Subtotal: €1.75
Ciprofloxacin, 500 mg 10 pcs
€3.12 €2.93
Respiratory tract infections, Biliary tract infections, Intestinal infections, Skin infections, Otitis media, Sinusitis, Urinary tract infections, Pneumonia, Infectious diseases
According to rxlist.com (2020), oral ciprofloxacin is indicated to treat infections caused by susceptible strains of microorganisms.
Adult patients
. Skin and soft tissue infections caused by Escherichia coli, Klebsiella pneumoniae, Enterobacter cloacae, Proteus mirabilis, Proteus vulgaris, Providencia stuartii, Morganella morganii, Citrobacter freundii, Pseudomonas aeruginosa, methicillin-sensitive strains of Staphylococcus aureus, methicillin-sensitive strains of Staphylococcus epidermidis or Streptococcus pyogenes.
Bone and joint infections caused by Enterobacter cloacae, Serratia marcescens, Pseudomonas aeruginosa.
Complicated intra-abdominal infections (in combination with metronidazole) caused by Escherichia coli, Pseudomonas aeruginosa, Proteus mirabilis, Klebsiella pneumoniae or Bacteroides fragilis.
Infectious diarrhea caused by Escherichia coli (enterotoxigenic isolates), Campylobacter jejuni, Shigella boydii*, Shigella dysenteriae, Shigella flexneri, Shigella sonnei* when antibiotic therapy is indicated.
* Although treatment of infections caused by this microorganism in this organ system has demonstrated clinically significant results, efficacy has been studied in fewer than 10 patients.
Typhoid fever caused by Salmonella typhi. The efficacy of ciprofloxacin for eradication of the pathogen in chronic carriage has not been demonstrated.
Uncomplicated gonorrhea (cervical and urethral) caused by Neisseria gonorrhoeae.
Chronic bacterial prostatitis caused by Escherichia coli or Proteus mirabilis.
Infections of the lower respiratory tract
– Infections caused by Escherichia coli, Klebsiella pneumoniae, Enterobacter cloacae, Proteus mirabilis, Pseudomonas aeruginosa, Haemophilus influenzae, Haemophilus parainfluenzae or Streptococcus pneumoniae.
– Ciprofloxacin is not the drug of first choice in the treatment of suspected or confirmed pneumonia caused by Streptococcus pneumoniae.
– Treatment of exacerbations of chronic bronchitis caused by Moraxella catarrhalis.
Because the use of fluoroquinolones, including ciprofloxacin, is associated with a risk of serious adverse reactions (see Precautions), and in some patients exacerbations of chronic bronchitis are self-resolving, use for this indication is possible only if other treatments have been unsuccessful.
Urinary tract infections
– Urinary tract infections caused by Escherichia coli, Klebsiella pneumoniae, Enterobacter cloacae, Serratia marcescens, Proteus mirabilis, Providencia rettgeri, Morganella morganii, Citrobacter koseri, Citrobacter freundii, Pseudomonas aeroportixermoctiae. Staphylococcus saprophyticus or Enterococcus faecalis, in adults.
– Acute uncomplicated cystitis caused by Escherichia coli or Staphylococcus saprophyticus, in adult women.
Because the use of fluoroquinolones, including ciprofloxacin, is associated with a risk of serious adverse reactions (see Precautions), and acute uncomplicated cystitis is a self-resolving condition in some patients, use for this indication is possible only if other treatments have been unsuccessful.
Pediatric patients
Complicated urinary tract infections and Escherichia coli-induced pyelonephritis in pediatric patients aged 1 to 17 years.
Despite efficacy in clinical trials, ciprofloxacin is not the drug of first choice in pediatric patients because of increased rates of adverse reactions compared to controls, including joint and/or surrounding tissue reactions. Ciprofloxacin use, like other fluoroquinolones, is associated with arthropathy and histopathological changes in load-bearing joints in young animals (see Pharmacology and Toxicology in Animals).
Acute sinusitis caused by Haemophilus influenzae, Streptococcus pneumoniae or Moraxella catarrhalis.
Because the use of fluoroquinolones, including ciprofloxacin, is associated with a risk of serious adverse reactions (see Precautions), and acute sinusitis is a self-resolving condition in some patients, use for this indication is possible only if other treatments have been unsuccessful.
Adult and pediatric patients
Pulmonary anthrax (after exposure). Ciprofloxacin is indicated in adult and pediatric patients ages birth to 17 years for inhalational anthrax (after exposure) to reduce the incidence or progression of disease after exposure to Bacillus anthracis in aerosol form.
The ciprofloxacin concentrations achieved in human serum served as a surrogate endpoint reasonably predictive of clinical efficacy and served as the initial basis for approval of this indication.1 Confirmatory clinical information on ciprofloxacin for post-exposure anthrax prophylaxis was obtained during the October 2001 anthrax bioterror attacks (see Clinical Studies).
Plague, including pneumonic and septic plague caused by Yersinia pestis, and for the prevention of plague in adult and pediatric patients from birth to 17 years. A study of the efficacy of ciprofloxacin could not be conducted in plague patients. This indication is based on efficacy studies performed only on animals (see Clinical Studies).
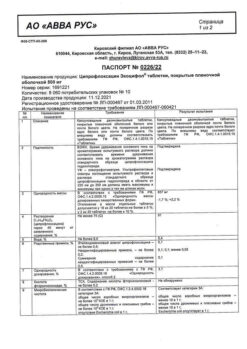
Active ingredient
Composition
Per 1 tablet:
Core:
Active substance:
Ciprofloxacin hydrochloride monohydrate – 590 mg (in terms of ciprofloxacin – 500 mg).
