No products in the cart.
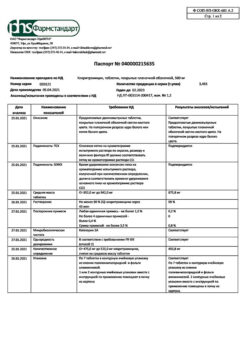
Clarithromycin, 250 mg 14 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: antibiotic-macrolide.
Code ATX: J01FA09
Pharmacological properties
Pharmacodynamics
. Clarithromycin is a semisynthetic antibiotic of the macrolide group and has an antibacterial effect by interacting with the 50S ribosomal subunit and inhibiting the protein synthesis of bacteria susceptible to it.
Clarithromycin has demonstrated high in vitro activity against both standard laboratory strains of bacteria and those isolated from patients in clinical practice. It shows high activity against many aerobic and anaerobic gram-positive and gram-negative microorganisms. Minimum inhibitory concentrations (MIC) of clarithromycin for most pathogens are lower than MIC of erythromycin on average by one log2 dilution.
Clarithromycin in vitro is highly active against Legionella pneumophila, Mycoplasma pneumoniae. It has a bactericidal effect against Helicobacter pylori, this activity of clarithromycin is higher at neutral pH than at acidic pH.
In addition, in vitro and in vivo data indicate that clarithromycin is active against clinically relevant mycobacterial species. Enterobacteriaceae and Pseudomonas spp. also other non-lactose-fermenting gram-negative bacteria are not sensitive to clarithromycin.
The activity of clarithromycin against most strains of the following microorganisms has been proven both in vitro and in clinical practice for the diseases listed under “Indications for use”.
Aerobic Gram-positive microorganisms: Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus pyogenes, Listeria monocytogenes.
Aerobic Gram-negative microorganisms: Haemophilus influenzae, Haemophilus parainfluenzae, Moraxella catarrhalis, Neisseria gonorrhoeae, Legionella pneumophila.
Other microorganisms: Mycoplasma pneumoniae, Chlamydia pneumoniae (TWAR). Mycobacteria: Mycobacterium leprae, Mycobacterium kansasii, Mycobacterium chelonae, Mycobacterium fortuitum, Mycobacterium avium complex (MAC) – complex including: Mycobacterium avium, Mycobacterium intracellulare.
The production of beta-lactamase has no effect on clarithromycin activity. Most staphylococcal strains resistant to methicillin and oxacillin are also resistant to clarithromycin.
Helicobacter pylori
The sensitivity of H.pylori to clarithromycin was studied on isolates of H. pylori isolated from 104 patients before starting therapy with the drug. Clarithromycin-resistant H.pylori strains were isolated in 4 patients, 2 patients had moderate resistance strains, and the remaining 98 patients had clarithromycin-sensitive H.pylori isolates.
Clarithromycin has in vitro action against most strains of the following microorganisms (but the safety and effectiveness of clarithromycin in clinical practice has not been confirmed by clinical studies, and the practical value remains unclear):
- aerobic gram-positive microorganisms: Streptococcus agalactiae, Streptococci
(groups C, F, G)., Viridans group streptococci;
- aerobic gram-negative microorganisms: Bordetella pertussis, Pasteurella
- anaerobic gram-positive microorganisms: Clostridium perfringens, Peptococcus niger, Propionibacterium acnes;
- anaerobic gram-negative microorganisms: Bacteroides melaninogenicus;
- Spirochetes: Borrelia burgdorferi, Treponema pallidum;
- Campylobacter: Campylobacter
The main metabolite of clarithromycin in humans is the microbiologically active metabolite 14-hydroxyclarithromycin (14-OH-clarithromycin). The microbiological activity of the metabolite is the same as that of the parent substance, or 1-2 times weaker against most microorganisms. The exception is H. influenzae, against which the effectiveness of the metabolite is twice as high. The parent substance and its main metabolite have either additive or synergistic effect against H.influenzae under conditions in vitro and in vivo depending on the bacterial strain.
Sensitivity test
Quantitative methods, which require measuring the diameter of the growth suppression zone, provide the most accurate estimates of the sensitivity of bacteria to antimicrobial agents. One recommended technique for sensitivity testing uses discs impregnated with 15 µg of clarithromycin (Kirby-Bauer disc-diffusion method); the diameters of the growth-suppression zones correlate with the IPC values of clarithromycin when interpreting the test. IPC values are determined by dilution in broth or agar.
When using these techniques, a report from the laboratory that the strain is “sensitive” indicates that the infectious agent is likely to respond to treatment. A “resistant” response indicates that the pathogen will probably not respond to treatment. A response of “intermediate sensitivity” suggests that the therapeutic effect of the drug may be ambiguous, or the microorganism may be sensitive using higher doses of the drug (intermediate sensitivity is also called “moderate sensitivity”).
Pharmacokinetics
absorption
The drug is easily and quickly absorbed in the gastrointestinal tract. Absolute bioavailability is about 50%. No cumulation was found when multiple doses of the drug were administered, and the metabolic pattern in the human body was not altered. Eating immediately before taking the drug increased the bioavailability of the drug by 25% on average. Overall, this increase is insignificant and should have little clinical significance with the recommended dosing regimens. Therefore, clarithromycin can be used regardless of food intake.
Distribution, metabolism and excretion In vitro
The in vitro studies showed that clarithromycin binds to plasma proteins by 70% at concentrations ranging from 0.45 to 4.5 µg/mL. At a concentration of 45.0 µg/ml, the binding decreases to 41%, probably as a result of saturation of the binding sites. This is observed only at concentrations many times greater than the therapeutic concentration.
In vivo
in vivo animal studies have shown that clarithromycin is present in all tissues except the central nervous system at concentrations several times greater than plasma. The highest concentrations (10-20 times higher than plasma concentrations) were found in the liver and lungs.
