No products in the cart.
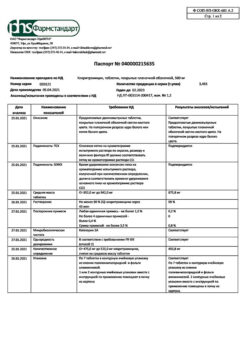
Clacid, 250 mg/5 ml 49.5 g 1 ml
€27.55 €23.87
Out of stock
(E-mail when Stock is available)
Description
– Infectious and inflammatory diseases caused by microorganisms sensitive to clarithromycin: Lower respiratory tract infections (such as bronchitis, pneumonia);
– Upper respiratory tract infections (such as pharyngitis, sinusitis);
– Skin and soft tissue infections (such as folliculitis, subcutaneous tissue inflammation, rye);
– disseminated or localized mycobacterial infections caused by Mycobacterium avium and Mycobacterium intracellulare;
– localized infections caused by Mycobacterium chelonae, Mycobacterium fortuitum and Mycobacterium kansasii;
– acute otitis media.
Indications
Indications
– infectious and inflammatory diseases caused by microorganisms sensitive to clarithromycin: lower respiratory tract infections (such as bronchitis, pneumonia);
– upper respiratory tract infections (such as pharyngitis, sinusitis);
– infections of the skin and soft tissues (such as folliculitis, inflammation of the subcutaneous tissue, erysipelas);
– disseminated or localized mycobacterial infections caused by Mycobacterium avium and Mycobacterium intracellulare;
– localized infections caused by Mycobacterium chelonae, Mycobacterium fortuitum and Mycobacterium kansasii;
– acute otitis media.
Pharmacological effect
Pharmacological effect
Bacteriostatic, antibacterial.
Pharmacokinetics
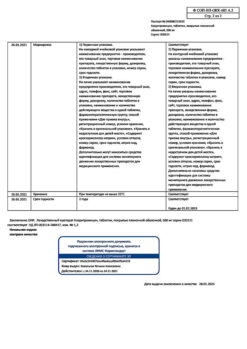
Special instructions
Special instructions
In the presence of chronic liver diseases, it is necessary to regularly monitor serum enzymes.
Prescribe with caution against drugs metabolized by the liver.
In case of co-administration with warfarin or other indirect anticoagulants, PT must be monitored.
In children, it is preferable to use Klacid in powder dosage form for the preparation of an oral suspension of 125 mg/5 ml and 250 mg/5 ml.
Active ingredient
Active ingredient
Clarithromycin
Composition
Composition
5 ml of ready-made suspension:
Active substances:
clarithromycin 250 mg
Excipients:
carbomer (carbopol 974P) – 150 mg,
povidone K90 – 35 mg,
hypromellose phthalate – 304.2 mg,
castor oil – 32.1 mg,
silicon dioxide – 10 mg,
maltodextrin – 238.7 mg,
sucrose – 2276.2 mg,
titanium dioxide – 35.7 mg,
xanthan gum – 3.8 mg,
fruit flavoring – 35.7 mg,
potassium sorbate – 20 mg,
citric acid – 4.24 mg.
Pregnancy
Pregnancy
The use of clarithromycin during pregnancy (especially in the first trimester) is possible only in the absence of alternative therapy, and the potential benefit to the mother outweighs the potential risk to the fetus. Clarithromycin is excreted in breast milk.
If it is necessary to take it during lactation, breastfeeding should be stopped.
Contraindications
Contraindications
– hypersensitivity to the components of the drug and other macrolides;
– simultaneous use of clarithromycin with the following drugs: astemizole, cisapride, pimozide, terfenadine; simultaneous use of clarithromycin with ergot alkaloids, for example, ergotamine, dihydroergotamine;
– simultaneous use of clarithromycin with midazolam for oral administration; patients with a history of QT prolongation, ventricular arrhythmia, or torsade de pointes;
– patients with hypokalemia (risk of QT interval prolongation); patients with severe liver failure occurring simultaneously with renal failure;
– simultaneous use of clarithromycin with HMG-CoA reductase inhibitors (statins), which are largely metabolized by the CYP3A4 isoenzyme (lovastatin, simvastatin), due to an increased risk of myopathy, including rhabdomyolysis;
– simultaneous use of clarithromycin with colchicine in patients with impaired liver or kidney function;
– patients with a history of cholestatic jaundice/hepatitis that developed while using clarithromycin;
– porphyria;
– period of breastfeeding;
– patients with congenital fructose intolerance, sucrase-isomaltase deficiency, glucose-galactose malabsorption syndrome.