Auxiliary substances:
Corn starch, pregelatinized starch (starch 1500), crosspovidone, lactose monohydrate, microcrystalline M 102 cellulose, talc, magnesium stearate.
The shell:
Hypromellose, macrogol4000 (polyethylene oxide 4000, polyethylene glycol 4000), propylene glycol, talc, copovidone (collidon VA 64, collidon VA64), titanium dioxide.
How to take, the dosage
Ingestion. The dose, route of administration and duration of therapy depend on localization and severity of infection, individual characteristics of the patient, including the state of renal and hepatic function and clinical effect.
Loss of function and potentially irreversible serious adverse reactions, including tendonitis and tendon rupture, peripheral neuropathy and CNS effects
The use of fluoroquinolones, including ciprofloxacin, is associated with the development of potentially irreversible serious adverse reactions from different body systems that may occur simultaneously in the same patient. These adverse reactions include tendinitis, tendon rupture, arthralgia, myalgia, peripheral neuropathy and CNS effects (hallucinations, anxiety, depression, insomnia, severe headache, confusion). These reactions may occur within hours or weeks after starting ciprofloxacin.
These adverse reactions have been observed regardless of patient age and without prior risk factors.
Stop taking ciprofloxacin immediately at the first signs or symptoms of any serious adverse effect.
Tendinitis and tendon rupture
The use of fluoroquinolones, including ciprofloxacin, is associated with an increased risk of tendinitis and tendon rupture in patients of any age. Achilles tendon injury is more common, and tendonitis and tendon rupture of the rotator cuff, hand, biceps, thumb, and other localized tendons have also been reported. Tendinitis or tendon rupture may occur within hours or days after initiation of ciprofloxacin therapy or within months of completion of therapy and may be bilateral.
The risk of fluoroquinolone-associated tendinitis and tendon rupture is increased in patients older than 60 years, in patients taking corticosteroids, and in patients with kidney, heart, or lung transplants. Other factors that may independently increase the risk of tendon rupture include vigorous exercise, renal insufficiency, and previous tendon diseases such as rheumatoid arthritis. Tendinitis and tendon rupture have also been reported in patients taking fluoroquinolones but without the above risk factors. If pain, swelling, inflammation or tendon rupture occurs, ciprofloxacin therapy should be stopped immediately, physical activity should be avoided, and a physician should be consulted.
The use of fluoroquinolones, including ciprofloxacin, should be avoided in patients with a history of tendon disease.
Peripheral neuropathy
The use of fluoroquinolones, including ciprofloxacin, is associated with an increased risk of peripheral neuropathy. Cases of sensory or sensorimotor axonal polyneuropathy with lesions of small and/or large axons manifested by paresthesia, hypoesthesia, dysesthesia and weakness have been reported in patients receiving fluoroquinolones, including ciprofloxacin. Symptoms may occur soon after initiation of ciprofloxacin therapy and may be irreversible in some patients.
The use of ciprofloxacin should be stopped immediately if the patient develops symptoms such as pain, burning, tingling, numbness and/or weakness or other sensory disturbances, including impaired sense of touch, pain, hyperthermia, loss of sense of position in space, changes in vibration sensitivity in order to minimize the development of an irreversible condition. Fluoroquinolones, including ciprofloxacin, should be avoided in patients with a history of peripheral neuropathy.
Impacts on the CNS
Mental disorders. Use of fluoroquinolones, including ciprofloxacin, is associated with an increased risk of adverse reactions such as toxic psychosis, psychotic reactions turning into suicidal ideas/thoughts, hallucinations or paranoia; Depression or self-harming behavior (attempted or completed suicide); anxiety, agitation, nervousness, confusion, delirium, disorientation or attention deficit disorder, insomnia or nightmares, memory impairment. These phenomena may occur after the first dose. If these reactions are observed in patients receiving ciprofloxacin, treatment should be discontinued immediately and appropriate measures taken.
CNS adverse reactions. The use of ciprofloxacin, as well as other fluoroquinolones, is associated with an increased risk of seizures, increased IOP (benign intracranial hypertension), dizziness and tremor. Ciprofloxacin, like other fluoroquinolones, causes seizures and lowers the seizure threshold. Cases of epileptic status have been reported. In patients with epilepsy and past or suspected CNS disorders that may predispose to seizures or lower the seizure threshold (e.g., history of seizures, severe cerebral arteriosclerosis, cerebral circulation disorders, organic brain damage or stroke), as well as in the presence of other risk factors (e.g., drug therapy, renal impairment) ciprofloxacin should be used with caution.
The aggravation of myasthenia gravis
Fluoroquinolones, including ciprofloxacin, have neuromuscular conduction-blocking activity and may exacerbate muscle weakness in patients with myasthenia gravis. Serious adverse reactions, including fatalities and the need for ventilatory ventilation, have been observed in the postmarketing period associated with the use of a fluoroquinolone in patients with myasthenia gravis. Ciprofloxacin should be avoided in patients with a history of myasthenia gravis.