Health
. When clarithromycin was administered at a dose of 250 mg 2 times daily, the maximum equilibrium concentration (Cmax) of clarithromycin and 14-OH-clarithromycin in plasma was reached after 2-3 days and was 1 µg/mL and 0.6 µg/mL, respectively. The half-life (T1/2) of clarithromycin and its main metabolite was 3-4 hours and 5-6 hours, respectively.
When clarithromycin was administered at a dose of 500 mg twice daily, the Cmax of clarithromycin and 14-OH-clarithromycin in plasma was reached after the 5th dose. After the 5th and 7th dose, the Cmax of clarithromycin and 14-OH-clarithromycin in plasma averaged 2.7-2.9 mcg/mL and 0.88-0.83 mcg/mL, respectively. The T1/2 of clarithromycin and its main metabolite was 4.5-4.8 hours and 6.9-8.7 hours, respectively.
The cmax of 14-OH clarithromycin did not increase in proportion to the clarithromycin dose, whereas the T1/2 of both clarithromycin and its hydroxylated metabolite tended to increase with increasing dose.
This nonlinear pharmacokinetics of clarithromycin combined with decreased formation of 14-hydroxylated and N-demethylated products at high doses indicates a nonlinear metabolism of clarithromycin that becomes more pronounced at higher doses.
The kidneys excreted about 37.9% after oral clarithromycin doses of 250 mg and 46.0% after clarithromycin doses of 1200 mg; the intestines excreted about 40.2% and 29.1% (including subjects with only one stool sample containing 14.1%), respectively.
Patients
Clarithromycin and its metabolite 14-OH-clarithromycin penetrate rapidly into tissues and body fluids. There is limited evidence that the concentration of clarithromycin in cerebrospinal fluid during oral administration is negligible (i.e., only 1-2% of the serum concentration with normal blood-brain barrier permeability). Concentrations in tissues are usually several times higher than in blood serum.
The table gives examples of tissue and serum concentrations:
Concentrations (250 mg every 12 hours) | |||
Tissue type | Tissue (µg/g) | Serum (µg/mL) | |
My tonsils | 1.6 | 0.8 | |
Light | 8.8 | 1.7 | |
LiverLiver function disorders
In patients with moderate to severe hepatic impairment but with preserved renal function, clarithromycin dose adjustment is not necessary. Equilibrium plasma concentration and systemic clearance of clarithromycin do not differ between patients in this group and healthy patients. Equilibrium concentration of 14-OH clarithromycin is lower in people with hepatic impairment than in healthy subjects. Kidney dysfunction
In impaired renal function, the Cmax and minimum concentration (Cmin) of clarithromycin in plasma, the elimination half-life and the area under the pharmacokinetic concentration-time curve (AUC) of clarithromycin and its metabolite 14-OH-clarithromycin increase. The elimination constant and renal excretion decreases. The degree of change in these parameters depends on the degree of renal impairment.
Elderly patients
Elderly patients had higher blood concentrations of clarithromycin and its metabolite 14-OH-clarithromycin and slower excretion than the younger group. However, after adjustment for renal creatinine clearance, there were no differences in the two groups. Thus, the main influence on the pharmacokinetic parameters of clarithromycin is renal function, not age.
Patients with mycobacterial infections
. Equilibrium concentrations of clarithromycin and 14-OH clarithromycin in patients with HIV infection who received clarithromycin at conventional doses (500 mg twice daily) were similar to those in healthy subjects. However, when clarithromycin is used in higher doses that may be necessary to treat mycobacterial infections, concentrations of the antibiotic may be significantly higher than usual. In HIV-infected patients taking clarithromycin at a dose of 1000 mg/day or 2000 mg/day in two doses, equilibrium Cmax values were typically 2-4 mcg/ml and 5-10 mcg/ml, respectively. When using the drug in higher doses, a prolongation of the T1/2 was observed compared to that in healthy subjects receiving clarithromycin in usual doses. The increased plasma concentrations and prolongation of the elimination half-life when using clarithromycin at higher doses are due to the non-linear pharmacokinetics of the drug.
Combined treatment with omeprazole
Clarithromycin 500 mg 3 times daily in combination with omeprazole at a dose of 40 mg/day helps to increase the T1/2 and AUC0-24 of omeprazole. There was an 89% increase in AUC0-24 and 34% increase in T1/2 of omeprazole in all patients receiving combination therapy compared to those receiving omeprazole alone. Clarithromycin had Cmax, Cmin, and AUC0-8 increases of 10%, 27%, and 15%, respectively, compared with data when clarithromycin alone was used without omeprazole. At equilibrium, clarithromycin concentrations in gastric mucosa were 25 times higher 6 h after administration in the group receiving the combination compared with those receiving clarithromycin alone. Clarithromycin concentrations in gastric tissue 6 hours after the 2-drug regimen were twice as high as in the clarithromycin alone group.
Indications
Indications
Infectious and inflammatory diseases caused by microorganisms sensitive to clarithromycin in adults and children over 12 years of age:
lower respiratory tract infections (such as bronchitis, pneumonia);
upper respiratory tract infections (such as pharyngitis, sinusitis);
infections of the skin and soft tissues (such as folliculitis, inflammation of the subcutaneous tissue, erysipelas);
disseminated or localized mycobacterial infections caused by Mycobacterium avium and Mycobacterium intracellulare; localized infections caused by Mycobacterium chelonae, Mycobacterium fortuitum and Mycobacterium kansasii;
prevention of the spread of infection caused by the Mycobacterium avium complex (MAC) to HIV-infected patients with a CD4 lymphocyte (T-helper lymphocyte) content of no more than 100 per 1 mm3;
eradication of Helicobacter pylori and reduction in the frequency of relapses of duodenal ulcers;
odontogenic infections.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: macrolide antibiotic.
ATX code: J01FA09
Pharmacological properties
Pharmacodynamics
Clarithromycin is a semisynthetic antibiotic of the macrolide group and has an antibacterial effect by interacting with the 50S ribosomal subunit and inhibiting the protein synthesis of bacteria sensitive to it.
