No products in the cart.
Description
A second-generation macrolide group antibiotic with a broad spectrum of antimicrobial action. It has bacteriostatic action. It disrupts protein synthesis of microorganisms – it binds to 50S subunit of the ribosome membrane of the microbial cell.
Clarithromycin is active against Streptococcus agalactiae (Streptococcus pyogenes, Streptococcus viridans, Streptococcus pneumoniae), Haemophilus influenzae (parainfluenzae), Haemophilus ducreyi, Neisseria gonorrhoeae, Neisseria meningitidis, Listeria monocytogenes, Legionella pneumophila, Mycoplasma pneumoniae, Helicobacter (Campilobacter) pylori, Campilobacter jejuni, Chlamidia pneumoniae (trachomatis), Moraxella (Branhamella) catarrhalis, Bordetella pertussis, Propionibacterium acnes, Staphylococcus aureus, Ureaplasma urealyticum, Toxoplasma gondii, Corynebacterium spp., Borrelia burgdorferi, Pasteurella multocida, some anaerobes (Eubacterium spp., Peptococcus spp., Propionibacterium spp., Clostridium perfringens, Bacteroides melaninogenicus) and all mycobacteria (including Mycobacterium avium, Mycobacterium leprae) except Mycobacterium tuberculosis.
Pharmacokinetics
Intake
After oral administration, absorption is rapid. Food slows absorption without significantly affecting bioavailability. The bioavailability of clarithromycin in suspension form is equivalent or slightly higher than when taken as tablets.
Two Cmax peaks are recorded after a single dose. The second peak is due to the ability of the drug to concentrate in the gallbladder with subsequent gradual or rapid release. Time to reach Cmax when administered orally in a dose of 250 mg is 1-3 hours.
Distribution and metabolism
The binding to plasma proteins is more than 90%.
After oral administration 20% of the taken dose is quickly hydroxylated in the liver with the participation of cytochrome P450 isoenzymes to form the main metabolite – 14-hydroxyclarithromycin, which has strong antimicrobial activity against Haemophilus influenzae.
In regular administration of 250 mg/day the Css of unchanged drug and its main metabolite are 1 and 0.6 mcg/ml, respectively; T1/2 is 3-4 h and 5-6 h, respectively. When increasing the dose to 500 mg/day Css of unchanged drug and its metabolite in plasma is 2.7-2.9 and 0.83-0.88 µg/ml, respectively; T1/2 is 4.8-5 h and 6.9-8.7 h, respectively. In therapeutic concentrations it accumulates in the lungs, skin and soft tissues (concentrations in them are 10 times higher than in blood serum).
Extracted by the kidneys and in the feces (20-30% – unchanged, the rest – as metabolites). With a single use in doses of 250 mg and 1.2 g, 37.9% and 46% were excreted in the urine, 40.2% and 29.1% in the faeces, respectively.
Indications
Indications
Treatment of infectious diseases caused by microorganisms sensitive to the drug:
lower respiratory tract infections (bronchitis, pneumonia);
upper respiratory tract infections (pharyngitis, sinusitis);
otitis;
skin and soft tissue infections (folliculitis, erysipelas);
widespread or localized mycobacterial infections caused by Mycobacterium avium and Mycobacterium intracellulare;
localized infections caused by Mycobacterium chelonae, Mycobacterium fortuitum and Mycobacterium kansasii;
to eradicate Helicobacter pylori and reduce the frequency of relapses of duodenal ulcers.
Pharmacological effect
Pharmacological effect
Antibiotic of the macrolide group of the second generation with a broad spectrum of antimicrobial action. Has a bacteriostatic effect. Disturbs the protein synthesis of microorganisms – binds to the 50S subunit of the ribosomal membrane of the microbial cell.
Clarithromycin is active against Streptococcus agalactiae (Streptococcus pyogenes, Streptococcus viridans, Sreptococcus pneumoniae), Haemophilus influenzae (parainfluenzae), Haemophilus ducreyi, Neisseria gonorrhoeae, Neisseria meningitidis, Listeria monocytogenes, Legionella pneumophila, Mycoplasma pneumoniae, Helicobacter (Campilobacter) pylori, Campilobacter jejuni, Chlamidia pneumoniae (trachomatis), Moraxella (Branhamella) catarrhalis, Bordetella pertussis, Propionibacterium acnes, Staphylococcus aureus, Ureaplasma urealyticum, Toxoplasma gondii, Corynebacterium spp., Borrelia burgdorferi, Pasteurella multocida, some anaerobes (Eubacterium spp., Peptococcus spp., Propionibacterium spp., Clostridium perfringens, Bacteroides melaninogenicus) and all mycobacteria (including Mycobacterium avium, Mycobacterium leprae), except Mycobacterium tuberculosis.
Pharmacokinetics
Suction
After oral administration, absorption is rapid. Food slows absorption without significantly affecting bioavailability. The bioavailability of clarithromycin in suspension form is equivalent to or slightly higher than when taken in tablet form.