With caution: moderate to severe renal failure; moderate to severe liver failure; myasthenia gravis (possible increased symptoms); simultaneous use of clarithromycin with benzodiazepines, such as alprazolam, triazolam, midazolam for intravenous use; simultaneous use with drugs that are metabolized by the CYP3A isoenzyme, for example, carbamazepine, cilostazol, cyclosporine, disopyramide, methylprednisolone, omeprazole, indirect anticoagulants (for example, warfarin), quinidine, rifabutin, sildenafil, tacrolimus, vinblastine; simultaneous use with drugs that induce the CYP3A4 isoenzyme, for example, rifampicin, phenytoin, carbamazepine, phenobarbital, St. John’s wort; simultaneous use with calcium channel blockers that are metabolized by the CYP3A4 isoenzyme (for example, verapamil, amlodipine, diltiazem); patients with coronary heart disease (CHD), severe heart failure, hypomagnesemia, severe bradycardia (less than 50 beats/min), as well as patients simultaneously taking class IA (quinidine, procainamide) and class III antiarrhythmic drugs (dofetilide, amiodarone, sotalol); pregnancy; diabetes mellitus (the drug contains sucrose).
Side Effects
Side Effects
The most common adverse events were from the gastrointestinal tract, incl. diarrhea, vomiting, abdominal pain and nausea. Other adverse reactions included headache, taste disturbances, and transient increases in liver enzymes.
Post-marketing experience
During treatment with clarithromycin, liver dysfunction, including increased liver enzymes, and hepatocellular and/or cholestatic hepatitis, with or without jaundice, has been reported infrequently. Hepatic dysfunction can be severe and is usually reversible. In very rare cases, deaths from liver failure have been reported, which were usually observed in the presence of serious concomitant diseases and/or concomitant use of other drugs.
Isolated cases of increased serum creatinine levels have been described, but their connection with the drug has not been established.
Allergic reactions have been reported with oral administration of clarithromycin, ranging from urticaria and minor rashes to anaphylaxis and Stevens-Johnson syndrome/toxic epidermal necrolysis.
There have been reports of transient CNS effects including dizziness, anxiety, insomnia, nightmares, tinnitus, confusion, disorientation, hallucinations, psychosis and depersonalization; their cause-and-effect relationship with the drug has not been established.
Cases of hearing loss have been reported during treatment with clarithromycin; after cessation of treatment, hearing was usually restored. There are also cases of disturbances in the sense of smell, which are usually combined with a perversion of taste.
Glossitis, stomatitis, oral thrush and discoloration of the tongue have been described during treatment with clarithromycin. There are known cases of tooth discoloration in patients treated with clarithromycin. These changes are usually reversible and can be corrected by your dentist.
Rare cases of hypoglycemia have been described, some of which were observed in patients receiving oral hypoglycemic agents or insulin.
Isolated cases of leukopenia and thrombocytopenia have been reported.
When treating with clarithromycin, as with other macrolides, prolongation of the QT interval, ventricular tachycardia and torsade de pointes (TdP) have been observed in rare cases.
Rare cases of pancreatitis and seizures have been described.
There are reports of the development of interstitial nephritis during treatment with clarithromycin.
In clinical practice, cases of toxicity of colchicine when combined with clarithromycin have been described, especially in elderly people. Some of them were observed in patients with renal failure; Several deaths have been reported in similar patients.
Children with suppressed immune systems
In patients with AIDS and other immunodeficiencies receiving clarithromycin in higher doses over a long period of time for the treatment of mycobacterial infections, it is often difficult to differentiate the undesirable effects of the drug from symptoms of HIV infection or intercurrent illnesses.
The main adverse events in patients taking clarithromycin orally at a dose of 1 g were nausea, vomiting, taste disturbance, abdominal pain, diarrhea, rash, bloating, headache, hearing loss, constipation, increased AST and ALT levels. Dyspnea, insomnia, and dry mouth were also reported less frequently.
In this group of patients with suppressed immunity, significant deviations of laboratory parameters from normative values in specific tests (sharp increase or decrease) were recorded.
Based on this, approximately 2–3% of patients taking clarithromycin orally at a dose of 1 g/day had significant laboratory abnormalities, such as increased AST, ALT levels and decreased white blood cell and platelet counts. Fewer patients also experienced elevated blood urea nitrogen levels.
Interaction
Interaction
Interaction with cytochrome P450
Clarithromycin is metabolized in the liver by the cytochrome P4503A isoenzyme (CYP3A). This mechanism determines many interactions with other drugs. Clarithromycin may inhibit the biotransformation of other drugs by this system, which may result in increased serum levels.