Clarithromycin demonstrated high activity in vitro against both standard laboratory strains of bacteria and those isolated from patients during clinical practice. Shows high activity against many aerobic and anaerobic gram-positive and gram-negative microorganisms. The minimum inhibitory concentrations (MICs) of clarithromycin for most pathogens are less than the MICs of erythromycin on average by one log2 dilution.
Clarithromycin is highly active in vitro against Legionella pneumophila, Mycoplasma pneumoniae. It has a bactericidal effect against Helicobacter pylori; this activity of clarithromycin is higher at neutral pH than at acidic pH.
In addition, in vitro and in vivo data indicate that clarithromycin is active against clinically relevant mycobacterial species. Enterobacteriaceae and Pseudomonas spp., as well as other non-lactose-fermenting gram-negative bacteria, are not sensitive to clarithromycin.
The activity of clarithromycin against most strains of the microorganisms listed below has been proven both in vitro and in clinical practice for the diseases listed in the “Indications for use” section.
Aerobic gram-positive microorganisms: Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus pyogenes, Listeria monocytogenes.
Aerobic gram-negative microorganisms: Haemophilus influenzae, Haemophilus parainfluenzae, Moraxella catarrhalis, Neisseria gonorrhoeae, Legionella pneumophila.
Other microorganisms: Mycoplasma pneumoniae, Chlamydia pneumoniae (TWAR). Mycobacteria: Mycobacterium leprae, Mycobacterium kansasii, Mycobacterium chelonae, Mycobacterium fortuitum, Mycobacterium avium complex (MAC) – a complex including: Mycobacterium avium, Mycobacterium intracellulare.
The production of beta-lactamase does not affect the activity of clarithromycin. Most strains of staphylococci resistant to methicillin and oxacillin are also resistant to clarithromycin.
Helicobacter pylori
The sensitivity of H. pylori to clarithromycin was studied on H. pylori isolates isolated from 104 patients before the start of drug therapy. H. pylori strains resistant to clarithromycin were isolated in 4 patients, moderately resistant strains were isolated in 2 patients, and in the remaining 98 patients, H. pylori isolates were sensitive to clarithromycin.
Clarithromycin is effective in vitro and against most strains of the following microorganisms (however, the safety and effectiveness of the use of clarithromycin in clinical practice has not been confirmed by clinical studies, and the practical significance remains unclear):
aerobic gram-positive microorganisms: Streptococcus agalactiae, Streptococci
(groups C, F, G), Viridans group streptococci;
aerobic gram-negative microorganisms: Bordetella pertussis, Pasteurella
anaerobic gram-positive microorganisms: Clostridium perfringens, Peptococcus niger, Propionibacterium acnes;
anaerobic gram-negative microorganisms: Bacteroides melaninogenicus;
spirochetes: Borrelia burgdorferi, Treponema pallidum;
campylobacter: Campylobacter
The main metabolite of clarithromycin in the human body is the microbiologically active metabolite 14-hydroxyclarithromycin (14-OH-clarithromycin). The microbiological activity of the metabolite is the same as that of the parent substance, or 1-2 times weaker against most microorganisms. The exception is H. influenzae, for which the effectiveness of the metabolite is twice as high. The parent substance and its major metabolite have either additive or synergistic effects against H. influenzae in vitro and in vivo, depending on the bacterial strain.
Sensitivity test
Quantitative methods that require measuring the diameter of the zone of growth inhibition provide the most accurate estimates of bacterial sensitivity to antimicrobial drugs. One recommended technique for determining sensitivity uses disks impregnated with 15 μg of clarithromycin (Kirby-Bauer disk diffusion method); when interpreting the test, the diameters of the zones of growth inhibition correlate with the MIC values of clarithromycin. MIC values are determined by broth or agar dilution method.
With these techniques, a report from the laboratory that the strain is “susceptible” indicates that the infectious agent is likely to respond to treatment. A “resistant” response indicates that the pathogen may not respond to treatment. An “intermediate sensitivity” response suggests that the therapeutic effect of the drug may be ambiguous or that the organism may be sensitive when using higher doses of the drug (intermediate sensitivity is also called “moderate sensitivity”).
Pharmacokinetics
Suction
The drug is easily and quickly absorbed from the gastrointestinal tract. Absolute bioavailability is about 50%. With repeated doses of the drug, practically no accumulation was detected, and the nature of metabolism in the human body did not change. Eating immediately before taking the drug increased the bioavailability of the drug by an average of 25%. Overall, this increase is small and should be of little clinical significance at recommended dosing regimens. Thus, clarithromycin can be used regardless of food intake.
Distribution, metabolism and excretion In vitro
In vitro studies have shown that clarithromycin is 70% bound to plasma proteins at concentrations ranging from 0.45 to 4.5 mcg/ml. At a concentration of 45.0 μg/ml, binding decreases to 41%, probably as a result of saturation of binding sites. This is observed only at concentrations many times higher than the therapeutic value.
In vivo
In vivo studies in animals have shown that clarithromycin is present in all tissues, with the exception of the central nervous system, in concentrations several times higher than plasma concentrations. The highest concentrations (10-20 times higher than plasma levels) were found in the liver and lungs.
Healthy
When clarithromycin was prescribed at a dose of 250 mg 2 times a day, the maximum equilibrium concentration (Cmax) of clarithromycin and 14-OH-clarithromycin in plasma was reached after 2-3 days and was 1 μg/ml and 0.6 μg/ml, respectively. The half-life (T1/2) of clarithromycin and its main metabolite was 3-4 hours and 5-6 hours, respectively.
When clarithromycin was prescribed at a dose of 500 mg 2 times a day, Cmax of clarithromycin and 14-OH-clarithromycin in plasma was achieved after taking the 5th dose. After taking the 5th and 7th doses, the Cmax of clarithromycin and 14-OH-clarithromycin in plasma averaged 2.7-2.9 μg/ml and 0.88-0.83 μg/ml, respectively. T1/2 of clarithromycin and its main metabolite was 4.5-4.8 hours and 6.9-8.7 hours, respectively.
