Stevens-Johnson syndrome, toxic epidermal necrolysis – Lyell’s syndrome (potentially life-threatening), drug rash with eosinophilia and systemic symptoms (DRESS syndrome); angioedema.
Mental disorders: often – insomnia; infrequently – drowsiness; unspecified frequency – confusion, depersonalization, depression, disorientation, hallucinations, psychotic disorders, nightmares, mania.
From the nervous system: often – headache, change in taste (dysgeusia); uncommon – dizziness, paresthesia, tremor, asthenia, anxiety; rarely – anosmia; unspecified frequency – convulsions.
From the senses: often – ageusia (loss of taste); uncommon – vertigo, tinnitus; rarely – hearing loss that goes away after discontinuation of the drug; unspecified frequency – parosmia.
From the cardiovascular system: infrequently – prolongation of the QT interval on the ECG (as with other macrolides); rarely – ventricular tachycardia, including the “torsade de pointes” type, flutter and fibrillation of the atria and ventricles.
From the gastrointestinal tract: often – diarrhea, nausea, abdominal pain, dyspepsia; uncommon – vomiting, glossitis, stomatitis, bloating, pseudomembranous colitis, anorexia, loss of appetite, constipation, belching, flatulence, dry oral mucosa, gastritis; unspecified frequency – acute pancreatitis, discoloration of teeth and tongue.
From the liver and biliary tract: infrequently – hepatocellular and cholestatic hepatitis, cholestasis, cholestatic jaundice; very rarely – in isolated cases, deaths from liver failure were recorded, which were usually observed in the presence of serious concomitant diseases and/or simultaneous use of other drugs.
From the skin and subcutaneous tissues: often – hyperhidrosis; rarely – erysipelas, unspecified frequency – acne.
From the musculoskeletal system and connective tissue: infrequently – myalgia, arthralgia; unspecified frequency – myopathy.
From the kidneys and urinary tract: rarely – interstitial nephritis; unspecified frequency – renal failure.
Laboratory indicators: often – increased activity of liver enzymes; uncommon – increased creatinine concentration, hypoglycemia (including with simultaneous use of hypoglycemic drugs), increased alkaline phosphatase activity, increased bilirubin; unspecified frequency – increased international normalized ratio (INR), prolongation of prothrombin time, change in urine color.
General disorders: uncommon – malaise, chest pain, chills, fatigue.
Immunosuppressed patients
In patients with AIDS and other immunodeficiencies receiving clarithromycin in higher doses over a long period of time for the treatment of mycobacterial infections, it is often difficult to distinguish adverse effects of the drug from symptoms of HIV infection or concomitant disease.
The most common adverse events in patients taking a daily dose of clarithromycin of 1000 mg were: nausea, vomiting, taste disturbance, abdominal pain, diarrhea, rash, flatulence, headache, constipation, hearing loss, increased concentrations of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) in the blood. Low incidence adverse events such as shortness of breath, insomnia and dry mouth were also reported.
In patients with suppressed immunity, laboratory parameters were assessed, analyzing their significant deviations from the norm (sharp increase or decrease). Based on this criterion, 2-3% of patients receiving clarithromycin at a dose of 1000 mg daily had a significant increase in the concentration of ALT and AST in the blood, as well as a decrease in the number of leukocytes and platelets. Increases in residual urea nitrogen concentrations have also been reported in a small number of patients.
Interaction
Interaction
Concomitant use with drugs such as astemizole, cisapride, pimozide, terfenadine, ergotamine, dihydroergotamine, midazolam (oral dosage forms), simvastatin, lovastatin is contraindicated due to the possibility of developing serious side effects (see “Contraindications”).
Cisapride and pimozide
When used together, the following are possible: an increase in the concentration of cisapride, an increase in the QT interval, the appearance of cardiac arrhythmias, including ventricular tachycardia, including pirouette type, ventricular fibrillation.
Terfenadine and astemizole
When used together, the following are possible: an increase in the concentration of terfenadine/astemizole in the blood, the occurrence of cardiac arrhythmias, an increase in the QT interval, ventricular tachycardia, ventricular fibrillation and torsade de pointes.
Ergotamine/dihydroergotamine
When used together, the following effects associated with acute poisoning with drugs of the ergotamine group are possible: vascular spasm, ischemia of the limbs and other tissues, including the central nervous system.
