No products in the cart.
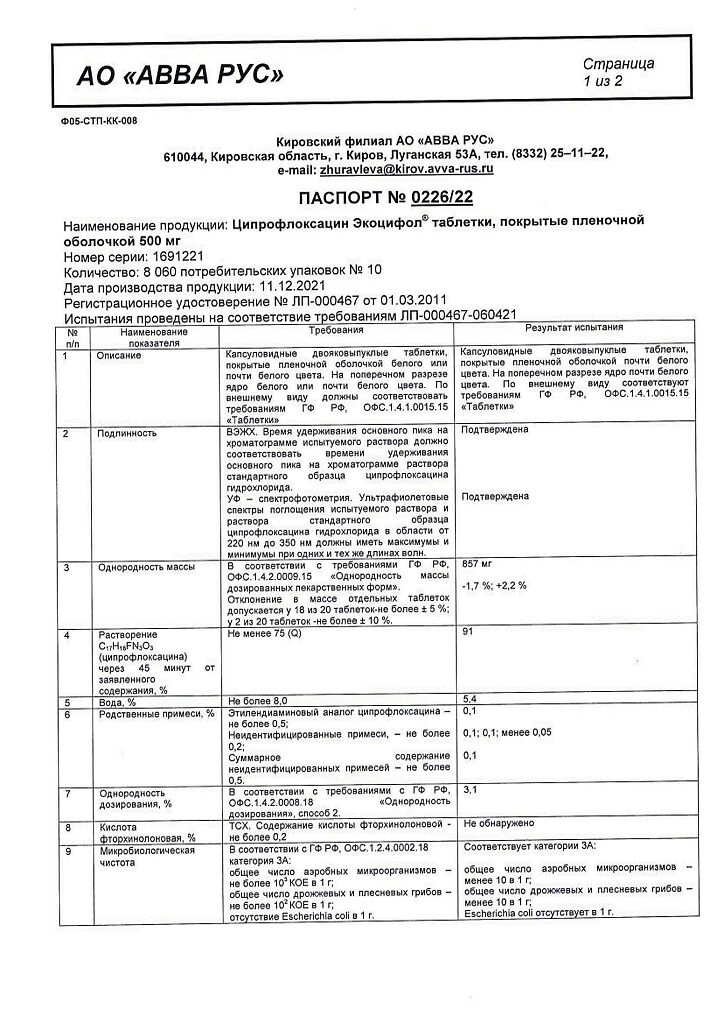
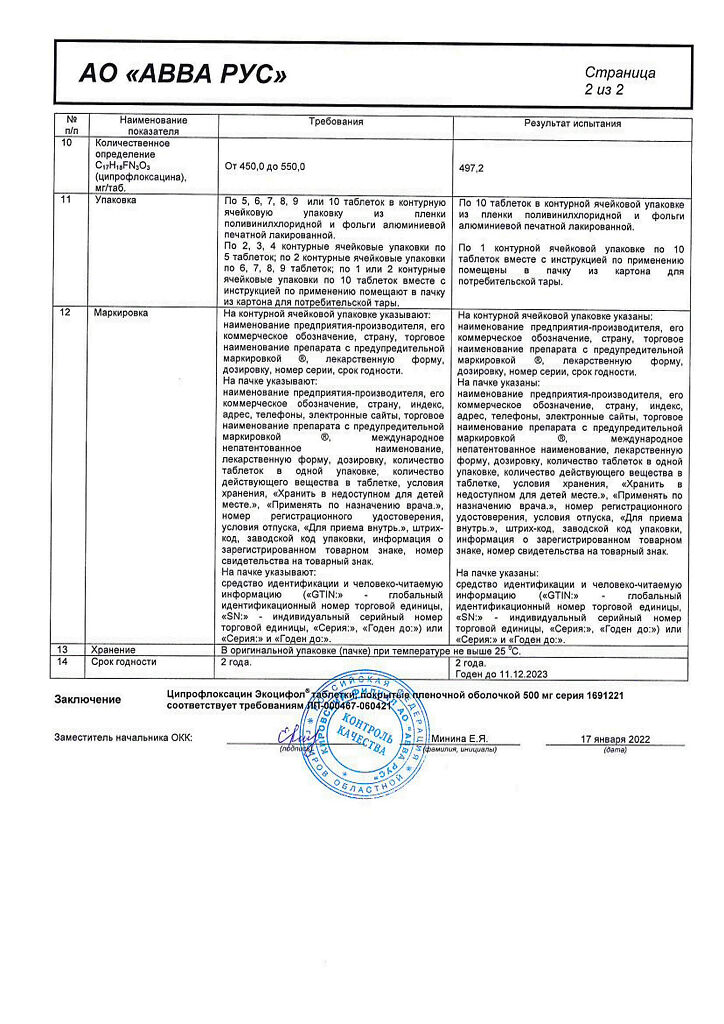
Ciprofloxacin Ecocifol, 500 mg 10 pcs
€3.00
Description
Pharmacotherapeutic group
Antimicrobial agent, fluoroquinolone
ATX Code
J01MA02
Pharmacodynamics:
The broad spectrum antimicrobial agent quinolone derivative inhibits bacterial DNA-gyrosis (topoisomerases II and IV responsible for the process of superspiralization of chromosomal DNA around nuclear RNA which is necessary for reading genetic information) disrupts DNA synthesis growth and division of bacteria; causes pronounced morphological changes (including cell wall, membrane and membrane).cell wall and membranes) and rapid death of the bacterial cell.
It acts bactericidally on Gram-negative organisms during resting and dividing (as it affects not only DNA-giase but also causes lysis of cell wall) on Gram-positive microorganisms – only during dividing.
Low toxicity for macroorganism cells is explained by the absence of DNA-hyrase in them. During ciprofloxacin administration there is no parallel development of resistance to other antibiotics which do not belong to DNA-Gyrase inhibitors group and this fact makes it highly effective against bacteria resistant to aminoglycosides, penicillins and cephalosporins and tetracyclines, for example.