Other serious and sometimes fatal reactions
Other serious and sometimes fatal adverse reactions, some of which have been attributed to hypersensitivity and some to an undetermined etiology, have been reported in patients treated with quinolones, including ciprofloxacin. These phenomena can be severe and usually occur after multiple doses. Clinical manifestations may include one or more of the following: fever, rash or severe dermatologic reactions (e.g., toxic epidermal necrolysis, Stevens-Johnson syndrome), vasculitis, arthralgia, myalgia, serum disease, allergic pneumonitis, interstitial nephritis, acute renal failure, hepatitis, jaundice, acute necrosis or liver function failure, anemia, includingincluding hemolytic and aplastic, thrombocytopenia, including thrombotic thrombocytopenic purpura; leukopenia, agranulocytosis, pancytopenia and/or other hematological changes.
The treatment with ciprofloxacin should be discontinued immediately on the first appearance of skin rash, jaundice or any other signs of hypersensitivity and maintenance therapy should be carried out.
Hypersensitivity reactions
There have been reports of serious and sometimes fatal hypersensitivity reactions (anaphylactic), some of which occurred after the first dose, in patients treated with fluoroquinolones, including ciprofloxacin. Some reactions were accompanied by cardiovascular collapse, loss of consciousness, tingling, swelling of the throat or face, dyspnea, urticaria, and itching. Only a few patients have a history of hypersensitivity reactions. If serious anaphylactic reactions occur, the use of ciprofloxacin should be discontinued immediately and appropriate treatment should be given.
Hepatotoxicity
When using ciprofloxacin, there have been cases of severe hepatotoxicity, including liver necrosis and life-threatening liver failure, and deaths. Acute liver damage (can be hepatocellular, cholestatic or mixed) develops rapidly (1 to 39 days) and is often associated with hypersensitivity. The majority of patients with fatalities were over 55 years of age. If any signs and symptoms of hepatitis (such as anorexia, jaundice, darkened urine, itching, abdominal pain) appear, ciprofloxacin should be stopped immediately.
In patients taking ciprofloxacin, especially those with prior liver disease, there may be a temporary increase in hepatic transaminases, alkaline phosphatase activity or cholestatic jaundice (see “Adverse effects”).
Risk of aortic aneurysm and dissection
Epidemiologic studies have reported an increased risk of aortic aneurysm and dissection within 2 months after fluoroquinolones, especially in elderly patients. The cause of the increased risk has not been determined. In patients with known aortic aneurysm or increased risk of aortic aneurysm, ciprofloxacin should be used only in the absence of alternative antibacterial agents.
Serious adverse reactions with concomitant use of theophylline
Serious and fatal reactions have been reported in patients taking ciprofloxacin and theophylline simultaneously. These reactions have included cardiac arrest, seizures, epileptic status, and respiratory failure. There have also been cases of nausea, vomiting, tremor, irritability, or palpitations.
While similar serious adverse reactions have been reported in patients receiving theophylline alone, the possibility that these reactions may be enhanced by ciprofloxacin cannot be excluded. If concomitant use cannot be avoided, serum theophylline levels should be monitored and the dose should be adjusted if necessary (see “Interactions”).
Diarrhea associated with Clostridium difficile
Diarrhea associated with Clostridium difficile has been reported with virtually all antibacterials, including ciprofloxacin, and can range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents leads to a modification of the normal flora of the large intestine and an overgrowth of C. difficile.
The C. difficile strains produce toxins A and B, which cause the development of diarrhea. C. difficile strains producing hypertoxin lead to an increased risk of morbidity and mortality because these infections may be resistant to antimicrobial therapy and require colectomy. The possibility of C. difficile-associated diarrhea should be considered in all patients who present with complaints of diarrhea after antimicrobial use. A thorough history should be taken, as C. difficile-associated diarrhea may develop within two months after antimicrobial use.
If C. difficile-associated diarrhea is suspected or confirmed, ciprofloxacin should be stopped and appropriate treatment (including fluids and electrolytes, protein supplements, antibiotics to which C. difficile strains are sensitive) and surgical evaluation should be initiated if clinically indicated.
The use of some fluoroquinolones, including ciprofloxacin, has been associated with prolongation of the QT interval on the ECG and cases of arrhythmias. During post-marketing surveillance, cases of torsade de pointes have been reported in patients using fluoroquinolones, including ciprofloxacin.
. Ciprofloxacin should be avoided in patients with prolonged QT, risk factors for prolonged QT or torsade de pointes (e.g., congenital prolonged QT syndrome, uncorrected electrolyte imbalances such as hypokalemia or hypomagnesemia heart disease such as heart failure, myocardial infarction, bradycardia), and in patients receiving class IA antiarrhythmic agents (quinidine, procainamide) or class III (amiodarone, sotalol), tricyclic antidepressants, macrolides, neuroleptics (see “Interaction “Interactions”). Elderly patients may also be more sensitive to the effect of drugs causing prolongation of QT interval.
Motor disorders in children and arthropathy in animals
Ciprofloxacin is indicated in pediatric patients (less than 17 years) only for treatment of complicated urinary tract infections, prevention of inhalational anthrax (after exposure) and plague (see “Administration”). There is an increased incidence of adverse reactions compared to controls, including reactions associated with joints and/or surrounding tissues.
In preclinical studies, oral administration of ciprofloxacin caused lameness in immature dogs. Histopathological examination of the joints of these dogs revealed irreversible cartilage damage. Other quinolones also cause cartilage erosion of large joints and other signs of arthropathy in immature animals of various species (see Animal Pharmacology and Toxicology).