Cmax of 14-OH-clarithromycin did not increase proportionally to the dose of clarithromycin, while T1/2 of both clarithromycin and its hydroxylated metabolite tended to increase with increasing dose.
This nonlinear pharmacokinetics of clarithromycin, coupled with a decrease in the formation of 14-hydroxylated and N-demethylated products at high doses, indicates a nonlinear metabolism of clarithromycin, which becomes more pronounced at high doses.
About 37.9% are excreted by the kidneys after oral administration of clarithromycin at a dose of 250 mg and 46.0% after administration of clarithromycin at a dose of 1200 mg; the intestines excreted about 40.2% and 29.1% (including the subject with only one stool sample containing 14.1%), respectively.
Patients
Clarithromycin and its metabolite 14-OH-clarithromycin quickly penetrate into body tissues and fluids. There is limited data indicating that the concentration of clarithromycin in the cerebrospinal fluid after oral administration is negligible (i.e., only 1-2% of the serum concentration when the blood-brain barrier is normally permeable). Concentrations in tissues are usually several times higher than in serum.
The table provides examples of tissue and serum concentrations:
Concentrations (250 mg every 12 hours)
Type of fabric
Tissue (µg/g)
Serum (µg/ml)
Tonsils
1.6
0.8
Lungs
8.8
1.7
Liver dysfunction
In patients with moderate to severe liver dysfunction, but with preserved renal function, no dose adjustment of clarithromycin is required. The steady-state plasma concentration and systemic clearance of clarithromycin do not differ between patients in this group and healthy patients. The steady-state concentration of 14-OH-clarithromycin in people with impaired liver function is lower than in healthy people. Renal dysfunction
If renal function is impaired, the Cmax and minimum concentration (Cmin) of clarithromycin in the blood plasma, the half-life, and the area under the pharmacokinetic concentration-time curve (AUC) of clarithromycin and its metabolite 14-OH-clarithromycin increase. The elimination constant and renal excretion decrease. The degree of changes in these parameters depends on the degree of renal dysfunction.
Elderly patients
In elderly patients, the concentration of clarithromycin and its metabolite 14-OH-clarithromycin in the blood was higher, and elimination was slower than in the group of young people. However, after adjustment for renal creatinine clearance, there was no difference in both groups. Thus, the main influence on the pharmacokinetic parameters of clarithromycin is renal function, and not age.
Patients with mycobacterial infections
Steady-state concentrations of clarithromycin and 14-OH-clarithromycin in patients with HIV infection receiving clarithromycin at usual doses (500 mg twice daily) were similar to those in healthy subjects. However, when clarithromycin is used in higher doses, which may be required to treat mycobacterial infections, antibiotic concentrations may be significantly higher than usual. In patients with HIV infection taking clarithromycin at a dose of 1000 mg/day or 2000 mg/day in two doses, steady-state Cmax values were usually 2-4 μg/ml and 5-10 μg/ml, respectively. When using the drug in higher doses, a prolongation of T1/2 was observed compared with that in healthy people receiving clarithromycin in usual doses. Increased plasma concentrations and prolongation of the half-life when using clarithromycin at higher doses are associated with the nonlinear pharmacokinetics of the drug.
Combination treatment with omeprazole
Clarithromycin 500 mg 3 times a day in combination with omeprazole at a dose of 40 mg/day increases T1/2 and AUC0-24 of omeprazole. In all patients receiving combination therapy, compared with those receiving omeprazole alone, there was an 89% increase in AUC0-24 and a 34% increase in omeprazole T1/2. For clarithromycin, Cmax, Cmin and AUC0-8 increased by 10%, 27% and 15%, respectively, compared with data when clarithromycin alone was used without omeprazole. At steady state, clarithromycin concentrations in the gastric mucosa 6 hours after dosing in the group receiving the combination were 25 times higher than those in those receiving clarithromycin alone. Concentrations of clarithromycin in gastric tissue 6 hours after taking 2 drugs were 2 times higher than the data obtained in the group of patients receiving clarithromycin alone.
Special instructions
Special instructions
Long-term use of antibiotics can lead to the formation of colonies with an increased number of insensitive bacteria and fungi. In case of superinfection, appropriate therapy must be prescribed.
Prescription of clarithromycin to pregnant women should be carried out with a careful assessment of the risk-benefit ratio, especially during the first three months of pregnancy.
Liver dysfunction (increased liver enzyme activity in the blood, hepatocellular and/or cholestatic hepatitis with or without jaundice) has been reported with the use of clarithromycin. Liver dysfunction can be severe but is usually reversible.
There have been cases of fatal liver failure, mainly associated with the presence of serious concomitant diseases and/or concomitant use of other drugs. If signs and symptoms of hepatitis appear, such as anorexia, jaundice, dark urine, itching, abdominal tenderness on palpation, clarithromycin therapy should be stopped immediately.
In the presence of chronic liver diseases, it is necessary to regularly monitor serum enzymes.
When treated with almost all antibacterial agents, including clarithromycin, cases of pseudomembranous colitis have been described, the severity of which can range from mild to life-threatening. Clostridium difficile-associated diarrhea has been reported during treatment with almost all antibacterial drugs, including clarithromycin, the severity of which can range from mild diarrhea to life-threatening colitis. Antibacterial drugs can change the normal intestinal microflora, which can lead to the growth of Clostridium difficile.
Pseudomembranous colitis caused by Clostridium difficile should be suspected in any patient who develops diarrhea after taking antibacterial agents. After a course of antibiotic therapy, careful medical monitoring of the patient is necessary. Cases of the development of pseudomembranous colitis 2 months after taking antibiotics have been described.
When treated with macrolides, including clarithromycin, prolongation of cardiac repolarization and QT interval was observed, causing the risk of developing cardiac arrhythmia and torsade de pointes (see section “Side effects”). Since the following situations may lead to an increased risk of developing ventricular arrhythmias (including torsade de pointes), clarithromycin should not be used in the following categories of patients:
in patients with hypokalemia (see section “Contraindications”);
simultaneous administration of clarithromycin with astemizole, cisapride, pimozide and terfenadine is contraindicated (see section “Contraindications”);
in patients with congenital or acquired documented prolongation of the QT interval or a history of ventricular arrhythmia (see section
“Contraindications”).