Effect of other drugs on clarithromycin
Drugs that are inducers of the CYP3A isoenzyme (for example: rifampicin, phenytoin, carbamazepine, phenobarbital, St. John’s wort) can induce the metabolism of clarithromycin. This may result in subtherapeutic concentrations of clarithromycin, resulting in reduced effectiveness. In addition, it is necessary to monitor the concentration of the CYP3A inducer in the blood plasma, which may increase due to inhibition of the CYP3A inducer by clarithromycin. When rifabutin and clarithromycin were used together, an increase in plasma concentration and a decrease in serum concentration of clarithromycin was observed with an increased risk of developing uveitis.
The following drugs have a proven or suspected effect on clarithromycin plasma concentrations; if used concomitantly with clarithromycin, dosage adjustments or switching to alternative treatment may be required.
Efavirenz, nevirapine, rifampicin, rifabutin and rifapentine
Strong inducers of the cytochrome P450 system, such as efavirenz, nevirapine, rifampicin, rifabutin and rifapentine, can accelerate the metabolism of clarithromycin and, thus, reduce the plasma concentration of clarithromycin and weaken its therapeutic effect, and at the same time increase the concentration
14-OH-clarithromycin is a metabolite that is also microbiologically active. Since the microbiological activity of clarithromycin and 14-OH-clarithromycin differs against different bacteria, the therapeutic effect may be reduced when clarithromycin is used together with inducers of cytochrome P450 isoenzymes.
Etravirine
The concentration of clarithromycin decreases with the use of etravirine, but the concentration of the active metabolite 14-OH-clarithromycin increases. Since
14-OH-clarithromycin has low activity against Mycobacterium avium complex (MAC) infections and overall activity against Mycobacterium avium complex (MAC) infections may be altered, so alternative treatments should be considered for the treatment of MAC.
Fluconazole
Coadministration of fluconazole 200 mg daily and clarithromycin 500 mg twice daily in 21 adult volunteers resulted in an increase in clarithromycin trough mean steady-state concentration (Css) and AUC by 33% and 18%, respectively. However, co-administration did not significantly affect the average steady-state concentration of the active metabolite 14-OH-clarithromycin. No dose adjustment of clarithromycin is required when taking fluconazole concomitantly.
Ritonavir
When taking ritonavir 600 mg per day and clarithromycin 1 g per day together, the metabolism of clarithromycin may decrease (increase in Cmax by 31%, Cmin by
182% and AUC by 77%), complete inhibition of the formation of 14-hydroxyclarithromycin. Due to the wide therapeutic index, dosage reduction is not required in patients with normal renal function. In patients with renal failure, it is advisable to consider the following dose adjustment options: with a creatinine clearance of 30-60 ml/min, the dose of clarithromycin should be reduced by 50%; with a creatinine clearance of less than 30 ml/min, the dose of clarithromycin should be reduced by 75%. Ritonavir should not be co-administered with clarithromycin in doses exceeding 1 g per day.
Oral hypoglycemic agents / Insulin
Concomitant use of clarithromycin and oral hypoglycemic drugs and/or insulin can lead to severe hypoglycemia. When clarithromycin is used concomitantly with certain oral hypoglycemic drugs, such as nateglinide, pioglitazone, repaglinide, rosiglitazone, hypoglycemia may occur due to inhibition of the CYP3A isoenzyme by clarithromycin. Close monitoring of blood glucose concentrations is recommended.
Effect of clarithromycin on other drugs
Antiarrhythmic drugs (quinidine and disopyramide)
When used together with quinidine or disopyramide, ventricular tachycardia of the “pirouette” type may occur. When clarithromycin is coadministered with these drugs, the electrocardiogram should be regularly monitored for prolongation of the QT interval, and serum concentrations of these drugs should also be monitored. During post-targeting use, cases of hypoglycemia have been reported when clarithromycin and disopyramide were taken together. It is necessary to monitor blood glucose concentrations when using clarithromycin and disopyramide simultaneously.
Interactions due to CYP3A4
Co-administration of clarithromycin, which is known to inhibit the CYP3A enzyme, and drugs primarily metabolized by the CYP3A isoenzyme, may be associated with a mutual increase in their concentrations, which may increase or prolong both therapeutic and side effects. Clarithromycin should be used with caution in patients receiving drugs that are substrates of the CYP3A isoenzyme, especially if these drugs have a narrow therapeutic index (for example: carbamazepine), and/or are extensively metabolized by this enzyme. If necessary, the dose of the drug taken together with clarithromycin should be adjusted. Also, whenever possible, serum concentrations of drugs primarily metabolized by the CYP3A isoenzyme should be monitored.
