No products in the cart.
Claira, 2 mg+2 mg, 3 mg+2 mg and 1 mg, 3 mg 84 pcs
€94.17 €78.47
EAN: 4029668001835
SKU: 219123
Categories: Contraceptive, Gynecology and Obstetrics, Hormonal, Medicine
Description
Pharmacotherapeutic group
Combination contraceptive (estrogen + gestagen)
ATX code
G03AB
Pharmacological properties
The contraceptive effect of combined oral contraceptives (OCs) is based on the interaction of various factors, the most important of which are ovulation suppression and changes in the properties of cervical mucus. Besides prevention of unwanted pregnancy, OCs have a number of positive characteristics that, when taken together with their negative characteristics (see “Special considerations,” “Side effects”), may help in choosing the most appropriate method of contraception. In women taking OCs the painfulness and intensity of menstrual bleeding decreases, thus reducing the risk of iron deficiency anemia. Besides, there is data on reduction of risk of endometrial and ovarian cancer development.
The estrogen in Klyra preparation is estradiol valerate, a precursor of natural human 17β-estradiol (1 mg of estradiol valerate corresponds to 0,76 mg of 17β-estradiol) The estrogen component used in this OC, thus, differs from estrogens usually used in OCs which are synthetic estrogens ethinyl estradiol or its precursor mestranol, both containing an ethynyl group in position 17α. This group causes higher metabolic stability, but also more expressed action on the liver.
Administration of Claira leads to a less pronounced effect on the liver compared to triphasic OCs containing ethinylestradiol and levonorgestrel. It was shown that the effect on the concentration of globulin binding sex steroids (GSSB) and hemostasis parameters is less pronounced. In combination with dienogestrel, estradiol valerate shows an increase in high-density lipoproteins (HDL), while the concentration of low-density lipoprotein cholesterol (LDL) decreases slightly.
Dienogest is an oral progestagen characterized by additional partial antiandrogenic effects. Its estrogenic, anti-estrogenic and androgenic properties are insignificant. Due to its special chemical structure a spectrum of pharmacological action is provided which combines the most important advantages of 19-nor-progestagens and progesterone derivatives.
Indications
Indications
Oral contraception.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Combined contraceptive (estrogen + gestagen)
ATX code
G03AB
Pharmacological properties
The contraceptive effect of combined oral contraceptives (COCs) is based on the interaction of various factors, the most important of which are suppression of ovulation and changes in the properties of cervical mucus. Along with the prevention of unwanted pregnancy, COCs have a number of positive properties, which, when also taking into account the negative properties (see “Special instructions”, “Side effects”), can help in choosing the most suitable method of contraception. In women taking COCs, the pain and intensity of menstrual-like bleeding decreases, resulting in a reduced risk of iron deficiency anemia. In addition, there is evidence of a reduced risk of endometrial and ovarian cancer.
The estrogen in Qlaira is estradiol valerate, a precursor to naturally occurring human 17β-estradiol (1 mg estradiol valerate corresponds to 0.76 mg 17β-estradiol). The estrogen component used in this COC is therefore different from the estrogens commonly used in COCs, which are the synthetic estrogens ethinyl estradiol or its precursor mestranol, both containing ethynyl group at position 17α. This group causes higher metabolic stability, but also a more pronounced effect on the liver.
Taking Qlaira leads to a less pronounced effect on the liver compared to triphasic COCs containing ethinyl estradiol and levonorgestrel. The effect on sex steroid binding globulin (SHBG) concentrations and hemostatic parameters has been shown to be less pronounced. In combination with dienogest, estradiol valerate demonstrates an increase in high-density lipoprotein (HDL) cholesterol, while low-density lipoprotein (LDL) cholesterol concentrations are slightly reduced.
Dienogest is an orally active progestogen that is characterized by additional partial antiandrogenic effects. Its estrogenic, antiestrogenic and androgenic properties are negligible. Thanks to the special chemical structure, a spectrum of pharmacological action is provided that combines the most important advantages of 19-nor-progestogens and progesterone derivatives.