Ciprofloxacin is sensitive to Gram-negative aerobic bacteria: Enterobacteriaceae (Escherichia coli Salmonella spp. Shigella spp. Citrobacter spp. Klebsiella spp. Enterobacter spp. Proteus mirabilis Proteus vulgaris Serratia marcescens Hafnia alvei Edwardsiella tarda Providencia spp. Morganella morganii Vibrio spp. Yersinia spp.) other Gram-negative bacteria (Haemophilus spp. Pseudomonas aeruginosa Moraxella catarrhalis Aeromonas spp. Pasteurella multocida Plesiomonas shigelloides Campylobacter jejuni Neisseria spp.); some intracellular pathogens: Legionella pneumophila Brucella spp. Listeria monocytogenes Mycobacterium tuberculosis Mycobacterium kansasii.
The following Gram-positive aerobic bacteria are also sensitive to ciprofloxacin: Staphylococcus spp. (Staphylococcus aureus Staphylococcus haemolyticus Staphylococcus hominis Staphylococcus saprophyticus) Streptococcus spp. (Streptococcus pyogenes Streptococcus agalactiae).
Active against Bacillus anthracis.
Most methicillin-resistant staphylococci are also resistant to ciprofloxacin. The sensitivity of Streptococcus pneumoniae Enterococcus faecalis Mycobacterium avium (located intracellularly) is moderate (high concentrations are required for their suppression).
Bacteroides fragilis Pseudomonas cepacia Pseudomonas maltophilia Ureaplasma urealyticum Clostridium difficile Nocardia asteroides are resistant to the drug. It is not effective against Treponema pallidum.