Photosensitivity/phototototoxicity
In patients exposed to direct sunlight or UV irradiation during treatment with fluoroquinolones, including ciprofloxacin, moderate to severe photosensitivity/phototototoxicity reactions may occur, the latter of which may manifest as excessive tanning reactions (e.g., burning, erythema, exudation, blisters, blisters, edema) in areas exposed to direct sunlight (typically the face, decollete, forearm surfaces, dorsal surfaces of hands). Excessive exposure to these light sources should therefore be avoided. Therapy should be stopped if a phototoxicity reaction develops.
The development of drug-resistant bacteria
The administration of ciprofloxacin in the absence of confirmed/suspected bacterial infection or for prophylactic reasons increases the risk of development of resistant bacteria.
Potential risk when used concomitantly with drugs metabolized by cytochrome P450 isoenzyme CYP1A2. Ciprofloxacin is an inhibitor of CYP1A2 isoenzyme. Concomitant use of ciprofloxacin and drugs metabolized mainly by this isoenzyme (e.g., methylxanthines including theophylline and caffeine, tizanidine, ropinirole, clozapine, olanzapine, zolpidem) leads to increased concentrations of these drugs in blood plasma and may cause clinically significant adverse reactions (see “Interaction”).
Intervention in the timely diagnosis of syphilis
The effectiveness of ciprofloxacin in the treatment of syphilis has not been proven. Antimicrobials used in high doses for short periods of time to treat gonorrhea may mask or delay symptoms of the incubation period of syphilis. A syphilis serologic test should be performed in all patients with gonorrhea at the time of diagnosis and a control syphilis serologic test 3 months after ciprofloxacin treatment.
Ciprofloxacin crystalluria
Ciprofloxacin crystals have rarely been found in human urine, but more often in the urine of laboratory animals, which is usually alkaline (see Preclinical Toxicology). The development of ciprofloxacin-associated crystalluria has rarely been reported in humans because human urine is usually acidic. Sufficient fluid intake and maintenance of an acidic urine reaction are necessary to avoid the development of crystalluria.
Changes in blood glucose levels
The use of fluoroquinolones, including ciprofloxacin, is associated with changes in blood glucose levels, including symptomatic hypo- and hyperglycemia, usually in patients with diabetes who are simultaneously receiving oral hypoglycemic agents (e.g., glibenclamide) or insulin. Close monitoring of blood glucose levels in these patients is recommended. Severe cases of hypoglycemia leading to coma or death have been reported. If hypoglycemic reaction occurs, the use of ciprofloxacin should be stopped immediately and appropriate therapy should be initiated (see “Interaction”).
The use in geriatrics
Elderly patients are at increased risk of severe tendon disease, including tendon rupture, when treated with a fluoroquinolone such as ciprofloxacin. This risk is further increased in patients receiving concomitant corticosteroid therapy. Tendinitis or tendon rupture can affect the Achilles tendon, tendon of the hand, shoulder, or other tendons and can occur during or after completion of therapy. Cases occurring within a few months of fluoroquinolone treatment have been reported. Caution should be exercised when using ciprofloxacin in elderly patients, especially those taking corticosteroids. Patients should be informed about possible side effects, advised to stop taking ciprofloxacin, and contact their physician if any symptoms of tendinitis or tendon rupture occur.
Epidemiologic studies have reported an increased incidence of aortic aneurysm and dissection within 2 months of fluoroquinolones, especially in older patients.
In a retrospective analysis of 23 controlled multiple-dose clinical trials of ciprofloxacin involving more than 3,500 patients receiving ciprofloxacin, 25% of patients were aged â¥65 years and 10% were aged â¥75 years. No overall differences in safety and efficacy were observed between these patients and younger patients; another clinical trial found no differences in clinical response between older and younger patients, but the greater sensitivity of some older people to any drug therapy cannot be ruled out. Ciprofloxacin is known to be largely excreted by the kidneys, and the risk of adverse reactions may be higher in patients with impaired renal function. Patients over 65 years of age with normal renal function do not require a dosage change. However, because some elderly people have reduced renal function, caution should be exercised when adjusting the dose for elderly patients, and renal function monitoring may be useful in these patients.
Elderly patients may be more susceptible to drug-associated QT interval changes. Therefore, precautions should be taken when using ciprofloxacin with concomitant drugs that may cause QT interval prolongation (e.g., class IA or class III antiarrhythmics) or in patients with risk factors for torsade de pointes (e.g., QT interval prolongation, unadjusted hypokalemia).
Renal dysfunction
Ciprofloxacin is eliminated primarily by the kidneys; however, it is also metabolized and partially eliminated through the hepatic and intestinal biliary systems. These alternative elimination routes appear to compensate for the reduced renal excretion in patients with impaired renal function. Nevertheless, dose modifications are recommended, especially in patients with severe renal dysfunction.
Hepatic dysfunction
In preliminary studies in patients with stable chronic cirrhosis no significant changes in pharmacokinetics of ciprofloxacin have been observed. Pharmacokinetics of ciprofloxacin in patients with acute liver failure have not been studied.
Pediatric use
Despite efficacy in clinical trials, ciprofloxacin is not the drug of first choice in pediatric patients due to increased rates of adverse reactions compared to controls. Quinolones, including ciprofloxacin, cause arthropathy (arthralgia, arthritis) in young animals (see Toxicology and/or Pharmacology in Animals).