Special instructions
Special instructions
If any of the diseases/conditions/risk factors listed below currently exist, the potential risk and expected benefits of using Qlaira® should be carefully weighed in each individual case and discussed with the woman before she decides to start taking the drug. If any of these conditions or risk factors worsen, intensify, or appear for the first time, a woman should consult her doctor, who may decide whether to discontinue the drug.
Diseases of the cardiovascular system
The results of epidemiological studies indicate a relationship between the use of COCs and an increased incidence of venous and arterial thrombosis and thromboembolism (such as DVT, PE, MI and cerebrovascular events). The risk of developing venous thromboembolism (VTE) is greatest in the first year of taking such drugs, mainly during the first 3 months. An increased risk is present after initial use of a COC or resumption of use of the same or different COCs (after a dosing interval of 4 weeks or more). The overall risk of VTE in patients taking low-dose COCs (ethinyl estradiol content less than 50 mcg) is 2-3 times higher than in patients who do not take COCs, however, this risk remains lower than the risk of VTE during pregnancy and childbirth. VTE can be fatal (in 1–2% of cases).
VTE, manifested as DVT or PE, can occur while using any COC. It is extremely rare when using COCs that thrombosis of other blood vessels occurs, such as hepatic, mesenteric, renal, cerebral arteries and veins or retinal vessels. There is no consensus regarding the relationship between the occurrence of these events and the use of CCPs. Arterial thromboembolism can be fatal.
The risk of developing thrombosis (venous and/or arterial) and thromboembolism increases:
– with age;
– in smokers (with an increase in the number of cigarettes smoked or an increase in age, the risk increases, especially in women over 35 years of age);
if available:
– family history (for example, venous or arterial thromboembolism ever in close relatives or parents at a relatively young age). In the case of a hereditary or acquired predisposition, the woman should be examined by an appropriate specialist to decide on the possibility of taking Qlaira®;
– obesity (body mass index more than 30 kg/m2);
– dislipoproteinemia;
– arterial hypertension;
– migraine;
– diseases of the heart valves;
– atrial fibrillation;
– prolonged immobilization; major surgery, any operation on the lower extremities or major trauma. In such situations, it is advisable to stop taking Qlaira® (for planned surgery – at least 4 weeks before it) and not resume taking it for 2 weeks after the end of immobilization.
The possible role of varicose veins and superficial thrombophlebitis in the development of VTE remains controversial.
The increased risk of thromboembolism in the postpartum period should be taken into account. Peripheral circulatory disorders may also occur in diabetes mellitus, systemic lupus erythematosus, hemolytic uremic syndrome, chronic inflammatory bowel disease (Crohn’s disease or ulcerative colitis) and sickle cell anemia. An increase in the frequency and severity of migraines while using Qlaira® (which may precede cerebrovascular events) may be grounds for immediate discontinuation of this drug.
Biochemical factors indicating a hereditary or acquired predisposition to arterial or venous thrombosis include the following: resistance to activated protein C, hyperhomocysteinemia, antithrombin III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipid antibodies, lupus anticoagulant).
When assessing the risk-benefit ratio, it should be taken into account that treatment of the relevant condition may reduce the associated risk of thrombosis. It should also be taken into account that the risk of thrombosis and thromboembolism during pregnancy is higher than when taking low-dose oral contraceptives (ethinyl estradiol content less than 50 mcg).
Tumors
The most significant risk factor associated with the development of cervical cancer is persistent human papillomavirus infection (PVI). There are reports of a slight increase in the risk of advanced cervical cancer with long-term use of COCs. The connection with the use of COCs has not been proven. The possibility of the relationship of these data with screening for cervical diseases and characteristics of sexual behavior (less frequent use of barrier methods of contraception) is discussed.