Resistance develops very slowly as there are practically no persistent microorganisms after ciprofloxacin action on the one hand and on the other hand bacterial cells have no enzymes which inactivate it. Pharmacokinetics:
In oral administration it is quickly and completely enough absorbed from the gastrointestinal tract (mainly in the duodenum and jejunum). Food intake slows down absorption but does not change maximum concentration (Cmax) and bioavailability. Bioavailability – 50-85% volume of distribution – 2-35 l/kg binding to plasma proteins – 20-40%. Time to reach maximal concentration (TCmax) – 60-90 min, maximal concentration depends linearly on the dose taken and is 12 24 43 and 54 mcg/ml at doses of 250 500 750 and 1000 mg, respectively. Twelve hours after oral doses of 250,500 and 750 mg, the plasma concentration of the drug decreases to 01 02 and 04 mcg/ml, respectively.
The drug is well distributed in body tissues (excluding fat-rich tissue such as nerve tissue). Concentrations in tissues are 2-12 times higher than in plasma. Therapeutic concentrations are reached in saliva tonsils liver gallbladder bile intestine abdominal and pelvic organs (endometrium fallopian tubes and ovaries uterus) seminal fluid prostate tissue kidney and urinary organs lung tissue bronchial secretion bone tissue muscle synovial fluid and articular cartilage peritoneal fluid skin. Small amount of cerebrospinal fluid is infiltrated into the cerebrospinal fluid, where its concentration in the absence of inflammation of the meninges is 6-10% of that in blood serum, and 14-37% in inflamed ones. Ciprofloxacin also penetrates well into the ocular fluid pleura peritoneal lymph through the placenta. Concentration of ciprofloxacin in neutrophils is 2-7 times higher than in blood serum.
It is metabolized in the liver (15-30%) with the formation of slightly active metabolites (diethylcyclofloxacin sulfociprofloxacin oxociprofloxacin formylciprofloxacin).
The elimination half-life is about 4 hours in chronic renal failure up to 12 hours. It is eliminated mainly by kidneys by tubular filtration and tubule secretion unchanged (40-50 %) and as metabolites (15 %); the rest part is eliminated through gastrointestinal tract. A small amount is excreted with breast milk.
Renal clearance is 3-5 ml/min/kg; total clearance is 8-10 ml/min/kg.
In chronic renal failure (creatinine clearance greater than 20 ml/minute) the percentage of ciprofloxacin excreted through the kidneys decreases, but there is no cumulation in the body due to compensatory increase of ciprofloxacin metabolism excretion through the gastrointestinal tract.
Indications
Indications
Infectious and inflammatory diseases caused by sensitive microorganisms:
diseases of the lower respiratory tract (acute and chronic (in the acute stage) bronchitis, pneumonia, bronchiectasis, infectious complications of cystic fibrosis);
ENT infections (acute sinusitis);
kidney and urinary tract infections (cystitis, pyelonephritis);
complicated intra-abdominal infections (in combination with metronidazole);
chronic bacterial prostatitis;
uncomplicated gonorrhea;
typhoid fever, campylobacteriosis, shigellosis, traveler’s diarrhea;
infections of the skin and soft tissues (infected ulcers, wounds, burns, abscesses, phlegmon);
bones and joints (osteomyelitis, septic arthritis);
infections due to immunodeficiency (occurring during treatment with immunosuppressive drugs or in patients with neutropenia);
prevention and treatment of pulmonary anthrax.
Children:
treatment of complications caused by Pseudomonas aeruginosa in children with cystic fibrosis of the lungs from 5 to 17 years;
prevention and treatment of pulmonary anthrax (infection with Bacillus anthracis).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Antimicrobial agent, fluoroquinolone
ATX code
J01MA02
Pharmacodynamics:
A broad-spectrum antimicrobial agent, a quinolone derivative, suppresses bacterial DNA gyrase (topoisomerases II and IV responsible for the process of supercoiling of chromosomal DNA around nuclear RNA, which is necessary for reading genetic information), disrupts DNA synthesis, growth and division of bacteria; causes pronounced morphological changes (including cell wall and membranes) and rapid death of the bacterial cell.