Complicated urinary tract infections and pyelonephritis. Ciprofloxacin is indicated for the treatment of complicated urinary tract infections and pyelonephritis caused by Escherichia coli in pediatric patients aged 1 to 17 years. Despite its efficacy in clinical trials, ciprofloxacin is not the drug of first choice in the pediatric population because of the increased incidence of adverse reactions compared to controls, including those associated with effects on joints and/or surrounding tissues.
Pulmonary anthrax (post-exposure). Ciprofloxacin is indicated in pediatric patients from birth to 17 years of age for inhalational anthrax (after exposure). A risk-benefit assessment shows that the use of ciprofloxacin in pediatric patients is appropriate.
Pestilence. Ciprofloxacin is indicated in pediatric patients from birth to 17 years of age for treatment of plague, including pneumonic and septic plague caused by Yersinia pestis (Y. pestis), and for prevention of plague. Studies of the efficacy of ciprofloxacin could not be conducted in humans with pneumonic plague. Thus, approval of this indication was based on efficacy studies conducted in animals. A risk-benefit assessment indicates that administration of ciprofloxacin to pediatric patients is appropriate (see “Administration”).
Interaction
Ciprofloxacin is an inhibitor of CYP1A2 isoenzyme of cytochrome P450. Concomitant use of ciprofloxacin with other drugs metabolized predominantly by CYP1A2 leads to increased plasma concentrations of these drugs and may lead to clinically significant adverse events.
Tizanidine. As a result of pharmacokinetic study with participation of healthy volunteers the concomitant administration of ciprofloxacin (500 mg 2 times daily for 3 days) and tizanidine (4 mg once daily) showed significant increase of tizanidine systemic exposure (Cmax by 7 times, AUC by 10 times). Simultaneous use of ciprofloxacin and tizanidine is contraindicated due to potentiation of hypotensive and sedative effects of tizanidine (see “Contraindications”).
Theophylline. Concomitant use of ciprofloxacin and theophylline may lead to an increased risk of adverse reactions in the patient, including CNS reactions. If concomitant use cannot be avoided, it is recommended to monitor theophylline serum concentrations continuously and to reduce theophylline dose if necessary (see “Precautions”).
Other xanthine derivatives. Concomitant use of ciprofloxacin and caffeine or pentoxifylline may result in decreased clearance, increased serum concentrations of xanthine derivatives and prolonged T1/2 from serum. Caution should be exercised and toxicity of xanthine should be monitored and the dose adjusted if necessary.
The drugs causing QT interval prolongation. Because ciprofloxacin may additionally prolong the QT interval, concomitant use of ciprofloxacin should be avoided in patients receiving drugs that prolong the QT interval (e.g., Class IA or Class III antiarrhythmic drugs, tricyclic antidepressants, macrolides, neuroleptics) (see “Precautions”).
Peroral hypoglycemic agents. Caution should be exercised when concomitant use of ciprofloxacin and oral hypoglycemic agents due to potentiation of the glucose-lowering effect. Severe hypoglycemia has been reported with concomitant use of ciprofloxacin and oral hypoglycemic agents, mainly sulfonylurea derivatives (e.g., glibenclamide, glimepiride). No fatal outcomes have been reported. Close monitoring of blood glucose levels is necessary (see “Side effects”).
Phenytoin. When concomitant use of ciprofloxacin and phenytoin, changes (increase or decrease) of phenytoin in blood serum have been observed. To avoid seizures associated with decreased phenytoin levels, and to prevent adverse events associated with phenytoin overdose when discontinuing ciprofloxacin, it is recommended to exercise caution and monitor phenytoin therapy in patients taking ciprofloxacin, including determination of serum phenytoin during the entire period of concurrent use and for a short time after completion of combined therapy.
Cyclosporine. When concomitant use of ciprofloxacin and cyclosporine, a transient increase in serum creatinine concentration has been observed. Caution should be exercised and renal function should be monitored (in particular, determination of blood creatinine concentration).
Anticoagulants. Concomitant use of ciprofloxacin and anticoagulants may lead to enhancement of their anticoagulant effect. The magnitude of this effect may vary depending on the infection, age and general condition of the patient, so it is difficult to assess the effect of ciprofloxacin on INR increase. Caution should be exercised and PV and INR should be monitored frequently when ciprofloxacin and oral anticoagulants (e.g., warfarin) are used together, and for a short time after completion of combined therapy.
Methotrexate. Concomitant use of methotrexate and ciprofloxacin may inhibit renal channel transport of methotrexate, which may be accompanied by increased plasma concentrations of methotrexate. This may increase the likelihood of side effects of methotrexate. Therefore, caution should be exercised: patients receiving methotrexate and ciprofloxacin concomitantly should be closely monitored.
Ropinirol. In a study involving 12 patients with Parkinson’s disease who received 6 mg of ropinirole once daily and 500 mg of ciprofloxacin twice daily, the Cmax and AUC of ropinirole were increased by 60 and 84%, respectively. Caution should be exercised when using ropinirole and ciprofloxacin concomitantly. It is recommended to monitor the side effects of ropinirole and adjust the dose accordingly when coadministered with ciprofloxacin and for a short time after completion of combined therapy.
Clozapine. When clozapine and ciprofloxacin were used concomitantly at a dose of 250 mg for 7 days, an increase in serum concentrations of clozapine and N-desmethylclozapine of 29 and 31%, respectively, was observed. Caution should be exercised, clozapine-associated adverse reactions should be closely monitored and the dosing regimen of clozapine should be adjusted if necessary during its co-administration with ciprofloxacin and for a short time after completion of combined therapy.