The following drugs/classes are metabolized by the same CYP3A isoenzyme as clarithromycin, for example, alprazolam, carbamazepine, cilostazol, cyclosporine, disopyramide, methylprednisolone, midazolam, omeprazole, indirect anticoagulants (eg warfarin), quinidine, rifabutin, sildenafil, tacrolimus, triazolam and vinblastine. Also, CYP3A agonists include the following drugs that are contraindicated for combined use with clarithromycin: astemizole, cisapride, pimozide, terfenadine, lovastatin, simvastatin and ergot alkaloids (see section “Contraindications”). Drugs that interact in this manner through other isoenzymes within the cytochrome P450 system include phenytoin, theophylline, and valproic acid.
HMG-CoA reductase inhibitors (statins)
Co-administration of clarithromycin with lovastatin or simvastatin is contraindicated (see section “Contraindications”) due to the fact that these statins are largely metabolized by the CYP3A4 isoenzyme, and combined use with clarithromycin increases their serum concentrations, which leads to an increased risk of myopathy, including rhabdomyolysis. Rare cases of rhabdomyolysis have been reported in patients taking these drugs together. If clarithromycin is necessary, lovastatin or simvastatin should be discontinued during therapy.
Clarithromycin should be used with caution in combination therapy with statins. If coadministration is necessary, it is recommended to take the lowest dose of statin. It is necessary to use statins that do not depend on the metabolism of the CYP3A isoenzyme (for example: fluvastatin). The development of signs and symptoms of myopathy should be monitored.
Oral anticoagulants
There is a risk of serious bleeding and a significant increase in prothrombin time when clarithromycin and warfarin are used simultaneously. If patients are receiving clarithromycin and oral anticoagulants concomitantly, prothrombin time and INR should be carefully monitored.
Omeprazole
When clarithromycin and omeprazole are used together, it is possible to increase the equilibrium plasma concentrations of omeprazole (Cmax, AUC0-24, T1/2 by 30%, 89%, and
34% respectively).
Sildenafil, tadalafil and vardenafil
Each of these phosphodiesterase inhibitors is metabolized, at least in part, by CYP3A. At the same time, the CYP3A isoenzyme can be inhibited in the presence of clarithromycin. Co-administration of clarithromycin with sildenafil, tadalafil or vardenafil may lead to increased phosphodiesterase inhibitory effects. When prescribing these drugs together, consider reducing the dose of sildenafil, tadalafil and vardenafil.
Theophylline, carbamazepine
It is possible to increase the concentration of theophylline or carbamazepine in the systemic circulation.
Tolterodine
The primary metabolism of tolterodine occurs through the 2D6 isoform of cytochrome P450 (CYP2D6). However, in part of the population lacking the CYP2D6 isoenzyme, metabolism occurs through CYP3A. In this population, inhibition of CYP3A results in significantly higher serum tolterodine concentrations. In populations that are poor metabolizers of CYP2D6, a dose reduction of tolterodine may be required in the presence of CYP3A inhibitors such as clarithromycin.
Benzodiazepines (eg: alprazolam, midazolam, triazolam)
When co-administered with clarithromycin (500 mg 2 times a day), the AUC of midazolam may increase: 7 times after oral administration and 2.7 times after intravenous administration. Concomitant oral administration of midazolam and clarithromycin should be avoided. If intravenous midazolam is used concomitantly with clarithromycin, the patient’s condition should be carefully monitored for possible dose adjustment. The same precautions should be applied to other benzodiazepines that are metabolized by CYP3A, including triazolam and alprazolam. For benzodiazepines whose elimination is not dependent on CYP3A (temazepam, nitrazepam, lorazepam), a clinically significant interaction with clarithromycin is unlikely.
When clarithromycin and triazolam are used together, central nervous system (CNS) effects such as drowsiness and confusion are possible.
Therefore, if coadministration occurs, it is recommended to monitor for symptoms of CNS impairment.
Interaction with other drugs
Aminoglycosides
When taking clarithromycin concomitantly with other ototoxic drugs, especially aminoglycosides, caution should be exercised and the functions of the vestibular and auditory systems should be monitored, both during and after therapy.
Colchicine
Colchicine is a substrate of both CYP3A and the drug efflux transport protein P-glycoprotein (Pgp). Clarithromycin and other macrolides are known to inhibit CYP3A and Pgp. When clarithromycin and colchicine are taken together, inhibition of Pgp and/or CYP3A may result in increased effects of colchicine.
The simultaneous use of clarithromycin and colchicine is contraindicated (see section “Contraindications”).