It has a bactericidal effect on gram-negative organisms during the period of rest and division (since it affects not only DNA gyrase but also causes lysis of the cell wall) on gram-positive microorganisms – only during the period of division.
Low toxicity for the cells of the macroorganism is explained by the absence of DNA gyrase in them. While taking ciprofloxacin, there is no parallel development of resistance to other antibiotics that do not belong to the group of DNA gyrase inhibitors, which makes it highly effective against bacteria that are resistant, for example, to aminoglycosides, penicillins, cephalosporins, tetracyclines.
Gram-negative aerobic bacteria are sensitive to ciprofloxacin: enterobacteria (Escherichia coli Salmonella spp. Shigella spp. Citrobacter spp. Klebsiella spp. Enterobacter spp. Proteus mirabilis Proteus vulgaris Serratia marcescens Hafnia alvei Edwardsiella tarda Providencia spp. Morganella morganii Vibrio spp. Yersinia spp.) other gram-negative bacteria (Haemophilus spp. Pseudomonas aeruginosa Moraxella catarrhalis Aeromonas spp. Pasteurella multocida Plesiomonas shigelloides Campylobacter jejuni Neisseria spp.); some intracellular pathogens: Legionella pneumophila Brucella spp. Listeria monocytogenes Mycobacterium tuberculosis Mycobacterium kansasii.
Gram-positive aerobic bacteria are also sensitive to ciprofloxacin: Staphylococcus spp. (Staphylococcus aureus Staphylococcus haemolyticus Staphylococcus hominis Staphylococcus saprophyticus) Streptococcus spp. (Streptococcus pyogenes Streptococcus agalactiae).
Active against Bacillus anthracis.
Most staphylococci resistant to methicillin are also resistant to ciprofloxacin. The sensitivity of Streptococcus pneumoniae Enterococcus faecalis Mycobacterium avium (located intracellularly) is moderate (high concentrations are required to suppress them).
The following are resistant to the drug: Bacteroides fragilis Pseudomonas cepacia Pseudomonas maltophilia Ureaplasma urealyticum Clostridium difficile Nocardia asteroides. Not effective against Treponema pallidum.
Resistance develops extremely slowly because, on the one hand, after the action of ciprofloxacin there are practically no persistent microorganisms left and, on the other hand, bacterial cells do not have enzymes that inactivate it.
Pharmacokinetics:
When taken orally, it is quickly and fairly completely absorbed from the gastrointestinal tract (mainly in the duodenum and jejunum). Eating slows down absorption but does not change the maximum concentration (Cmax) or bioavailability. Bioavailability – 50-85%; volume of distribution – 2-35 l/kg; binding to plasma proteins – 20-40%. The time to reach the maximum concentration (TCmax) is 60-90 minutes; the maximum concentration linearly depends on the size of the dose taken and is 12 24 43 and 54 μg/ml at doses of 250, 500, 750 and 1000 mg, respectively. 12 hours after oral administration of 250,500 and 750 mg, the concentration of the drug in plasma decreases to 01,02 and 04 mcg/ml, respectively.
It is well distributed in body tissues (excluding tissue rich in fats, such as nervous tissue). The concentration in tissues is 2-12 times higher than in plasma. Therapeutic concentrations are achieved in saliva tonsils liver gallbladder bile intestines abdominal and pelvic organs (endometrium fallopian tubes and ovaries uterus) seminal fluid prostate tissue kidneys and urinary organs lung tissue bronchial secretions bone tissue muscles synovial fluid and articular cartilage peritoneal fluid skin. It penetrates into the cerebrospinal fluid in small quantities, where its concentration in the absence of inflammation of the meninges is 6-10% of that in the blood serum, and with inflammation – 14-37%. Ciprofloxacin also penetrates well into the ocular fluid, pleura, peritoneum, and lymph through the placenta. The concentration of ciprofloxacin in blood neutrophils is 2-7 times higher than in blood serum.