A meta-analysis of 54 epidemiological studies found a small increase in the relative risk (RR = 1.24) of developing breast cancer in women currently taking COCs. The increased risk gradually disappears within 10 years of stopping these drugs. Because breast cancer is rare in women under 40 years of age, the slight increase in breast cancer diagnoses in women who are currently or recently taking COCs is small relative to the overall risk of breast cancer. Its connection with the use of COCs has not been proven. The observed increased risk may also be a consequence of earlier diagnosis of breast cancer in women using COCs. Women who have ever used COCs are diagnosed with earlier stages of breast cancer than women who have never used them.
In rare cases, during the use of COCs, the development of benign, and in extremely rare cases, malignant liver tumors, which in some cases led to life-threatening intra-abdominal bleeding, was observed. If severe pain in the upper abdomen, an increase in liver size, or signs of intra-abdominal bleeding occur in women taking COCs, liver tumors must be excluded in the differential diagnosis.
Other states
Women with hypertriglyceridemia (or a family history of this condition) may have an increased risk of developing pancreatitis while taking COCs.
Although slight increases in blood pressure have been described in many women taking COCs, clinically significant increases have rarely been reported. However, if a persistent, clinically significant increase in blood pressure develops while taking Qlaira®, the drug should be discontinued and treatment of arterial hypertension should be started. Taking Qlaira® can be resumed if necessary if normal blood pressure levels are achieved through antihypertensive therapy.
The following conditions develop or worsen both during pregnancy and when taking COCs, but their relationship with taking COCs has not been proven: jaundice and/or cholestatic pruritus, cholelithiasis, porphyria, systemic lupus erythematosus, hemolytic-uremic syndrome, Sydenham’s chorea, herpes of pregnancy, hearing loss due to otosclerosis.
In women with hereditary forms of angioedema, exogenous estrogens may induce or worsen symptoms of angioedema.
Acute or chronic liver dysfunction may require discontinuation of Qlaira® until liver function tests return to normal. Recurrent cholestatic jaundice, which develops for the first time during pregnancy or previous use of sex hormones, requires discontinuation of the drug Qlaira®.
Although COCs may have an effect on insulin resistance and glucose tolerance, there is no need to change the therapeutic regimen in diabetic patients using Qlaira®. However, women with diabetes need careful monitoring while taking Qlaira®.
Cases of Crohn’s disease and ulcerative colitis have also been described with the use of COCs.
Chloasma can sometimes develop, especially in women with a history of chloasma during pregnancy.
Women prone to developing chloasma should avoid exposure to the sun or UV radiation while taking Qlaira®.
Effect on laboratory tests. Taking Qlaira® may affect the results of some laboratory tests, including biochemical parameters of liver, thyroid, adrenal and kidney function, plasma concentrations of transport proteins, such as DSG and lipid/lipoprotein fractions, parameters of carbohydrate metabolism, coagulation and fibrinolysis. These changes usually remain within laboratory limits.
Medical examinations. Before starting to use the drug Qlaira®, it is necessary to carefully evaluate contraindications to the drug’s use based on the woman’s life history, family history, as well as general medical and gynecological examination. The frequency and nature of these examinations should be based on existing standards of medical practice, with due consideration for the individual characteristics of each patient. As a rule, blood pressure is measured, the condition of the mammary glands, abdominal cavity and pelvic organs is checked, including cervical cytology.
It is necessary to explain to women that Qlaira® does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Reduced efficiency. The effectiveness of Qlaira® may be reduced if tablets with active ingredients are missed (see recommendations for taking missed tablets in the “Dosage and Administration” section), gastrointestinal disorders while taking tablets with active ingredients (see recommendations for gastrointestinal disorders in the “Dosage and Administration” section) or against the background of concomitant drug treatment (see “Interactions”).
Insufficient control of the menstrual cycle. While using the drug Qlaira®, especially in the first months of use, irregular menstrual-like bleeding (spotting or breakthrough uterine bleeding) may occur. Therefore, evaluation of any irregular menstrual-like bleeding should be carried out only after an adaptation period of approximately 3 menstrual-like cycles.
