No products in the cart.
Chloe, 28 pcs.
€23.91 €19.93
Out of stock
(E-mail when Stock is available)
EAN: 3582910090885
SKU: 211598
Categories: Contraceptive, Gynecology and Obstetrics, Hormonal, Medicine
Description
Pharmacodynamics
A combined low-dose monophasic oral contraceptive with antiandrogenic activity. The mechanism of action is due to its constituent antiandrogenic steroid drug, cyproterone acetate, and the oral estrogen, ethinyl estradiol.
Cyproterone acetate
It has the ability to competitively bind to natural androgen receptors (including testosterone, dihydroepiandrosterone, androstenedione) formed in small quantities in women, mainly in the adrenal glands, ovaries and skin. By blocking androgen receptors in target organs, it reduces androgenization phenomena in women (due to disruption of processes mediated by hormone-receptor complexes at the level of main intracellular mechanisms). Thus it becomes possible to treat diseases caused by increased formation of androgens or specific sensitivity to these hormones.
In the course of taking the drug the increased activity of sebaceous glands, which play an important role in the occurrence of acne and seborrhea, is reduced. After 3-4 months of therapy the existing rash usually disappears. Excessive greasiness of hair and skin disappears even earlier. Hair loss, which often accompanies seborrhea, is also reduced.
Therapy with Chloe® in women of reproductive age reduces clinical manifestations of mild forms of hirsutism; however, the effect of treatment should be expected only after several months of use.
In addition to its antiandrogenic properties, cyproterone acetate has gestagenic activity mimicking that of corpus luteum hormone. It inhibits secretion of gonadotropic hormones by pituitary gland and inhibits ovulation, which determines contraceptive effect.
Ethinylestradiol
Entinylestradiol enhances the central and peripheral effects of cyproterone acetate on ovulation, preserves the high viscosity of cervical mucus, making it difficult for sperm to enter the uterine cavity and contributing to a reliable contraceptive effect.
With this drug the cycle becomes more regular, painful menstrual periods are less frequent, bleeding intensity decreases, and the risk of iron deficiency anemia decreases.
Pharmacokinetics
Cyproterone acetate
Intake
Intake/p>
After oral administration, cyproterone acetate is completely absorbed from the gastrointestinal tract. Cmax in plasma is reached after 1.6 h and is 15 ng/ml. Bioavailability is 88%.
Distribution
Ciproterone acetate is almost completely bound to plasma albumin, approximately 3.5-4% is free. Because binding to proteins is non-specific, changes in sex steroid-binding globulin (SBSG) levels do not affect the pharmacokinetics of cyproterone acetate.
Metabolism
Biotransformed by hydroxylation and conjugation, the main metabolite is the 15b-hydroxyl derivative.
Elevation
The pharmacokinetics of cyproterone acetate is biphasic: T1/2 is 0.8 h and 2.3 days for the first and second phases, respectively. Total plasma clearance is 3.6 ml/min/kg. It is excreted mainly as metabolites by the kidneys and through the intestine at a ratio of 1:2, a small part is excreted unchanged through the intestine. Up to 0.2% of the dose of cyproterone acetate is excreted with breast milk. T1/2 for cyproterone acetate metabolites is 1.8 days.
Ethinylestradiol
Intake
After drug administration, ethinylestradiol is quickly and completely absorbed from the gastrointestinal tract. Cmax is approximately 80 pg/mL and is reached after 1.7 h. Bioavailability is about 45%, has considerable individual variability.
Distribution
The binding to plasma proteins (albumin) is high: only 2% are free in plasma.
Ethinylestradiol increases hepatic synthesis of HSPC and corticosteroid-binding globulin (CRBG) with continuous use. With Chloe® treatment, serum HSPC concentration increases from approximately 100 nmol/L to 300 nmol/L and serum CRC concentration increases from approximately 50 µg/mL to 95 µg/mL.
Metabolism
In the process of absorption and “first passage” through the liver, ethinylestradiol undergoes extensive metabolism.