Metabolized in the liver (15-30%) with the formation of low-active metabolites (diethylciprofloxacin sulfociprofloxacin oxociprofloxacin formylciprofloxacin).
The half-life is about 4 hours; in chronic renal failure, it is up to 12 hours. It is excreted mainly by the kidneys by tubular filtration and tubular secretion in unchanged form (40-50%) and in the form of metabolites (15%), the rest through the gastrointestinal tract. A small amount is excreted in breast milk.
Renal clearance – 3-5 ml/min/kg; total clearance – 8-10 ml/min/kg.
In chronic renal failure (creatinine clearance above 20 ml/min), the percentage of ciprofloxacin excreted through the kidneys decreases, but accumulation in the body does not occur due to a compensatory increase in the metabolism of ciprofloxacin excreted through the gastrointestinal tract.
Special instructions
Special instructions
In patients with epilepsy, seizures, a history of vascular diseases and organic brain lesions, due to the risk of developing adverse reactions from the central nervous system, ciprofloxacin should be prescribed only for health reasons.
If severe and prolonged diarrhea occurs during or after treatment with ciprofloxacin, the diagnosis of pseudomembranous colitis should be excluded, which requires immediate discontinuation of the drug and the appointment of appropriate treatment. The use of drugs that suppress intestinal motility is contraindicated.
If pain occurs in the tendons or when the first signs of tenosynovitis appear, treatment should be stopped due to the fact that isolated cases of inflammation and even tendon rupture have been described during treatment with fluoroquinolones.
During treatment with ciprofloxacin, it is necessary to provide a sufficient amount of fluid while maintaining normal diuresis.
During treatment with ciprofloxacin, contact with direct sunlight should be avoided.
Considering that women are characterized by a longer average duration of the QT interval compared to men, they are more sensitive to drugs that cause prolongation of the QT interval. Ciprofloxacin should be used with caution in combination with drugs that prolong the QT interval (for example, class IA and III antiarrhythmic drugs, tricyclic antidepressants, macrolides, antipsychotics) in patients with an increased risk of prolongation of the QT interval or the development of torsade de pointes (for example, congenital long QT syndrome, heart disease (heart failure, myocardial infarction, bradycardia) electrolyte imbalance (for example, hypokalemia, hypomagnesemia)).
Cases of liver necrosis and life-threatening liver failure have been reported with the use of ciprofloxacin. If symptoms of liver disease such as anorexia, jaundice, dark urine, itching, abdominal pain are present, the use of ciprofloxacin should be discontinued. In patients with myasthenia gravis gravis, ciprofloxacin should be used with caution as it may worsen symptoms.
When using ciprofloxacin, cases of tendonitis and tendon rupture (mainly the Achilles tendon), sometimes bilateral, may occur within the first 48 hours after the start of therapy; inflammation and rupture of the tendon can occur even several months after stopping treatment with ciprofloxacin. In elderly patients and in patients with tendon diseases who are simultaneously treated with glucocorticosteroids, there is an increased risk of tendinopathy.
Cases of status epilepticus have been reported when using ciprofloxacin. Ciprofloxacin, like other fluoroquinolones, can provoke seizures and reduce the seizure threshold. If seizures occur, use of the drug should be discontinued. Mental reactions may occur even after the first use of fluoroquinolones, including ciprofloxacin.
In patients using fluoroquinolones, including ciprofloxacin, cases of sensory and sensorimotor axonal polyneuropathy affecting small and (or) large axons and leading to paresthesia, hypoesthesia, dysesthesia and weakness have been reported. Symptoms may appear soon after starting use and may be irreversible. If the patient develops symptoms of neuropathy including pain, burning, tingling, numbness and/or weakness or other sensory disturbances including tactile pain, temperature vibration sensitivity and position sense, the use of ciprofloxacin should be discontinued immediately.