If irregular menstrual-like bleeding recurs or occurs for the first time after previous regular cycles, the possibility of non-hormonal causes should also be considered and a thorough examination should be performed to rule out malignancy or pregnancy. Such measures may include diagnostic curettage.
Some women may not develop menstrual bleeding while taking inactive white tablets. If the drug Qlaira® was taken in accordance with the rules specified in the section “Method of administration and dosage”, pregnancy is unlikely. However, if before the first absent menstrual-like bleeding the tablets were taken irregularly or there are no 2 menstrual-like bleedings in a row, you should not continue to use the drug Qlaira until pregnancy has been ruled out.
Impact on the ability to drive a car or perform work that requires increased speed of physical and mental reactions. There was no negative effect of the drug Qlaira® on the ability to drive a car or operate machinery, however, patients who experience episodes of dizziness and impaired concentration during the adaptation period (the first 3 months of taking the drug) should be careful.
Active ingredient
Active ingredient
Dienogest, Estradiol valerate and Estradiol valerate [set]
Composition
Composition
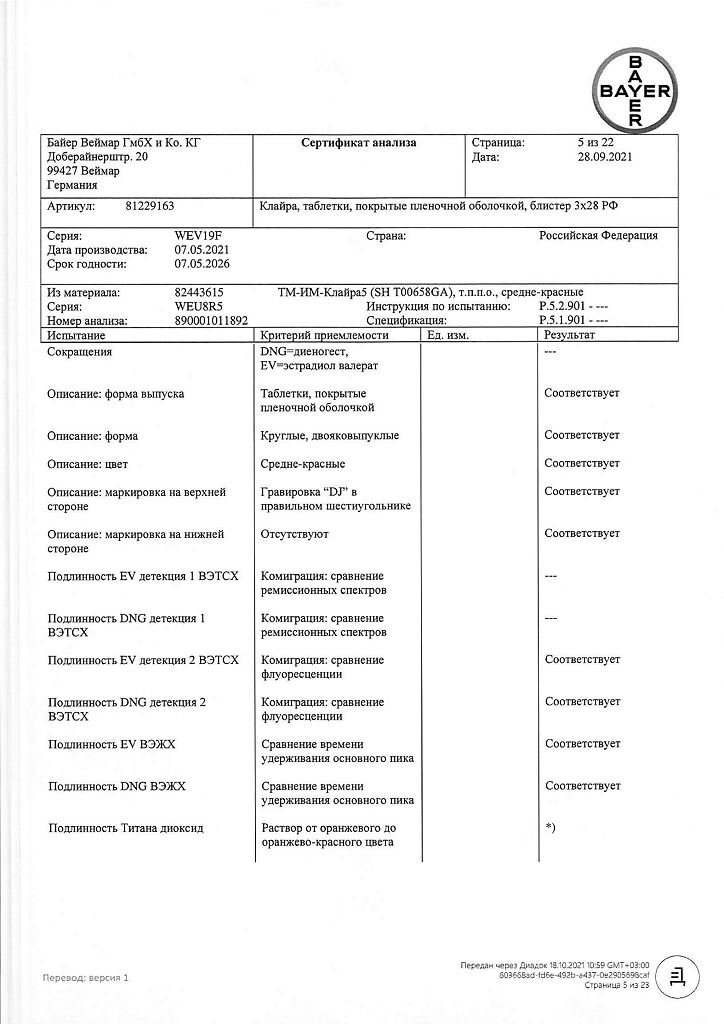
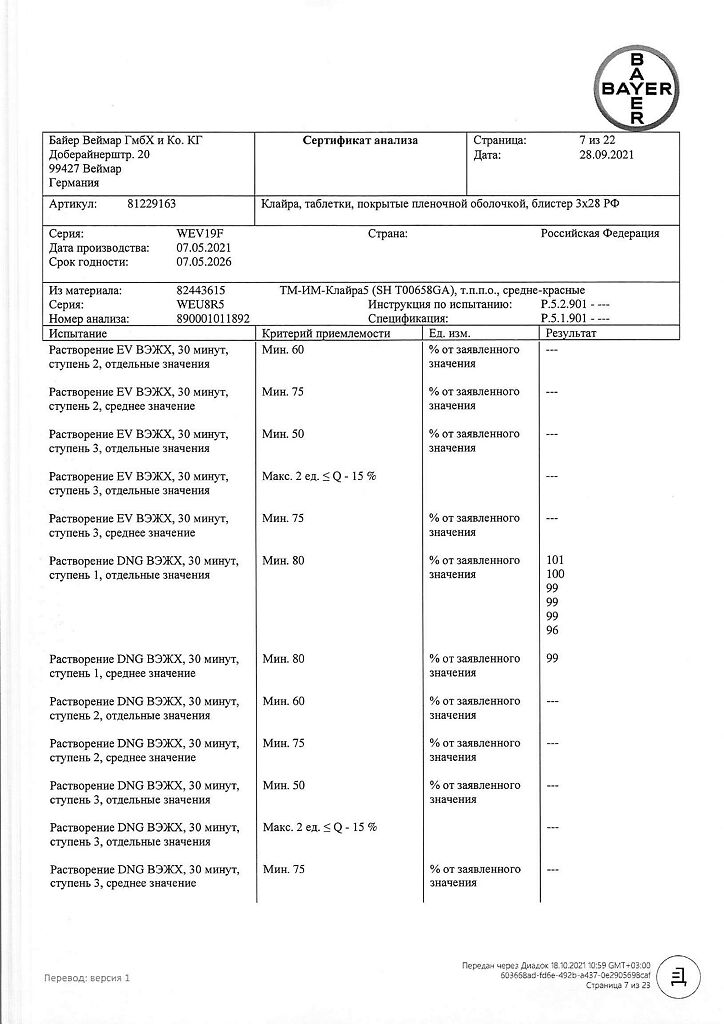
For one pink film-coated tablet:
Active components: Estradiol valerate, micro 20 – 2,000 mg Dienogest, micro – 2,000 mg,
Auxiliary components: lactose monohydrate, corn starch, pregelatinized corn starch, povidone-25, magnesium stearate
Shell: hypromellose, macrogol-6000, talc, titanium dioxide, red iron oxide dye.
For one pale yellow film-coated tablet:
Active components: estradiol valerate, micro 20 – 2,000 mg Dienogest, micro – 3,000 mg
Auxiliary components: lactose monohydrate, corn starch, pregelatinized corn starch, povidone-25, magnesium stearate