After a single dose, 2 Cmax peaks are recorded. The second peak is due to the ability of the drug to concentrate in the gallbladder, followed by gradual or rapid release. The time to reach Cmax when administered orally at a dose of 250 mg is 1-3 hours.
Distribution and metabolism
Plasma protein binding is more than 90%.
After oral administration, 20% of the dose taken is quickly hydroxylated in the liver with the participation of cytochrome P450 isoenzymes to form the main metabolite – 14-hydroxyclarithromycin, which has pronounced antimicrobial activity against Haemophilus influenzae.
With regular intake of 250 mg/day, the Css of the unchanged drug and its main metabolite are 1 and 0.6 μg/ml, respectively; T1/2 3-4 hours and 5-6 hours, respectively. When the dose is increased to 500 mg/day, Css of the unchanged drug and its metabolite in plasma is 2.7-2.9 and 0.83-0.88 mcg/ml, respectively; T1/2 – 4.8-5 hours and 6.9-8.7 hours, respectively. At therapeutic concentrations it accumulates in the lungs, skin and soft tissues (concentrations there are 10 times higher than the level in blood serum).
Removal
It is excreted by the kidneys and with feces (20-30% unchanged, the rest in the form of metabolites). With a single dose of 250 mg and 1.2 g, 37.9 and 46% are excreted in the urine, and 40.2 and 29.1% in feces, respectively.
Special instructions
Special instructions
In the presence of chronic liver diseases, it is necessary to regularly monitor the activity of liver enzymes.
Prescribed with caution while taking drugs metabolized in the liver; It is recommended to determine their concentration in blood plasma.
In case of combined use with warfarin or other indirect anticoagulants, it is necessary to monitor the prothrombin time.
If you have a history of heart disease, simultaneous use with terfenadine, cisapride, or astemizole is not recommended.
Attention should be paid to the possibility of cross-resistance between clarithromycin and other macrolide antibiotics, as well as lincomycin and clindamycin.
With prolonged or repeated use of the drug, the development of superinfection (growth of insensitive bacteria and fungi) is possible.
Active ingredient
Active ingredient
Clarithromycin
Composition
Composition
Each film-coated tablet contains:
Active ingredient: Clarithromycin – 500 mg.
Excipients: microcrystalline cellulose, corn starch, pregelatinized starch, polyvinylpyrrolidone, purified talc, sodium starch glycolate, colloidal silicon dioxide, stearic acid, magnesium stearate.
Shell composition: isopropyl alcohol, hydroxypropyl methylcellulose, titanium dioxide, purified talc, polyethylene glycol 6000, methylene chloride, lemon flavor, peppermint powder.
Pregnancy
Pregnancy
Use during pregnancy and breastfeeding
The safety of clarithromycin during pregnancy and lactation has not been established.
Therefore, during pregnancy, Klarbakt is prescribed only in the absence of alternative therapy, if the expected benefit outweighs the possible risk to the fetus.
Clarithromycin is excreted in breast milk, so the drug should be used with caution during lactation.
Use in children
For children, the drug is prescribed at a dose of 7.5 mg/kg body weight per day. The maximum daily dose is 500 mg. Duration of treatment is 7-10 days.
Contraindications
Contraindications
severe liver dysfunction;
severe renal dysfunction;
simultaneous use of ergot alkaloids;
simultaneous use of cisapride, pimozide, astemizole, terfenadine;
hypersensitivity to macrolide antibiotics.
Side Effects
Side Effects
From the digestive system: most often – nausea, dyspepsia, abdominal pain, vomiting and diarrhea; possible pseudomembranous colitis (from moderate to life-threatening), taste disturbances and a transient increase in the activity of liver enzymes, glossitis, stomatitis, candidiasis of the oral mucosa, change in the color of the tongue during treatment with clarithromycin, change in the color of teeth (in most cases reversible); rarely – hepatitis with an increase in the level of liver enzymes in the blood, the development of cholestasis and jaundice (these liver damage in some cases were severe and, as a rule, reversible); in isolated cases – liver failure with a fatal outcome.
From the central nervous system and peripheral nervous system: possible transient headache, dizziness, anxiety, fear, fear, insomnia, nightmares, tinnitus, confusion, disorientation, hallucinations, psychosis and depersonalization; rarely – paresthesia.
From the senses: possible hearing loss (recovered after discontinuation of the drug), changes in the perception of taste, as a rule, occurring together with a taste disorder.
From the cardiovascular system: rarely – increased QT interval, ventricular arrhythmia (including ventricular paroxysmal tachycardia, ventricular flutter or fibrillation).
From the urinary system: rarely – increased serum creatinine, interstitial nephritis, renal failure.
From the hematopoietic system: in some cases – thrombocytopenia, leukopenia.
Allergic reactions: if taken orally, urticaria, skin rash, anaphylactic reactions, Stevens-Johnson syndrome are possible.
Other: rarely – hypoglycemia (in some cases, while taking oral hypoglycemic agents or insulin).