In rare cases, depression or psychotic reactions may progress to suicidal thoughts and self-harmful behavior such as attempted or completed suicide. If the patient develops one of these reactions, stop taking the drug and notify the doctor; Caution should be exercised when simultaneous use of ciprofloxacin and drugs metabolized by CYP4501A2 isoenzymes such as ropinirole olanzapine theophylline methylxanthine caffeine duloxetine clozapine.
Sometimes, after taking the first dose of ciprofloxacin, hypersensitivity to the drug, including allergic reactions, may develop, which should be reported to your doctor immediately. In extremely rare cases, after the first use, anaphylactic reactions up to anaphylactic shock may occur. In these cases, the use of ciprofloxacin should be stopped immediately and appropriate treatment should be carried out.
Because ciprofloxacin has some activity against Mycobacterium tuberculosis, false-negative culture results may be obtained when specimens are collected during treatment with ciprofloxacin.
Impact on the ability to drive vehicles. Wed and fur.:
During treatment, you should refrain from driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Ciprofloxacin
Composition
Composition
One tablet contains:
Active substance:
ciprofloxacin hydrochloride monohydrate (in terms of ciprofloxacin) 500 mg;
Excipients:
lactulose 600.0 mg,
low molecular weight povidone 28.0 mg,
croscarmellose sodium 65.0 mg,
microcrystalline cellulose 60.0 mg,
magnesium stearate 10.0 mg,
sufficient amount of corn starch to obtain an uncoated tablet weighing 1400.0 mg;
Shell excipients:
hypromellose 19.04 mg, macrogol-4000 8.32 mg, talc 2.2 mg, titanium dioxide 10.44 mg.
Contraindications
Contraindications
Hypersensitivity, simultaneous use with tizanidine (risk of a pronounced decrease in blood pressure, drowsiness), age up to 18 years (before the completion of the skeletal formation process, except for the treatment of complications caused by Pseudomonas aeruginosa in children with cystic fibrosis of the lungs from 5 to 17 years old; prevention and treatment of pulmonary anthrax), pregnancy, lactation period.
With caution
Severe cerebral atherosclerosis, cerebrovascular accident, mental illness, epilepsy, severe renal and/or liver failure, old age.
Side Effects
Side Effects
From the digestive system: nausea, diarrhea, vomiting, abdominal pain, flatulence, decreased appetite and amount of food taken, anorexia, cholestatic jaundice (especially in patients with previous liver diseases), hepatitis, pancreatitis, hepatonecrosis.
From the nervous system: dizziness headache increased fatigue tremor insomnia “nightmare” dreams paresthesia and dysesthesia hypoesthesia hyperesthesia convulsions vertigo incoordination sweating anxiety psychomotor hyperactivity/agitation disorientation confusion hallucinations psychotic reactions (which can lead to self-injurious behavior such as suicidal behavior/thoughts and suicide attempt or successful suicide) depression (which can lead to self-harmful behavior such as suicidal behavior/thoughts and suicide attempt or successful suicide) seizures epilepsy benign intracranial hypertension peripheral neuropathy and polyneuropathy.
From the senses: disturbances of taste and smell, visual disturbances (diplopia, changes in color perception), tinnitus, hearing loss, hearing loss.
From the cardiovascular system: tachycardia, prolongation of the QT interval, ventricular arrhythmias (including torsade de pointes), decreased blood pressure, flushing of the face, vasodilation.
From the hematopoietic system: neutropenia leukopenia agranulocytosis granulocytopenia anemia thrombocytopenia leukocytosis thrombocytosis hemolytic anemia pancytopenia (life-threatening).
From the laboratory parameters: increased activity of “liver” transaminases and alkaline phosphatase, hypercreatininemia, hyperbilirubinemia, hyperglycemia, hypoglycemia, increased international normalized ratio (in patients receiving vitamin K antagonists), changes in prothrombin levels, increased amylase activity.
From the urinary system: hematuria crystalluria (primarily with alkaline urine and low diuresis), impaired renal function, renal failure, interstitial nephritis.