Shell: hypromellose, macrogol-6000, talc, titanium dioxide, yellow iron oxide dye.
For one red film-coated tablet:
Active ingredient: estradiol valerate, micro 20 – 1,000 mg
Auxiliary components: lactose monohydrate, corn starch, pregelatinized corn starch, povidone-25, magnesium stearate
Shell: hypromellose, macrogol-6000, talc, titanium dioxide, red iron oxide dye.
Contraindications
Contraindications
Qlaira® should not be used if any of the conditions listed below are present. The drug should be discontinued immediately if any of these conditions develop for the first time while taking it:
hypersensitivity to the active substances or any of the excipients;
thrombosis (venous and arterial) and thromboembolism currently or in history (including deep vein thrombosis (DVT), pulmonary embolism (PE), myocardial infarction (MI), stroke currently or in history);
conditions preceding thrombosis (including transient ischemic attacks, angina) currently or in history;
identified acquired or hereditary predisposition to venous or arterial thrombosis, including resistance to activated protein C, antithrombin III deficiency, protein C deficiency, protein S deficiency, hyperhomocyssinemia, antibodies to phospholipids (anticardiolipin antibodies, lupus anticoagulant);
presence of a high risk of venous or arterial thrombosis (see “Special Instructions”);
migraine with focal neurological symptoms, incl. in the anamnesis;
diabetes mellitus with vascular complications;
pancreatitis with severe hypertriglyceridemia currently or in history;
liver failure and severe liver diseases (until normalization of liver function indicators);
liver tumors (benign and malignant) currently or in history;
identified hormone-dependent malignant tumors (including genital organs or mammary glands) or suspicion of them;
bleeding from the vagina of unknown origin;
pregnancy or suspicion of it;
breastfeeding period;
lactose intolerance, lactase deficiency, glucose-galactose malabsorption.