The following drugs or classes are known or suspected to be metabolized by the same CYP3A isoenzyme: alprazolam, astemizole, carbamazepine, cilostazol, cisapride, cyclosporine, disopyramide, ergot alkaloids, lovastatin, methylprednisolone, midazolam, omeprazole, oral anticoagulants (e.g. warfarin), pimozide, quinidine, rifabutin, sildenafil, simvastatin, tacrolimus, terfenadine, triazolam and vinblastine.
Similar mechanisms of interaction, which are mediated by other cytochrome P450 isoenzymes, are characteristic of phenytoin, theophylline and valproic acid. In clinical studies, there was a small but statistically significant (p) difference when combining theophylline or carbamazepine with clarithromycin.
In clinical practice, the following CYP3A-mediated interactions have been reported with the use of erythromycin and/or clarithromycin.
When clarithromycin was combined with HMG-CoA reductase inhibitors, such as lovastatin and simvastatin, rhabdomyolysis developed in rare cases.
With simultaneous use of clarithromycin with cisapride, an increase in the levels of the latter was observed. This may lead to prolongation of the QT interval and the development of cardiac arrhythmias, including ventricular tachycardia, ventricular fibrillation, and torsade de pointes (TdP). Similar effects have been reported in patients receiving clarithromycin with pimozide.
Macrolides caused disruption of the metabolism of terfenadine, which led to an increase in its plasma levels and was sometimes associated with the development of arrhythmias, incl. prolongation of the QT interval, ventricular tachycardia, ventricular fibrillation and torsade de pointes (TdP).
In one study of 14 healthy volunteers, the combined use of clarithromycin tablets and terfenadine resulted in a 2- to 3-fold increase in serum levels of the acid metabolite terfenadine and a prolongation of the QT interval, which was not associated with any clinical effects.
In clinical practice, cases of ventricular tachycardia of the “pirouette” type have been reported when clarithromycin is combined with quinidine or disopyramide. Serum levels of these drugs should be monitored during treatment with clarithromycin.
Ergotamine/dihydroergotamine. In clinical practice, when clarithromycin was combined with ergotamine or dihydroergotamine, cases of acute toxicity of the latter, which is characterized by vasospasm and ischemia of the limbs and other tissues, including the central nervous system, were recorded.
Interaction with other drugs. In patients receiving clarithromycin tablets in combination with digoxin, an increase in serum concentrations of the latter was observed. Monitoring serum digoxin levels is advisable.
Colchicine. It is a substrate for CYP3A and P-glycoprotein. Clarithromycin and other macrolides are inhibitors of CYP3A and P-glycoprotein. When colchicine and clarithromycin are coadministered, inhibition of P-glycoprotein and/or CYP3A may result in increased effects of colchicine. Patients should be closely monitored for symptoms of colchicine toxicity.
Interaction with antiretroviral drugs. Concomitant oral use of clarithromycin tablets with zidovudine in HIV-infected adults may result in a decrease in the Css of zidovudine. This interaction was not observed in HIV-infected children taking clarithromycin pediatric suspension with zidovudine or dideoxyinosine.
In a pharmacokinetic study, the combined use of ritonavir at a dose of 200 mg every 8 hours and clarithromycin at a dose of 500 mg every 12 hours resulted in a significant suppression of the metabolism of clarithromycin. Cmax of clarithromycin when combined with ritonavir increased by 31%, Cmin by 182%, AUC by 77%.
Virtually complete inhibition of the formation of 14-hydroxyclarithromycin was observed. Given the high therapeutic index of clarithromycin, a dose reduction is not required in patients with normal renal function. However, in patients with impaired renal function, dose adjustment is advisable.
In patients with Cl creatinine 30–60 ml/min, the dose of clarithromycin is reduced by 50%, and in patients with Cl creatinine
Overdose
Overdose
Symptoms: Taking a large dose of clarithromycin may cause symptoms of gastrointestinal disorders. In one patient with a history of bipolar disorder, changes in mental status, paranoid behavior, hypokalemia, and hypoxemia were described after taking 8 g of clarithromycin.
Treatment: in case of overdose, the unabsorbed drug should be removed from the gastrointestinal tract and symptomatic therapy should be carried out. Hemodialysis and peritoneal dialysis do not have a significant effect on the level of clarithromycin in the serum, which is also typical for other macrolide drugs.
Manufacturer
Manufacturer
EbbVee S.r.L., Italy
Additional information
| Manufacturer | AbbVi S.r.l., Italy |
|---|---|
| Medication form | granules for preparation of oral suspension |
| Brand | AbbVi S.r.l. |
Other forms…
Related products
Buy Clacid, 250 mg/5 ml 49.5 g 1 ml with delivery to USA, UK, Europe and over 120 other countries.