Allergic reactions: skin itching rash urticaria formation of blisters accompanied by bleeding and small nodules forming scabs drug fever pinpoint hemorrhages (petechiae) swelling of the face or larynx shortness of breath eosinophilia increased photosensitivity vasculitis erythema nodosum exudative erythema multiforme acute generalized pustular exanthema Stevens-Johnson syndrome (malignant exudative erythema) toxic epidermal necrolysis (Lyell’s syndrome) angioedema anaphylactic reactions anaphylactic shock (life-threatening) serum sickness.
Other: respiratory failure (including bronchospasm) arthralgia arthritis tenosynovitis tendon ruptures general weakness myalgia increased muscle tone muscle cramps muscle weakness exacerbation of myasthenia gravis symptoms gait disturbance superinfections (candidiasis pseudomembranous colitis).
Interaction
Interaction
Due to a decrease in the activity of microsomal oxidation processes in hepatocytes, it increases the concentration and lengthens the half-life of theophylline (and other xanthines, such as caffeine), oral hypoglycemic drugs, indirect anticoagulants, and helps reduce the prothrombin index. When taken simultaneously with theophylline, it is recommended to constantly monitor the concentration of theophylline in the blood plasma and, if necessary, reduce the dose of theophylline.
When combined with other antimicrobial drugs (beta-lactam antibiotics, aminoglycosides, clindamycin, metronidazole), synergism is usually observed; can be successfully used in combination with azlocillin and ceftazidime for infections caused by Pseudomonas spp.; with mezlocillin, azlocillin and other beta-lactam antibiotics – for streptococcal infections; with isoxazolylpenicillins and vancomycin – for staphylococcal infections; with metronidazole and clindamycin – for anaerobic infections.
Enhances the nephrotoxic effect of cyclosporine; an increase in serum creatinine is noted; in such patients, this indicator must be monitored 2 times a week.
When taken concomitantly with indirect anticoagulants, the international normalized ratio should be monitored quite often and also within a short time after completion of combination therapy. Oral administration together with iron-containing drugs sucralfate and antacid drugs containing magnesium, calcium and aluminum salts leads to a decrease in the absorption of ciprofloxacin, so it should be prescribed 1-2 hours before or 4 hours after taking the above drugs.
The simultaneous use of ciprofloxacin and dairy products or drinks fortified with minerals (eg milk, yogurt, calcium-fortified orange juice) should be avoided as the absorption of ciprofloxacin may be reduced. However, calcium contained in other foods does not significantly affect the absorption of ciprofloxacin.
Non-steroidal anti-inflammatory drugs (excluding acetylsalicylic acid) increase the risk of developing seizures. Fluoroquinolones form chelate compounds with magnesium and aluminum ions in the buffer system of the dosage form of didanosine, which sharply reduces the absorption of antibiotics; therefore, ciprofloxacin is taken 2 hours before taking didanosine or 2 hours after taking this drug.
Metoclopramide accelerates absorption, which leads to a decrease in the time to reach its maximum concentration.
Ciprofloxacin, due to a decrease in the activity of microsomal oxidation processes in hepatocytes, increases the plasma concentration and prolongs T1/2 of glibenclamide, which can lead to hypoglycemia in rare cases – severe. The simultaneous use of ciprofloxacin with glibenclamide may enhance the effect of the latter.
With the simultaneous use of ciprofloxacin and phenytoin, a change (increase or decrease) in the content of phenytoin in the blood plasma was observed. To avoid weakening of the anticonvulsant effect of phenytoin due to a decrease in its concentration, as well as to prevent adverse events associated with phenytoin overdose when discontinuing ciprofloxacin, it is recommended to monitor phenytoin therapy in patients taking both drugs. including determination of phenytoin levels in blood plasma during the entire period of simultaneous use of both drugs and for a short time after completion of combination therapy. Caution should be exercised when ciprofloxacin and other fluoroquinolones are used simultaneously in patients receiving drugs that prolong the QT interval (for example, class 1A or class III antiarrhythmic drugs, tricyclic antidepressants, macrolides, antipsychotics) (see section “Special Instructions”).