WITH CAUTION
If any of the diseases/conditions/risk factors listed below currently exist, then the potential risk and expected benefit of using Qlaira® should be carefully weighed in each individual case:
risk factors for the development of thrombosis and thromboembolism (smoking; obesity; dyslipoproteinemia; arterial hypertension; migraine; heart valve disease; cardiac arrhythmia; extensive surgical interventions without prolonged immobilization);
other diseases in which peripheral circulatory disorders may occur (diabetes mellitus, systemic lupus erythematosus, hemolytic-uremic syndrome, Crohn’s disease and ulcerative colitis, sickle cell anemia);
hereditary angioedema;
hypertriglyceridemia;
diseases that first appeared or worsened during pregnancy or against the background of previous use of sex hormones (for example, cholestatic jaundice, cholestatic itching, cholelithiasis, otosclerosis with hearing impairment, porphyria, pregnancy herpes, Sydenham’s chorea);
postpartum period.
Side Effects
Side Effects
System-organ class
Often
Uncommon
Rarely
Infections and infestations
Fungal infection, vaginal candidiasis, unspecified vaginal infection
Candidiasis, herpes, presumptive ocular histoplasmosis syndrome, lichen versicolor, urinary tract infection, bacterial vaginosis, vulvovaginal candidiasis
Metabolism and nutritional disorders
Increased appetite
Fluid retention, hypertriglyceridemia
Nervous system
Headache (including tension headache)
Depression/low mood, decreased libido, mental disorder, mood changes, dizziness
Affective lability, aggressiveness, anxiety, dysphoria, increased libido, nervousness, restlessness, sleep disturbance, stress, impaired attention, paresthesia, vertigo
Organ of vision
Contact lens intolerance, dry eye mucosa, eyelid swelling
Cardiovascular system
Increased blood pressure, migraine (including with and without aura)
Bleeding from varicose veins, hot flashes to the face, decreased blood pressure, pain along the veins
From the gastrointestinal tract
Abdominal pain (including bloating)
Diarrhea, nausea, vomiting
Constipation, dyspepsia, gastroesophageal reflux
From the liver and biliary tract
Increased ALT activity, focal nodular hyperplasia of the liver
From the skin and subcutaneous tissues
Acne
Alopecia, pruritus (including generalized pruritus and pruritic rash), rash (including macular rash), hyperhidrosis
Allergic skin reaction, including allergic dermatitis and urticaria, chloasma, dermatitis, hirsutism, hypertrichosis, neurodermatitis, pigmentation disorder, seborrhea, unspecified skin lesion
From the musculoskeletal and connective tissue side
Back pain, muscle spasms, feeling of heaviness
From the genital organs and breast
Absence of menstrual-like bleeding, discomfort in the mammary glands, pain in the mammary glands, sore nipples, pain in the nipples, painful menstrual-like bleeding, irregular menstrual-like bleeding (metrorrhagia)
Breast enlargement, diffuse thickening of the mammary glands, cervical epithelial dysplasia, dysfunctional uterine bleeding, dyspareunia, fibrocystic mastopathy, menorrhagia, ovarian cysts, pelvic pain, premenstrual syndrome, uterine leiomyoma, uterine cramps, vaginal discharge, vulvovaginal dryness
Benign neoplasm in the mammary gland, breast cyst, bleeding during sexual intercourse, galactorrhea, vaginal bleeding, hypomenorrhea, delayed menstrual bleeding, rupture of an ovarian cyst, burning sensation in the vagina, uterine/vaginal bleeding (including spotting, vaginal odor, vulvovaginal discomfort)
From the blood and lymphatic system
Lymphadenopathy
General symptoms
Weight gain
Irritability, swelling, weight loss
Chest pain, fatigue, malaise
The following serious adverse events have been reported in women using COCs (which include Qlaira®): arterial and venous thrombosis and thromboembolic complications; worsening or provoking symptoms of angioedema; liver tumors; acute pancreatitis