Clarithromycin should be used with caution in the following categories of patients:
in patients with coronary artery disease, severe heart failure, conduction disorders or clinically significant bradycardia;
in patients with electrolyte disturbances such as hypomagnesemia;
in patients simultaneously taking other drugs associated with prolongation of the QT interval (see section “Interaction with other drugs”).
Epidemiological studies examining the risk of adverse cardiovascular outcomes with macrolide use have reported mixed results. Some observational studies have identified a short-term risk of arrhythmia, myocardial infarction, and cardiovascular death associated with the use of macrolides, including clarithromycin. When prescribing clarithromycin, the expected benefits of taking the drug should be weighed against these risks.
It is possible to develop cross-resistance to clarithromycin and other macrolide antibiotics, as well as lincomycin and clindamycin.
Given the increasing resistance of Streptococcus pneumoniae to macrolides, it is important to perform susceptibility testing when prescribing clarithromycin to patients with community-acquired pneumonia. For hospital-acquired pneumonia, clarithromycin should be used in combination with appropriate antibiotics.
Mild to moderate skin and soft tissue infections are most often caused by Staphylococcus aureus and Streptococcus pyogenes. Moreover, both pathogens can be resistant to macrolides. Therefore, it is important to conduct a sensitivity test.
Macrolides can be used for infections caused by Corynebacterium minutissimum, acne vulgaris and erysipelas, as well as in situations where penicillin cannot be used.
If acute hypersensitivity reactions occur, such as anaphylactic reaction, severe cutaneous drug reactions (eg, acute generalized exanthematous pustulosis), Stevens-Johnson syndrome, toxic epidermal necrolysis, and drug rash with eosinophilia and systemic symptoms (DRESS syndrome), discontinue clarithromycin immediately and initiate appropriate therapy.
In case of combined use with warfarin or other indirect anticoagulants, it is necessary to monitor the INR and prothrombin time (see section “Interaction with other drugs”).
Impact on the ability to drive vehicles and machinery
There are no data regarding the effect of clarithromycin on the ability to drive a car or use machinery.
Caution should be exercised when operating vehicles and machinery, given the potential for dizziness, vertigo, confusion and disorientation that may occur when using this drug.
Active ingredient
Active ingredient
Clarithromycin
Composition
Composition
1 film-coated tablet contains:
active substance: clarithromycin in terms of 100% anhydrous substance 250 mg or 500 mg;
excipients: potato starch 46.0 mg or 92.0 mg, microcrystalline cellulose 75.0 mg or 150.0 mg, povidone (low molecular weight medical polyvinylpyrrolidone) 40.0 mg or 80.0 mg, pregelatinized starch (starch-1500) 30.0 mg or 60.0 mg, colloidal silicon dioxide (aerosil) 4.5 mg or 9.0 mg, magnesium stearate 4.5 mg or 9.0 mg;
shell: opadry II (polyvinyl alcohol, partially hydrolyzed 8.0 mg or 16.0 mg, macrogol (polyethylene glycol) 3350 4.040 mg or 8.080 mg, talc 2.960 mg or 5.920 mg, titanium dioxide E171 4.374 mg or 8.748 mg, yellow-based aluminum varnish quinoline E104 0.602 mg or 1.204 mg, iron (II) oxide dye E172 0.006 mg or 0.012 mg, aluminum varnish based on sunset yellow E110 0.014 mg or 0.028 mg, aluminum varnish based on indigo carmine E132 0.004 mg or 0.008 mg).
Pregnancy
Pregnancy
The safety of clarithromycin during pregnancy and breastfeeding has not been established.
The use of clarithromycin during pregnancy (especially in the first trimester) is possible only when there is no alternative therapy and the potential benefit to the mother outweighs the potential risk to the fetus.
Clarithromycin is excreted in breast milk. If it is necessary to use the drug during lactation, breastfeeding should be stopped.
Contraindications
Contraindications
hypersensitivity to clarithromycin, macrolides and other components of the drug;
simultaneous use of clarithromycin with the following drugs: astemizole, cisapride, pimozide, terfenadine (see section “Interaction with other drugs”);
simultaneous use of clarithromycin with ergot alkaloids, for example, ergotamine, dihydroergotamine (see section “Interaction with other drugs”);
simultaneous use of clarithromycin with midazolam for oral use (see section “Interaction with other drugs”);
simultaneous use of clarithromycin with HMG-CoA reductase inhibitors (statins), which are largely metabolized by the CYP3A4 isoenzyme (lovastatin or simvastatin), due to an increased risk of myopathy, including rhabdomyolysis (see section “Interaction with other drugs”);
simultaneous use of clarithromycin with colchicine (see section “Interaction with other drugs”);
simultaneous use of clarithromycin with ticagrelor or ranolazine;
history of prolongation of the QT interval (congenital or acquired registered prolongation of the QT interval) or ventricular arrhythmia, including ventricular tachycardia of the “pirouette” type (see sections “Special instructions” and “Interaction with other drugs”);
hypokalemia (risk of QT interval prolongation);
severe liver failure occurring simultaneously with renal failure
history of cholestatic jaundice/hepatitis that developed during the use of clarithromycin (see section “Special Instructions”);
porphyria;
breastfeeding period;
age up to 12 years (efficacy and safety have not been established).