The NSAIDs. Combination of very high doses of quinolones and NSAIDs (excluding acetylsalicylic acid) may provoke seizures; use with caution.
Sildenafil. Simultaneous use in healthy volunteers of ciprofloxacin 500 mg and sildenafil in a single oral dose of 50 mg increased Cmax and AUC of sildenafil by approximately 2-fold. Therefore, caution and monitoring of sildenafil toxicity is necessary.
Duloxetine. In clinical trials it has been shown that concomitant use of duloxetine and strong CYP1A2 isoenzyme inhibitors (such as fluvoxamine) may increase AUC and Cmax of duloxetine by 5 and 2.5 times, respectively. Concomitant use of ciprofloxacin and duloxetine should be avoided. If this is not possible, monitoring of duloxetine toxicity is necessary.
Zolpidem. Concomitant use with ciprofloxacin may increase zolpidem blood levels, it is recommended to avoid concomitant use.
Probenecid. Probenecid slows down the rate of renal excretion of ciprofloxacin and increases its serum concentrations. Caution should be exercised when using ciprofloxacin and probenecid concomitantly (increased side effects of ciprofloxacin are possible).
Omeprazole. When using ciprofloxacin as a single dose of 1000 mg and omeprazole (40 mg once daily for 3 days) in 18 healthy volunteers AUC and Cmax of ciprofloxacin in blood were decreased by 20 and 23% respectively. The clinical significance of this interaction has not been determined.
Lidocaine. In a study involving 9 healthy volunteers, concomitant IV administration of lidocaine at a dose of 1.5 mg/kg and ciprofloxacin (500 mg twice daily) was shown to increase Cmax and AUC of lidocaine by 12 and 26%, respectively. Despite good tolerability of lidocaine, concomitant use with ciprofloxacin may result in increased side effects due to interaction.
Histamine H2-receptor antagonists do not seem to have a significant effect on the bioavailability of ciprofloxacin.
Metronidazole. Serum concentrations of ciprofloxacin and metronidazole do not change when used concomitantly.
Methoclopramide. Metoclopramide significantly accelerates absorption of ciprofloxacin when administered orally, which shortens the time to reach Cmax in plasma. No significant effect on the bioavailability of ciprofloxacin was observed.
Cationic drugs. Simultaneous oral administration of ciprofloxacin and cationic drugs, such as multivitamins, magnesium- and aluminum-containing antacids, sucralfate, polymeric phosphate-binding compounds (e.g. sevelamer, lanthanum carbonate) and drugs with high buffer capacity (e.g. didanosine), mineral supplements containing calcium, iron, zinc – reduces absorption of ciprofloxacin, which leads to lower serum and urine levels.
The simultaneous use of antacids containing magnesium hydroxide or aluminum hydroxide may decrease the bioavailability of ciprofloxacin by 90%.
In the cases listed above, ciprofloxacin should be taken either 2 h before or 6 h after taking such medications.
Eating food and dairy products. Simultaneous oral administration of ciprofloxacin and dairy products or beverages enriched with minerals (e.g., milk, yogurt, calcium-enriched juices) should be avoided, since absorption of ciprofloxacin may be reduced. Calcium in regular foods has no significant effect on absorption of ciprofloxacin.
Contraindications
Side effects
The following serious and important adverse reactions are detailed in the “Precautions” section:
Loss of function and potentially irreversible serious adverse reactions (see “Precautions”);
Tendinitis and tendon rupture (see “Precautions);
– peripheral neuropathy (see Precautions);
– effects on the CNS (see Precautions. “Precautions);
– aggravation of myasthenia gravis (see Precautions);
– other serious and sometimes fatal reactions (see Precautions.
– hypersensitivity reactions (see “Precautions”);
– hepatotoxicity (see “Precautions”).
– risk of aortic aneurysm and dissection (see “Precautions”);
– serious adverse reactions with concomitant use of theophylline (see “Precautions”).
– diarrhea associated with Clostridium difficile (see “Precautions”);
– QT interval prolongation (see “Precautions”).
– musculoskeletal disorders in children (see “Precautions”);
– photosensitivity/photototototoxicity (see “Precautions”). “
– development of drug-resistant bacteria (see “Precautions”).
The results of clinical trials
Because clinical trials are conducted with a different set of conditions, the frequency of adverse reactions observed in these clinical trials may not be the same as those obtained in other clinical trials and observed in clinical practice.
Adult patients
In clinical trials of oral and parenteral forms of ciprofloxacin, 49038 patients were treated.
The most common adverse reactions reported in clinical trials (regardless of dosage, duration of therapy, or indication) were nausea (2.5%), diarrhea (1.6%), abnormal liver function tests (1.3%) ), vomiting (1%), and rash (1%).
The clinically important adverse reactions seen in <1% of patients when treated with ciprofloxacin are listed below.
The body in general: headache, pain, including abdominal pain/discomfort.
CCS: fainting, angina pectoris, myocardial infarction, cardiac and respiratory arrest, tachycardia, hypotension.
CNS side: anxiety, dizziness, sleep disturbance, nightmares, hallucinations, paranoia, psychosis (toxic), manic reaction, irritability, tremor, ataxia, seizures (including epileptic status), malaise, anorexia, phobia, depersonalization, depression (potentially leading to self-harming behaviors such as suicidal acts/thoughts and attempted or successful suicide), paresthesia, abnormal gait, migraine.