Digoxin
Digoxin is suspected to be a Pgp substrate. Clarithromycin is known to inhibit Pgp. When digoxin and clarithromycin are co-administered, inhibition of Pgp by clarithromycin may result in increased effects of digoxin. Coadministration of digoxin and clarithromycin may also result in increased serum concentrations of digoxin. Some patients experienced significant clinical symptoms of digoxin toxicity, including potentially fatal arrhythmias. When clarithromycin and digoxin are taken together, it is necessary to carefully monitor the concentration of digoxin in the blood serum.
Zidovudine
Concomitant oral administration of clarithromycin and zidovudine in adults
In HIV-infected patients, the steady-state concentration of zidovudine may decrease.
Because clarithromycin interferes with the oral absorption of zidovudine, the interaction can be largely avoided by taking clarithromycin and zidovudine 4 hours apart.
This type of interaction does not occur in HIV-infected children receiving clarithromycin suspension with zidovudine or dideoxyinosine. Since clarithromycin may interfere with the absorption of zidovudine when administered concomitantly orally in adult patients, such an interaction is unlikely to occur when clarithromycin is used intravenously.
Phenytoin and valproic acid
There is evidence of interactions between CYP3A inhibitors (including clarithromycin) and drugs that are not metabolized by CYP3A (phenytoin and valproic acid). For these drugs, when used together with clarithromycin, it is recommended to determine their serum concentrations, as there are reports of their increase.
Bidirectional drug interactions
Atazanavir
Clarithromycin and atazanavir are both substrates and inhibitors of CYP3A. There is evidence of a bidirectional interaction between these drugs. Coadministration of clarithromycin (500 mg twice daily) and atazanavir (400 mg once daily daily) may result in a twofold increase in clarithromycin exposure and a 70% decrease in 14-OH-clarithromycin levels, with a 28% increase in atazanavir AUC. Due to the wide therapeutic range of clarithromycin, dose reduction is not required in patients with normal renal function.
In patients with moderate renal impairment (creatinine clearance
30-60 ml/min) the dose of clarithromycin should be reduced by 50%. In patients with creatinine clearance less than 30 ml/min, the dose of clarithromycin should be reduced by 75%. Clarithromycin in doses exceeding 1000 mg per day should not be used in conjunction with protease inhibitors.
Blockers of “slow” calcium channels
When using clarithromycin simultaneously with blockers of “slow” calcium channels that are metabolized by the CYP3A4 isoenzyme (for example: verapamil, amlodipine, diltiazem), caution should be exercised as there is a risk of arterial hypotension. Plasma concentrations of clarithromycin, as well as slow calcium channel blockers, may increase with simultaneous use. Hypotension, bradyarthymia and lactic acidosis are possible when taking clarithromycin and verapamil simultaneously.
When taken together with clarithromycin, a decrease in blood pressure, bradyarrhythmia and lactic acidosis is possible.
Itraconazole
Clarithromycin and itraconazole are substrates and inhibitors of the CYP3A isoenzyme, which determines the bidirectional interaction of the drugs. Clarithromycin may increase plasma concentrations of itraconazole, while itraconazole may increase plasma concentrations of clarithromycin. Patients taking itraconazole and clarithromycin concomitantly should be closely monitored for symptoms of increased or prolonged pharmacological effects of these drugs.
Saquinavir
Clarithromycin and saquinavir are substrates and inhibitors of the CYP3A isoenzyme, which determines the bidirectional interaction of the drugs. With simultaneous use of clarithromycin (500 mg 2 times a day) and saquinavir
(soft gelatin capsules, 1200 mg 3 times daily) may increase AUC and
Css of saquinavir by 177% and 187%, and clarithromycin by 40%. When these two drugs are used together for a limited time and in the doses/formulations indicated above, no dose adjustment is required. The results of drug interaction studies with saquinavir monotherapy may not be consistent with the effects observed with saquinavir/ritonavir therapy. When taking saquinavir with ritonavir, the potential effect of ritonavir on clarithromycin should be considered.
Overdose
Overdose
Symptoms: Taking a large dose of clarithromycin may cause nausea, vomiting, abdominal pain, diarrhea, headache, and confusion.
Treatment: gastric lavage, symptomatic therapy. Hemodialysis and peritoneal dialysis do not have a significant effect on the concentration of clarithromycin in serum, which is also typical for other drugs of the macrolide group.
Storage conditions
Storage conditions
At a temperature not higher than 25 oC.
Shelf life
Shelf life
2 years.
Manufacturer
Manufacturer
Pharmstandard-Tomskkhimpharm, Russia
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 oC. |
| Manufacturer | Pharmstandard-Tomskkhimpharm, Russia |
| Medication form | pills |
| Brand | Pharmstandard-Tomskkhimpharm |
Other forms…
Related products
Buy Clarithromycin, 500 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.