The combined use of uricosuric drugs leads to a slower elimination (up to 50%) and an increase in plasma concentrations of ciprofloxacin. Increases the maximum concentration by 7 times (from 4 to 21 times) and the area under the concentration-time curve by 10 times (from 6 to 24 times) of tizanidine, which exceeds the risk of a pronounced decrease in blood pressure and drowsiness.
When used simultaneously with omeprazole, a slight decrease in the maximum plasma concentration of the drug and a decrease in AUC may be observed.
Probenecid inhibits the renal excretion of ciprofloxacin leading to increased concentrations of ciprofloxacin.
In a study on healthy volunteers, it was found that the simultaneous use of drugs containing lidocaine and ciprofloxacin, a moderate inhibitor of the CYP1A2 isoenzyme, leads to a decrease in the clearance of lidocaine by 22% when administered intravenously. Despite the good tolerability of lidocaine, when used simultaneously with ciprofloxacin, side effects may increase due to interaction.
With simultaneous use of clozapine and ciprofloxacin at a dose of 250 mg for 7 days, an increase in serum concentrations of clozapine and N-desmethylclozapine by 29% and 31%, respectively, was observed. The patient’s condition should be monitored and, if necessary, the dosage regimen of clozapine should be adjusted during its simultaneous use with ciprofloxacin and for a short time after completion of combination therapy.
With the simultaneous use of ciprofloxacin and methotrexate, there is a slowdown in the renal tubular transport of methotrexate, potentially leading to an increase in plasma concentrations of methotrexate, which may increase the risk of toxic reactions associated with methotrexate. Therefore, it is necessary to monitor the condition of patients when treated with methotrexate and simultaneously taking ciprofloxacin.
During clinical studies, it was shown that the simultaneous use of duloxetine and potent inhibitors of the CYP1A2 isoenzyme (such as fluvoxamine) may lead to an increase in the AUC and Cmax of duloxetine. Despite the lack of clinical data on possible interactions with ciprofloxacin, the likelihood of such an interaction can be anticipated when ciprofloxacin and duloxetine are used simultaneously.
When ropinirole is used concomitantly with ciprofloxacin, there is a possibility of increased concentrations of ropinirole, which may be accompanied by an increased risk of adverse reactions. If used concomitantly, monitor for adverse effects of ropinirole during coadministration with ciprofloxacin and for a short time after completion of combination therapy.
With simultaneous use of ciprofloxacin at a dose of 500 mg and sildenafil at a dose of 50 mg, a 2-fold increase in Cmax and AUC of sildenafil was observed. The use of this combination is possible only after assessing the benefit/risk ratio.
Overdose
Overdose
Symptoms: nausea, vomiting, confusion, dizziness, tremor, headache, fatigue, seizures, hallucinations, mental agitation, prolongation of the QTc interval, gastrointestinal disorders, liver and kidney dysfunction, crystalluria, hematuria.
A specific antidote is unknown. It is necessary to carefully monitor the patient’s condition, perform gastric lavage, carry out routine emergency measures, and ensure sufficient fluid intake. Using hemo- or peritoneal dialysis, only a small (less than 10%) amount of the drug can be removed.
To prevent the development of crystalluria, it is recommended to monitor renal function, including urine pH and acidity.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25°C.
Keep out of the reach of children.
Shelf life
Shelf life
2 years. Do not use after expiration date.
Manufacturer
Manufacturer
ABVA RUS, Russia
Additional information
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In a dry place protected from light at a temperature not exceeding 25°C. Store out of the reach of children. |
| Manufacturer | Avva Rus, Russia |
| Medication form | pills |
| Brand | Avva Rus |
Related products
Buy Ciprofloxacin Ecocifol, 500 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.