With caution
Moderate to severe renal failure; moderate to severe liver failure; simultaneous use of clarithromycin with benzodiazepines, such as alprazolam, triazolam, midazolam for intravenous use or for application to the oral mucosa (see section “Interaction with other drugs”); simultaneous use with drugs that are metabolized by the CYP3A isoenzyme, for example, carbamazepine, cilostazol, cyclosporine, disopyramide, methylprednisolone, omeprazole, indirect anticoagulants (for example, warfarin), quinidine, rifabutin, sildenafil, tacrolimus, vinblastine (see section “Interaction with other drugs”); simultaneous use with drugs that induce the CYP3A4 isoenzyme, for example, rifampicin, phenytoin, carbamazepine, phenobarbital, St. John’s wort (see section “Interaction with other drugs”); simultaneous use of clarithromycin with statins that do not depend on the metabolism of the CYP3A isoenzyme (for example, fluvastatin) (see section “Interaction with other drugs”); simultaneous use with blockers of “slow” calcium channels that are metabolized by the CYP3A4 isoenzyme (for example, verapamil, amlodipine, diltiazem); patients with coronary heart disease (CHD), severe heart failure, hypomagnesemia, conduction disturbances or clinically significant bradycardia, as well as patients simultaneously taking class IA (quinidine, procainamide) and class III antiarrhythmic drugs (dofetilide, amiodarone, sotalol); pregnancy.
Side Effects
Side Effects
Classification of adverse reactions by frequency (number of reported cases/number of patients): very common (> 1/10), common (> 1/100, 1/1000, < 1/100), frequency unknown (side effects from post-marketing experience; frequency cannot be estimated based on available data).
Allergic reactions: often – rash; uncommon – anaphylactoid reaction1, hypersensitivity, bullous dermatitis1, itching, urticaria, maculopapular rash3; frequency unknown – anaphylactic reaction, angioedema, serious cutaneous adverse reactions (for example, acute generalized exanthematous pustulosis), Stevens-Johnson syndrome, toxic epidermal necrolysis, drug rash with eosinophilia and systemic symptoms (DRESS syndrome).
From the nervous system: often – headache, insomnia; uncommon – loss of consciousness1, dyskinesia1, dizziness, drowsiness, tremor, anxiety, increased excitability3; frequency unknown – convulsions, psychotic disorders, confusion, depersonalization, depression, disorientation, hallucinations, dream disturbances (nightmare dreams), paresthesia, mania.
From the skin: often – intense sweating; frequency unknown – acne. From the urinary system: frequency unknown – renal failure, interstitial nephritis.
From the side of metabolism and nutrition: infrequently – anorexia, loss of appetite.
From the musculoskeletal system: infrequently – muscle spasm3, musculoskeletal stiffness1, myalgia2; frequency unknown – rhabdomyolysis3, myopathy.
From the digestive system: often – diarrhea, vomiting, dyspepsia, nausea, abdominal pain; uncommon – esophagitis1, gastroesophageal reflux disease2, gastritis, proctalgia2, stomatitis, glossitis, bloating4, constipation, dry mouth, belching, flatulence, cholestasis4, hepatitis incl. cholestatic or hepatocellular4; frequency unknown – acute pancreatitis, discoloration of the tongue and teeth, liver failure, cholestatic jaundice.
From the respiratory system: infrequently – asthma1, nosebleeds2, pulmonary embolism1.
From the senses: often – dysgeusia; infrequently – vertigo, hearing loss, ringing in the ears; frequency unknown – deafness, ageusia (loss of taste), parosmia, anosmia.
From the cardiovascular system: often – vasodilation1; uncommon – cardiac arrest1, atrial fibrillation1, prolongation of the QT interval on the electrocardiogram, extrasystole1, palpitations; frequency unknown – ventricular tachycardia, including pirouette type, ventricular fibrillation, bleeding.
Laboratory indicators: often – deviation in the liver test; infrequently – increased creatinine concentration1, increased urea concentration1, changes in the albumin-globulin ratio1, leukopenia, neutropenia4, eosinophilia4, thrombocythemia3, increased activity of: alanine aminotransferase (ALT), aspartate aminotransferase (AST), gammaglutamyltransferase (GGTP)4, alkaline phosphatase4, lactate dehydrogenase (LDG)4; frequency unknown – agranulocytosis, thrombocytopenia, increased international normalized ratio (INR), prolongation of prothrombin time, change in urine color, increased bilirubin concentration in the blood.
General disorders: very often – phlebitis at the injection site1; often – pain at the injection site1, inflammation at the injection site1; infrequently – malaise4, hyperthermia3, asthenia, chest pain4, chills4, fatigue4.
Infectious and parasitic diseases: uncommon – cellulitis1, candidiasis, gastroenteritis2, secondary infections3 (including vaginal); frequency unknown – pseudomembranous colitis, erysipelas.
It is assumed that the frequency, type and severity of adverse reactions in children is the same as in adults.
Immunosuppressed patients: In patients with AIDS and other immunodeficiencies receiving clarithromycin in higher doses over a long period of time to treat mycobacterial infections, it is often difficult to distinguish adverse effects of the drug from symptoms of HIV infection or concomitant disease.
The most common adverse events in patients taking a daily dose of clarithromycin of 1000 mg were: nausea, vomiting, taste disturbance, abdominal pain, diarrhea, rash, flatulence, headache, constipation, hearing loss, increased AST and ALT activity in the blood. Low incidence adverse events such as shortness of breath, insomnia and dry mouth were also reported.
In patients with suppressed immunity, laboratory parameters were assessed, analyzing their significant deviations from the norm (sharp increase or decrease). Based on this criterion, a significant increase in AST and ALT activity in the blood, as well as a decrease in the number of leukocytes and platelets, was observed in 2-3% of patients receiving clarithromycin at a dose of 1000 mg daily. Increases in residual urea nitrogen concentrations have also been reported in a small number of patients.
*In some reports of rhabdomyolysis, clarithromycin was co-administered with other drugs known to be associated with rhabdomyolysis (statins, fibrates, colchicine or allopurinol).
1 – Reports of these adverse reactions were received only when using clarithromycin, in dosage form (DF) lyophilisate for the preparation of solution for infusion.
2 – Reports of these adverse reactions were received only with the use of clarithromycin, in LF extended-release film-coated tablets.
3 – Reports of these adverse reactions were received only when using clarithromycin, in LF granules for the preparation of an oral suspension.