Gastrointestinal organs: intestinal perforation, gastrointestinal bleeding, cholestatic jaundice, hepatitis, pancreatitis.
Hematopoietic and lymphatic system disorders: petechiae.
Metabolism and nutrition disorders: hyperglycemia, hypoglycemia.
Motor system disorders: arthralgia, joint stiffness, muscle weakness.
Urogenital system disorders: interstitial nephritis, renal failure.
Respiratory system: dyspnea, laryngeal edema, hemoptysis, bronchospasm.
Skin side/hypersensitivity: Anaphylactic reactions, including potentially life-threatening anaphylactic shock, erythema multiforme/Stevens-Johnson syndrome, exfoliative dermatitis, toxic epidermal necrolysis, pruritis, urticaria, photosensitivity/photototoxicity reactions, blood rush to face, fever, angioneurotic edema, erythema nodosa, sweating.
Sense organs: blurred vision, visual disturbances (chromatopsia and photopsia), decreased visual acuity, diplopia, tinnitus, decreased hearing, loss of sense of taste.
Pediatric patients
. The short-term (6 weeks) and long-term (1 year) safety of ciprofloxacin with respect to the musculoskeletal and nervous systems when administered orally or by IV was compared with cephalosporin in the treatment of complicated urinary tract infections and pyelonephritis in pediatric patients aged 1 to 17 years (mean age (6±4) years) in an international multicenter study. The duration of therapy ranged from 10 to 21 days (mean duration of treatment was 11 days, ranging from 1 to 88 days). A total of 335 patients who received ciprofloxacin and 349 patients who received the comparison drug were included.
The Independent Pediatric Safety Committee (IPSC) reviewed all cases of adverse musculoskeletal reactions, including abnormal gait or joint deviation on physical examination (baseline or requiring treatment). At 6 weeks after treatment initiation, musculoskeletal adverse reactions were noted in 9.3% (31/335) of patients receiving ciprofloxacin compared with 6% (21/349) of patients receiving the comparison drug. All musculoskeletal adverse reactions occurring within 6 weeks resolved (clinical resolution of signs and symptoms) usually within 30 days of treatment completion.
Radiological studies to confirm resolution of adverse reactions were not usually used. Patients who received ciprofloxacin were more likely to report more than one adverse reaction and more than one adverse reaction compared to control patients. The incidence of musculoskeletal side effects was consistently higher in the ciprofloxacin group compared with the control group in all age subgroups. At the end of 1 year, the incidence of these adverse reactions reported at any time during this period was 13.7% (46/335) in the ciprofloxacin group compared with 9.5% (33/349) in the comparison group, as shown in Table 2.
Table 2
Skeletal and musculoskeletal adverse reactions1 as assessed by IPSC
/p> Ciprofloxacin Comparison drug All patients (within 6 weeks) 31/335 (9.3%) 21/349 (6%) 95% CI2 (-0.8%, +7.2%) Age group 12-24 months 1/36 (2.8%) 0/41 2-6 years 5/124 (4%) 3/118 (2.5%) 6-12 years 18/143 (12.6%) 12/153 (7.8%) 12-17 years 7/32 (21.9%) 6/37 (16.2%) All patients (within 1 year) 46/335 (13.7%) 33/349 (9.5%) 95% CI2 (-0.6%, + 9.1%)
1 Adverse effects such as arthralgia, abnormal gait, abnormal joint condition on examination, sprained joints, leg pain, back pain, arthritis, bone pain, pain, myalgia, arm pain, and decreased range of motion in the joint (knee, elbow, ankle, hip, wrist, shoulder) were included.
2 The study was designed to demonstrate that the level of arthropathy in the ciprofloxacin group did not exceed that in the control group by more than + 6%. In both the 6-week and 1-year assessments, the 95% confidence CI showed that it could not be concluded that the ciprofloxacin group had comparable results to the control group.
The incidence of neurologic adverse reactions at 6 weeks from initiation of ciprofloxacin treatment was 3% (9/335) in the ciprofloxacin group compared with 2% (7/349) in the comparison group and included dizziness, nervousness, insomnia and somnolence.
In this study, the overall incidence of adverse reactions within 6 weeks of starting ciprofloxacin treatment was 41% (138/335) compared with 31% (109/349) in the comparison group. The most common adverse reactions were gastrointestinal, 15% (50/335) in patients treated with ciprofloxacin compared with 9% (31/349) in the comparison group.
Serious adverse reactions were seen in 7.5% (25/335) of patients receiving ciprofloxacin compared with 5.7% (20/349) of control group patients. Discontinuation of ciprofloxacin due to adverse effects was reported in 3% (10/335) of patients receiving ciprofloxacin compared with 1.4% (5/349) of comparison group patients. Other adverse reactions reported in at least 1% of patients receiving ciprofloxacin were diarrhea (4.8%), vomiting (4.8%), abdominal pain (3.3%), dyspepsia (2.7%), nausea (2.7%), fever (2.1%), asthma (1.8%) and rash (1.8%).
Short-term safety data for ciprofloxacin were also collected in a randomized, double-blind clinical trial in acute pulmonary exacerbations in patients with cystic fibrosis (ages 5 to 17 years). Sixty-seven patients received ciprofloxacin v/v at a dose of 10 mg/kg every 8 h for 1 week and then ciprofloxacin orally at a dose of 20 mg/kg every 12 h until completion of 10-21 days of treatment.