Elimination
The pharmacokinetics of ethinylestradiol are biphasic: T1/2 1-2 h and approximately 20 h, respectively. Plasma clearance is about 5 ml/min/kg. Ethinylestradiol is excreted from the body as metabolites: about 40% – by the kidneys, 60% – through the intestine. With the breast milk is excreted up to 0.02% of the dose of ethinylestradiol.
Indications
Indications
Androgen-dependent diseases in women:
Active ingredient
Active ingredient
Composition
Composition
Yellow-orange film-coated tablets (21 pcs. in blister).
1 tablet contains:
Active substances:
Ethinylestradiol 35 mcg,
Ciproterone acetate 2 mg.
Associates:
Lactose monohydrate – 68.8 mg,
povidone – 2 mg,
sodium carboxymethyl starch (type A) – 1.5 mg,
colloidal anhydrous silica – 0.188 mg,
aluminum colloidal oxide – 0.04 mg,
magnesium stearate – 0.375 mg.
Composition of the shell:
Opadry II Yellow OY-L-32901 (Opadry II Yellow OY-L-32901) dye – 3 mg (lactose monohydrate, hypromellose 2910, titanium dioxide, macrogol 4000, iron oxide yellow, iron oxide black, iron oxide red, purified water).
Tablets (placebo) white (7 pieces in blister).
Auxiliary substances:
Lactose monohydrate,
povidone,
sodium carboxymethyl starch (type A),
colloidal anhydrous silicon dioxide,
colloidal aluminum oxide,
magnesium stearate.
There are 28 tablets in the blister.
The film-coated tablets are 21 yellow-orange in a blister.
Tablets (placebo) of white color 7 pieces in a blister.
There is 1 blister in the carton pack.
How to take, the dosage
How to take, the dosage
The drug should be taken orally in 1 tablet/day. The tablet is taken without chewing and with a small amount of liquid. It is recommended to take the drug at the same time, preferably after breakfast or dinner.
The use of Chloe® starts on day 1 of the cycle using the tablet of the corresponding day of the week from the calendar package. Daily intake of the drug is carried out using the tablets from the calendar pack in the direction of the arrow on the foil, until all the tablets are taken. After all of the yellow-orange tablets in the calendar pack have been taken, the remaining white tablets must be taken for the next 7 days.
In the last 7 days of the treatment cycle (28 days), menstrual-like bleeding should occur (as a result of treatment withdrawal). Menstruation usually begins 2-3 days after the 21st day of the treatment cycle with the drug.
The next package must be started the day after taking the pills from the previous package completely finished, regardless of whether bleeding continues/continues.
When switching from combined oral contraceptives, Chloe® should be started the day after taking the last tablet with the active ingredients of the previous drug, but in no case later than the day after the usual 7-day interval of taking (for products containing 21 pills). Continue as described above.
If the patient has taken the previous contraceptive daily for 28 days, Chloe® should be started after taking the last inactive pill.
When switching from a contraceptive containing only gestagens (“mini-pills”), Chloe® can be started without interruption.
When using injectable forms of contraceptives, Chloe® should be used from the day the next injection is due.
When switching from an implant, Chloe® should be used as early as the day it is removed.
In all cases, an additional barrier method of contraception should be used for the first 7 days of use.
After a first trimester abortion a woman may begin using Chloe® immediately. In this case there is no need for additional contraceptive methods.
After childbirth or a second trimester abortion, the use of the drug should be started on days 21-28. If administration is started later, an additional barrier method of contraception should be used for the first 7 days of the drug.
If a woman was sexually active between childbirth or abortion and the start of the drug, pregnancy should be excluded first, or the first menstrual period should be awaited.
The missed pill should be taken as soon as possible, the next pill should be taken at the usual time. Late < 12 hours late does not reduce the reliability of contraception. If the delay in taking the pill is > 12 h, the reliability of contraception may be reduced.
If pills are late > 12 h (interval from last pill > 36 h) during weeks 1 and 2 of taking the drug, a woman should take the last missed pill as soon as possible: even if this means taking two pills at once. The next pill should be taken at the usual time. Additionally, a barrier method of contraception should be used for the next 7 days.