Interaction
Interaction
With simultaneous use, clarithromycin increases the concentration in the blood of drugs metabolized in the liver with the participation of isoenzymes of the cytochrome P450 system: indirect anticoagulants, carbamazepine, theophylline, triazolam, midazolam, cyclosporine, disopyramide, phenytoin, rifabutin, lovastatin, digoxin, ergot alkaloids.
When used simultaneously with clarithromycin, there is a significant increase in the concentration of cisapride, pimozide, astemizole and terfenadine (2-3 times) in the blood plasma, which may prolong the QT interval and develop cardiac arrhythmias, including ventricular paroxysmal tachycardia, ventricular fibrillation and ventricular flutter or fibrillation (this combination is contraindicated).
Rare cases of acute necrosis of skeletal muscles have been reported, coinciding with the simultaneous administration of clarithromycin and HMG-CoA reductase inhibitors – lovastatin and simvastatin.
There are reports of increased concentrations of digoxin in the plasma of patients receiving simultaneously digoxin and clarithromycin tablets. In such patients, it is necessary to constantly monitor the level of digoxin in the serum to avoid digitalis intoxication.
Clarithromycin may decrease the clearance of triazolam and thus increase its pharmacological effects resulting in drowsiness and confusion.
Concomitant use of clarithromycin and ergotamine (ergot alkaloids) can lead to acute ergotamine intoxication, manifested by severe peripheral vasospasm and sensory disturbances.
Concomitant administration of oral zidovudine and clarithromycin tablets to HIV-infected adults may result in a decrease in the Css of zidovudine. Given that clarithromycin is likely to alter the absorption of concomitantly administered oral zidovudine, this interaction can be largely avoided by taking clarithromycin and zidovudine at different times of the day (at least 4 hours apart).
With the simultaneous administration of clarithromycin and ritonavir, the serum concentrations of clarithromycin increase. No dose adjustment of clarithromycin is required in these cases for patients with normal renal function. However, in patients with creatinine clearance from 30 to 60 ml/min, the dose of clarithromycin should be reduced by 50%. When CC is less than 30 ml/min, the dose of clarithromycin should be reduced by 75%. During concomitant treatment with ritonavir, clarithromycin should not be prescribed in doses greater than 1 g/day.
Overdose
Overdose
Symptoms: nausea, vomiting, diarrhea, headache, confusion.
Treatment: immediate gastric lavage and symptomatic treatment are necessary. Hemodialysis and peritoneal dialysis do not lead to a significant change in clarithromycin serum levels.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
2 years
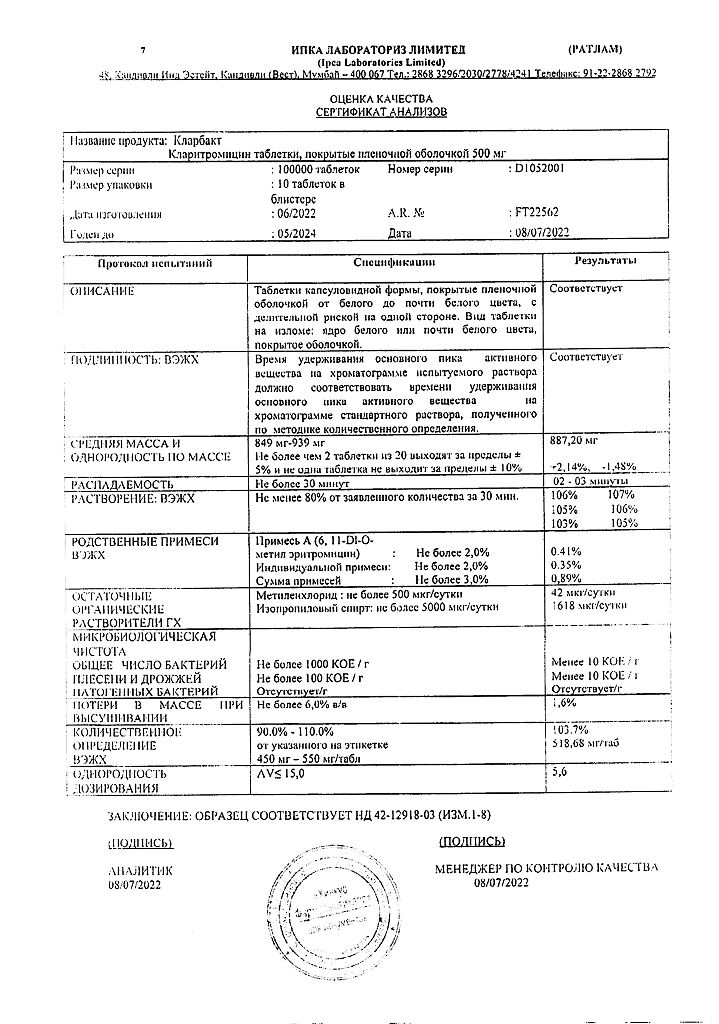
Manufacturer
Manufacturer
Ipka Laboratories Limited, India
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | Ipka Laboratories Limited, India |
| Medication form | pills |
| Brand | Ipka Laboratories Limited |
Related products
Buy Clarbact, 500 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.