Musculoskeletal evaluations were performed periodically by non-treatment experts. Patients were observed for an average of 23 days after completion of treatment (range 0-93 days). Musculoskeletal adverse reactions were reported in 22% of patients, decreased range of motion in 12% of patients, and arthralgia in 10% of patients. The efficacy of ciprofloxacin for the treatment of acute pulmonary exacerbations in pediatric patients with cystic fibrosis has not been established.
In addition to adverse reactions reported in pediatric patients in clinical trials, adverse reactions reported in adults during clinical trials or postmarketing experience should also be expected to occur in pediatric patients.
Postmarketing experience
The following are adverse reactions that have been reported with fluoroquinolones, including ciprofloxacin. Because these cases are reported voluntarily, from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Systems side: prolongation of the QT interval, torsade de pointes, ventricular arrhythmias, vasculitis, hypertension.
CNS: myasthenia gravis, exacerbation of myasthenia gravis, peripheral neuropathy, polyneuropathy.
Visual disorders: eye twitching, nystagmus.
Gastrointestinal disorders: pseudomembranous colitis.
Hematopoietic and lymphatic system disorders: pancytopenia (life-threatening or fatal), methemoglobinemia.
Hepatic and biliary tract disorders: liver failure (including fatal cases).
Infections and invasions: candidiasis (oral, gastrointestinal, vaginal).
Studies: increased or decreased PV, increased cholesterol (serum), increased potassium (serum).
Musculoskeletal system: myalgia, myoclonus, tendinitis, tendon rupture.
Psychiatric disorders: agitation, confusion, delirium.
Skin disorders/hypersensitivity: acute generalized exanthematous pustulosis, fixed rash; serum-like reactions, anosmia.
Sensory organs: hyperesthesia, hypoesthesia, loss of taste.
Laboratory findings: hepatic – increased levels of ALT, AST, ALP, LDH, serum bilirubin; hematological – eosinophilia, leukopenia, decreased or increased levels of platelets, pancytopenia; renal – reported increases in serum creatinine, urea nitrogen, crystalluria, cylinduria and hematuria; Others – increased serum GGT levels, increased serum amylase levels, decreased blood glucose levels, increased uric acid levels, decreased Hb, anemia, bleeding diathesis, increased blood monocytes, and leukocytosis.
Overdose
Symptoms: in case of acute overdose, reversible renal toxicity has been reported in some cases.
Treatment: induction of vomiting, gastric lavage, administration of antacids containing magnesium, aluminum, calcium to reduce absorption of ciprofloxacin. Close monitoring of the patient’s condition and symptomatic therapy should be carried out, including monitoring of renal function, urine pH, and acidification if necessary, to prevent the development of crystalluria. Adequate fluid intake should be provided. Only a small amount (< 10%) of ciprofloxacin may be excreted by hemo- or peritoneal dialysis.
Pregnancy use
Pregnancy
Risk summary. Long-term experience with ciprofloxacin use in pregnant women (over several decades), based on available published information from case reports, case-control studies, and observational studies, indicates no drug-associated risk of serious birth defects, miscarriage, or adverse outcomes for the mother or fetus.
The available studies cannot definitively establish the absence of risk because they have methodological limitations, including small sample sizes, and some are nonspecific for ciprofloxacin.
The oral administration of ciprofloxacin at doses up to 100 mg/kg to pregnant female mice and rats during organogenesis and at doses up to 30 mg/kg to pregnant rabbits did not cause fetal malformations. These doses were 0.3; 0.6 and 0.4 times higher than MRDH in mice, rats, and rabbits, respectively, in terms of body surface area.
The estimated background risk of serious birth defects and miscarriage in women is unknown. In any pregnancy, there is a background risk of developing a birth defect, miscarriage, or other adverse outcomes. In the general population in the United States, the estimated baseline risk of serious birth defects and miscarriage in clinically determined pregnancies is 2-4% and 15-20%, respectively.
Breastfeeding
Risk summary. The published literature reports that ciprofloxacin is present in breast milk after IV and oral administration. There is no information on the effects of ciprofloxacin on milk production or on the infant. Because of the potential risk of serious adverse reactions in breastfed infants, including arthropathy, as shown in studies in young animals, breastfeeding is not recommended during treatment with ciprofloxacin for most indications and for an additional 2 days (5 T1/2 periods) after the last dose.
But in inhalational anthrax (after exposure), an assessment of the risks and benefits of continued breastfeeding while the mother (and possibly the baby) is receiving ciprofloxacin is necessary. Consideration should be given to the developmental and health benefits of breastfeeding, the clinical necessity of the mother’s use of ciprofloxacin, and the potential for side effects in the breastfed infant.
Clinical Warnings
Ciprofloxacin may cause changes in the gut flora of the infant. It is recommended that the breastfed infant be monitored for liquid or bloody stools and candidiasis (thrush, diaper rash).
Similarities
| Shelf life | See package insert. |
|---|---|
| Conditions of storage | Store in a dark place at 5 ° to 20 ° C out of the reach of children. Do not freeze! |
| Manufacturer | Ozon, Russia |
| Medication form | pills |
| Brand | Ozon |
Other forms…
Related products
Buy Ciprofloxacin, 500 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.