If a delay in taking the pill is > 12 h (interval from taking the last pill > 36 h) during week 3 of the drug, the woman should take the last missed pill as soon as possible: even if it means taking two pills at the same time. The next pill should be taken at the usual time. Taking a pill from a new pack should be started, at the end of the current pack – without interruption. It is likely that you will not have a bleeding discontinuation until the end of the second package, but there may be a bleeding discontinuation or uterine breakthrough bleeding on the days you take the pills.
If a woman has vomited within 3 to 4 hours after taking the drug, absorption of the active ingredients may be incomplete. In this case, it is necessary to be guided by the recommendations for skipping the pill.
In order to delay the start date of her period, a woman should continue taking pills from a new package of the drug immediately after taking all pills from the previous package, without interruption. The pills from the new pack can be taken as long as the woman wishes (until the pack runs out). While taking the pills from the second package, the woman may experience menses or breakthrough uterine bleeding. The pills in the next package should be started after all 28 pills have been taken.
In order to postpone the day her period starts to another day of the week, a woman should shorten the nearest interval between the pills by as many days as she wants. The shorter the interval, the higher the risk that she won’t have a bleeding withdrawal and, subsequently, will have a smeary, bleeding breakthrough while taking her second pack (just like when she would want to delay the start of her period).
In the treatment of hyperandrogenic conditions, the duration of use of the drug is determined by the severity of the disease. After disappearance of symptoms it is recommended to take the drug for at least 3-4 months. If a relapse occurs several weeks or months after completion of the course, retreatment with Chloe® may be repeated.
Interaction
Interaction
The simultaneous use of Chloe® with microsomal liver enzyme inducers (hydantoins, barbiturates, primidone, carbamazepine and rifampicin; and possibly oxcarbazepine, topiramate, felbamate, and griseofulvin) increase the clearance of ethinylestradiol and ciproterone, which may lead to breakthrough uterine bleeding or decreased contraceptive reliability.
Concomitant use with ampicillin, rifampicin, and tetracyclines decreases the contraceptive reliability of Chloe®.
Special Instructions
Special Instructions
Before starting Chloe® administration, a general medical examination should be performed (including breast and cervical mucus cytology), pregnancy and clotting disorders should be excluded. During long-term use of the drug, prophylactic control examinations should be performed every 6 months.
If there are any risk factors, the potential risk and expected benefits of therapy should be carefully evaluated and discussed with the woman before initiating treatment.
The estimated incidence of venous thromboembolism (VTE) with low-dose estrogen oral contraceptives ( < 50 µg ethinyl estradiol) is up to 4/10,000 women per year compared to 0.5-3/10,000 women not taking oral contraceptives. And the incidence of VTE with combined oral contraceptives is lower than the incidence of VTE associated with pregnancy (6/10,000 pregnant women per year).
The patient should be warned that if symptoms of venous or arterial thrombosis develop, she should see a physician immediately. These symptoms include unilateral leg pain and/or swelling, sudden severe chest pain with or without irradiation to the left arm, sudden shortness of breath, sudden coughing fits, any unusual, severe, prolonged headache, increased frequency and severity of migraines, sudden partial or complete loss of vision, Diplopia, slurred speech or aphasia, dizziness, collapse with/without partial seizure, weakness or very significant loss of sensation, sudden on one side or in one part of the body, motor disturbances, acute abdominal symptoms.
The relationship between the use of combined oral contraceptives and arterial hypertension has not been established. If persistent arterial hypertension occurs, the drug should be discontinued and appropriate hypotensive therapy should be prescribed. The contraceptive may be continued with normalization of BP.
If liver function abnormalities occur, temporary withdrawal of the drug may be required until normalization of laboratory parameters.
Recurrent cholestatic jaundice developing for the first time during pregnancy or during previous use of sex hormones requires discontinuation of combined oral contraceptives.
While combined oral contraceptives affect tissue insulin resistance and glucose tolerance, it is not usually necessary to adjust the dose of hypoglycemic drugs in patients with diabetes. Nevertheless, this category of patients should be closely monitored.