4 – Reports of these adverse reactions were received only with the use of clarithromycin in LF film-coated tablets.
Interaction
Interaction
The use of the following drugs with clarithromycin is contraindicated due to the potential for serious side effects
Cisapride pimozide terfenadine astemizole
When clarithromycin is taken together with cisapride/pimozide/terfenadine/astemizole, it is possible to increase the concentration of the latter in the blood plasma, which can lead to an increase in the QT interval and the appearance of cardiac arrhythmias including ventricular tachycardia, ventricular fibrillation, and ventricular tachycardia of the “pirouette” type (see section “Contraindications”).
Ergot alkaloids
When clarithromycin is used together with ergotamine or dihydroergotamine, acute poisoning with drugs of the ergotamine group is possible: vascular spasm, ischemia of the limbs and other tissues, including the central nervous system. Concomitant use of clarithromycin and ergot alkaloids is contraindicated (see section “Contraindications”)
Effect of other drugs on clarithromycin
The following drugs have a proven or suspected effect on clarithromycin concentrations. If they are used together with clarithromycin, dosage adjustments and switching to alternative treatment may be required.
Drugs that are inducers of the CYP3A isoenzyme (for example, rifampicin, phenytoin, carbamazepine, phenobarbital, St. John’s wort) can induce the metabolism of clarithromycin. This may result in subtherapeutic concentrations of clarithromycin, resulting in reduced effectiveness. In addition, it is necessary to monitor the concentration of the CYP3A inducer in the blood plasma, which may increase due to inhibition of the CYP3A isoenzyme by clarithromycin.
Efavirenz nevirapine rifampicin rifabutin rifapentine
Strong inducers of the cytochrome P430 system such as efavirenz nevirapine rifampicin rifabutin and rifapentine can accelerate the metabolism of clarithromycin and thus reduce the concentration of clarithromycin in the blood and weaken the therapeutic effect and, at the same time, increase the concentration of 14-(R)-hydroxyclarithromycin.
Etravirine
The concentration of clarithromycin decreases with the use of etravirine, but the concentration of the active metabolite 14-(R)-hydroxyclarithromycin increases.
Fluconazole
Co-administration of fluconazole at a dose of 200 mg daily and clarithromycin at a dose of 1 g/day increases the minimum mean steady-state concentration of clarithromycin (Cmin) and the area under the clarithromycin concentration-time curve by 33% and 18%, respectively. No dose adjustment of clarithromycin is required in case of concomitant use of fluconazole.
Ritonavir
Co-administration of ritonavir at a dose of 600 mg/day and clarithromycin 1 g/day leads to a decrease in the metabolism of clarithromycin. When co-administered with ritonavir, the maximum steady-state concentration (Cmax) of clarithromycin increased by 31%, Cmin increased by 182% and the area under the concentration-time curve increased by 77%. Complete inhibition of the formation of 14-(R)-hydroxyclarithromycin was noted. In patients with chronic renal failure, dose adjustment is necessary: with a creatinine clearance of 30-60 ml/min, the dose of clarithromycin should be reduced by 50% and with a creatinine clearance of less than 30 ml/min by 75%. Doses of clarithromycin exceeding 1 g/day should not be used together with ritonavir.
Oral hypoglycemic drugs/insulin
When clarithromycin is used concomitantly with oral hypoglycemic agents and/or insulin, severe hypoglycemia may occur. Close monitoring of glucose levels is recommended.
Effect of clarithromycin on other drugs
Antiarrhythmic drugs
Ventricular tachycardia of the pirouette type may occur with the combined use of clarithromycin and antiarrhythmic drugs (quinidine procainamide). When clarithromycin is coadministered with these drugs, the electrocardiogram should be regularly monitored for prolongation of the QT interval and serum concentrations of these drugs should also be monitored.
Interactions caused by CYP3A isoenzymes
Co-administration of clarithromycin and drugs primarily metabolized by CYP3A isoenzymes may enhance or prolong both therapeutic and side effects. Clarithromycin should be used with caution in patients receiving drugs that are substrates of the CYP3A isoenzyme, especially if these drugs have a narrow therapeutic range (for example, carbamazepine) and/or are extensively metabolized by this enzyme; if necessary, the dose of the drug taken together with clarithromycin should be adjusted. Also, whenever possible, serum concentrations of drugs primarily metabolized by the CYP3A isoenzyme should be monitored.
3-Hydroxy-3-methylglutaryl-coenzyme A reductase (HMG-CoA reductase) inhibitors (statins)
Clarithromycin increases the concentration of HMG-CoA reductase inhibitors (for example, lovastatin, simvastatin). Co-administration of clarithromycin with lovastatin or simvastatin is contraindicated (see section “Contraindications”) due to the fact that these statins are largely metabolized by the CYP3A4 isoenzyme and combined use with clarithromycin increases their serum concentrations, which leads to an increased risk of developing myopathy. If clarithromycin is necessary, lovastatin or simvastatin should be discontinued during therapy.
Indirect anticoagulants
When taking warfarin and clarithromycin together, bleeding is possible, expressed by an increase in INR and prothrombin time. In case of combined use with warfarin or other indirect anticoagulants, it is necessary to monitor the INR and prothrombin time.
Omeprazole
When clarithromycin and omeprazole are taken simultaneously, plasma levels of clarithromycin and its metabolite increase. The concentration of clarithromycin in the tissues and mucous membranes of the stomach also increases when taken simultaneously.
Sildenafil tadalafil vardenafil
Concomitant use of clarithromycin with sildenafil, tadalafil or vardenafil (phosphodiesterase 5 inhibitors) may lead to increased phosphodiesterase inhibitory effects. A dose reduction of sildenafil, tadalafil and vardenafil may be required.
Theophylline carbamazepine
When clarithromycin and theophylline or carbamazepine are used together, the concentration of these drugs in the systemic circulation may increase.