Interaction
Interaction
The influence of other drugs on the active components of the drug Qlaira®
The interaction of COCs with other drugs may lead to breakthrough uterine bleeding and/or lack of contraceptive effect. The following types of interactions have been described in the literature on COCs in general or studied during clinical trials of Qlaira®:
Isoenzyme inducers (CYP3A4 isoenzyme). There may be an interaction with drugs that induce microsomal enzymes (for example, cytochrome P450 systems), as a result of which the clearance of sex hormones can increase (such drugs include phenytoin, barbiturates, primidone, carbamazepine, rifampicin and possibly also oxcarbazepine, topiramate, felbamate, ritonavir, griseofulvin, as well as drugs containing St. John’s wort perforated). It has been reported that HIV protease inhibitors (eg ritonavir), non-nucleoside reverse transcriptase inhibitors (eg nevirapine) and combinations thereof may also have an effect on hepatic metabolism.
Effect on enterohepatic recirculation. When taking certain groups of antibiotics (for example, penicillin and tetracycline groups), the enterohepatic circulation of estrogen may decrease, which can lead to a decrease in the concentration of estradiol.
Women who are treated with microsomal enzyme-inducing drugs or antibiotics are advised to temporarily use a barrier method of contraception or choose another method of contraception in addition to Qlaira®. The barrier method of contraception should be used during the entire period of taking concomitant medications and for another 28 days after their discontinuation.
Isoenzyme inhibitors (CYP3A4 isoenzyme). Co-administration of rifampicin with tablets containing estradiol valerate and dienogest resulted in a significant reduction in Css and systemic exposure of dienogest and estradiol. Systemic exposure of dienogest and estradiol at Css, measured based on AUC0–24, decreased by 83 and 44%, respectively.
Known inhibitors of CYP3A4, such as azole antifungals, cimetidine, verapamil, macrolides, diltiazem, antidepressants and grapefruit juice, may increase plasma concentrations of dienogest. When administered concomitantly with the potent inhibitor ketoconazole, the AUC0–24 value at steady state increased for dienogest by 186%, and for estradiol by 57%. When administered concomitantly with the moderate inhibitor erythromycin, the AUC0–24 value of dienogest and estradiol at steady state increased by 62 and 33%, respectively.
Effects of Qlaira® in relation to other drugs: COCs can affect the metabolism of a number of other drugs (for example, lamotrigine), which can lead to either an increase or decrease in the concentration of these substances in the blood plasma and tissues. However, based on data from in vitro studies, inhibition of CYP enzymes when using Qlaira® at a therapeutic dose is unlikely.
Note: to identify possible interactions, you should read the instructions for accompanying drugs.
Incompatibility. Absent.
Overdose
Overdose
Symptoms: no serious problems have been reported following an overdose of Qlaira®. Based on the overall experience of using COCs, the symptoms that may occur with an overdose of active tablets: nausea, vomiting, spotting or metrorrhagia.
Treatment: symptomatic.
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C
Shelf life
Shelf life
4 years
Manufacturer
Manufacturer
Bayer Bitterfeld GmbH, Germany
Additional information
| Shelf life | 4 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Bayer Bitterfeld GmbH, Germany |
| Medication form | tablet set |
| Brand | Bayer Bitterfeld GmbH |
Other forms…
Related products
Gynecology and Obstetrics
Gynecology and Obstetrics
Gynecology and Obstetrics
Prepidil, intracervical gel 0.5 mg/3 g syringes with catheter
Buy Claira, 2 mg+2 mg, 3 mg+2 mg and 1 mg, 3 mg 84 pcs with delivery to USA, UK, Europe and over 120 other countries.