Women who are prone to chloasma should avoid prolonged sun exposure and exposure to ultraviolet radiation while taking combined oral contraceptives.
If women with hirsutism have recently developed symptoms or have significantly worsened, other causes such as androgen-producing tumor, congenital adrenal cortex dysfunction should be considered in making a differential diagnosis.
The use of Chloe® may cause irregular bleeding (smear-like discharge or breakthrough bleeding), especially during the first months of therapy. Therefore, any irregular bleeding should be evaluated only after an adjustment period of approximately 3 cycles.
If irregular bleeding recurs or develops after previous regular cycles, non-hormonal causes should be considered and adequate diagnostic measures (including diagnostic curettage) should be performed to rule out malignancy or pregnancy.
In some cases, bleeding withdrawal may not develop during a break in use. If the pills are taken irregularly or if there are no two consecutive menstrual-like bleeding events, pregnancy should be ruled out before continuing the drug.
There may be changes in skin allergy tests and decreased concentrations of LH and FSH during the use of the drug.
With regard to the fact that the full contraceptive effect is seen by day 7 after the start of the drug, additional non-hormonal methods of contraception are recommended in the first week.
The use of the drug after childbirth is not recommended before the first normal menstrual cycle has passed.
The treatment should be stopped immediately 3 months before the planned pregnancy and approximately 6 weeks before the planned surgical intervention, with prolonged immobilization.
In case of diarrhea and vomiting the contraceptive effect decreases (additional non-hormonal methods of contraception should be used without stopping the drug).
Smoking women who take hormonal contraceptive drugs have an increased risk of vascular disease with serious consequences (myocardial infarction, stroke). The risk increases with age and according to the number of cigarettes smoked (especially in women over 30).
Contraindications
Contraindications
Side effects
Side effects
Endocrine system: rarely – engorgement, soreness, increase and discharge from the mammary glands, weight gain.
Perior genital system disorders: rarely – intermenstrual bleeding, changes in the vaginal secretion, changes in libido.
CNS disorders: rarely – headache, migraine, decreased mood.
The digestive system: rarely – nausea, vomiting, gastralgia.
Others: very rare – poor tolerance of contact lenses, edema of the eyelids, visual impairment, conjunctivitis, decreased hearing, allergic reactions, thrombophlebitis, thromboembolism, generalized itching, jaundice, appearance of pigment spots on the face (chloasma).
The side effects listed may occur in the first few months of treatment and usually decrease with time.
Overdose
Overdose
Symptoms: nausea, vomiting, slight vaginal bleeding.
Treatment: symptomatic therapy is carried out. There is no specific antidote.
Pregnancy use
Pregnancy use
The drug is contraindicated in pregnancy, suspected pregnancy and during breastfeeding.
Similarities
Similarities
Additional information
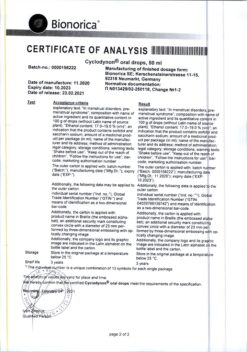
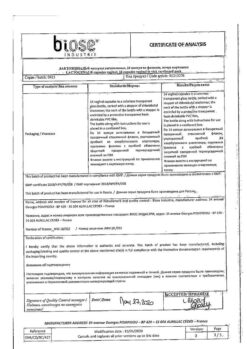
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Store out of reach of children at temperatures under 25°C. |
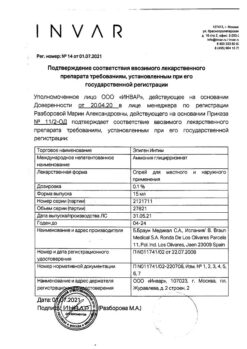
| Manufacturer | Laboratorios Leon Pharma S.A., Spain |
| Medication form | pills |
| Brand | Laboratorios Leon Pharma S.A. |
Related products
Buy Chloe, 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.