Tolterodine
When co-administering clarithromycin with tolterodine in patients with low CYP2D6 activity, a dose reduction of tolterodine may be required in the presence of clarithromycin (a CYP3A inhibitor).
Benzodiazepines (eg alprazolam midazolam triazolam)
When clarithromycin (1 g/day) was taken together with midazolam (orally), an increase in the area under the concentration-time curve of midazolam by 7 times was observed. Concomitant oral administration of clarithromycin and midazolam should be avoided. When using midazolam (intravenous) and clarithromycin, dose adjustment may be required.
The same precautions should be applied to other benzodiazepines that are metabolized by CYP3A, including triazolam and alprazolam. For benzodiazepines whose elimination does not depend on the CYP3A isoenzyme (temazepam nitrazepam lorazepam), a clinically significant interaction with clarithromycin is unlikely.
When clarithromycin and triazolam are used together, effects on the central nervous system (CNS) such as drowsiness and confusion are possible. Therefore, it is advisable to monitor for symptoms of CNS impairment if coadministration occurs.
Interaction with other drugs
Colchicine
When clarithromycin is taken together with colchicine, the effect of colchicine may be enhanced. It is necessary to monitor the possible development of clinical symptoms of colchicine poisoning, especially in elderly patients and patients with chronic renal failure (some cases have been reported to be fatal).
In patients with normal renal and hepatic function, the dose of colchicine should be reduced when used concomitantly with clarithromycin.
The simultaneous use of clarithromycin and colchicine is contraindicated in patients with impaired liver and kidney function (see section “Contraindications”).
Digoxin
Coadministration of digoxin and clarithromycin may result in increased serum digoxin concentrations in patients. When taking clarithromycin and digoxin together, the concentration of digoxin in the blood serum should be carefully monitored (an increase in its concentration and the development of potentially detailed arrhythmias is possible).
Zidovudine
Concomitant use of clarithromycin and zidovudine in adult HIV-infected patients may result in a decrease in the steady-state concentration of zidovudine. Because clarithromycin interferes with the absorption of zidovudine when taken orally, interactions can be largely avoided by taking clarithromycin and zidovudine 4 hours apart.
Phenytoin and valproic acid
When using phenytoin or valproic acid together with clarithromycin, it is recommended to determine their serum concentrations as there are reports of their increase.
Bidirectional drug interactions
Atazanavir
Coadministration of clarithromycin (1 g/day) and atazanavir (400 mg/day) may result in a twofold increase in clarithromycin exposure and a 70% decrease in 14-(R)-hydroxyclarithromycin exposure, with a 28% increase in the AUC of atazanavir.
In patients with normal renal function, a dose reduction of clarithromycin is not required.
In patients with moderate renal impairment (creatinine clearance 30-60 ml/min), the dose of clarithromycin should be reduced by 50%.
In patients with creatinine clearance less than 30 ml/min, the dose of clarithromycin should be reduced by 75%. Clarithromycin in doses exceeding 1 g/day should not be used in conjunction with protease inhibitors.
Blockers of “slow” calcium channels
When using clarithromycin simultaneously with blockers of “slow” calcium channels that are metabolized by the CYP3A isoenzyme (for example, verapamil amlodipine diltiazem), caution should be exercised since there is a risk of arterial hypotension. Plasma concentrations of clarithromycin, as well as slow calcium channel blockers, may increase with simultaneous use. Arterial hypotension, bradyarrhythmia and lactic acidosis are possible when taking clarithromycin and verapamil simultaneously.
Itraconazole
When clarithromycin and itraconazole are taken together, a mutual increase in the concentration of drugs in plasma is possible. Patients taking itraconazole and clarithromycin concomitantly should be closely monitored for symptoms of increased or prolonged pharmacological effects of these drugs.
Saquinavir
With simultaneous administration of clarithromycin (1 g / day) and saquinavir (in soft gelatin capsules 1200 mg 3 times a day), it is possible to increase the area under the concentration-time curve and Cmax of saquinavir by 177% and 187%, respectively, and clarithromycin by 40%. When these two drugs are used together for a limited time at the doses indicated above, no dose adjustment is required.
Overdose
Overdose
Symptoms: Taking a large dose of clarithromycin may cause gastrointestinal symptoms.
In one patient with a history of bipolar disorder, changes in mental status, paranoid behavior, hypokalemia, and hypoxemia were described after taking 8 g of clarithromycin.
Treatment: in case of overdose, the unabsorbed drug should be removed from the gastrointestinal tract (gastric lavage, activated charcoal, etc.) and symptomatic therapy should be carried out. Hemodialysis and peritoneal dialysis do not have a significant effect on the concentration of clarithromycin in serum, which is also typical for other macrolide drugs.
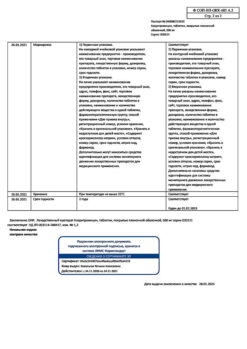
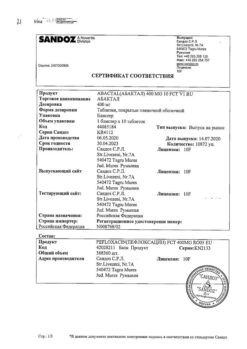
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25 ° C. Keep out of the reach of children.
Shelf life
Shelf life
2 years. Do not use after expiration date.
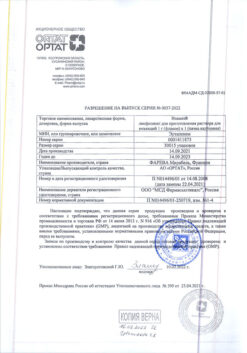
Manufacturer
Manufacturer
Rapharma JSC, Russia
Additional information
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store in a light-protected place at a temperature not exceeding 25 °С. Keep out of reach of children. |
| Manufacturer | Rapharma JSC, Russia |
| Medication form | pills |
| Brand | Rapharma JSC |
Other forms…
Related products
Buy Clarithromycin, 250 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.