No products in the cart.
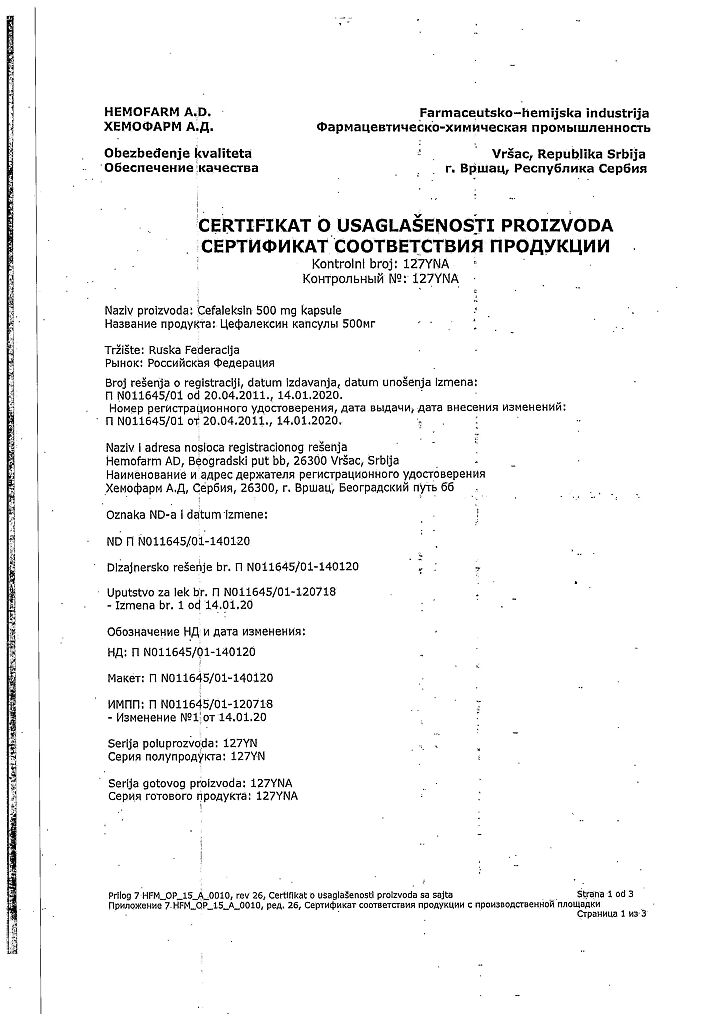
Cephalexin, 500 mg capsules 16 pcs
€3.36 €3.05
Out of stock
(E-mail when Stock is available)
Description Pharmacotherapeutic group: Antibiotic cephalosporin Pharmacodynamics: Pharmacokinetics:
ATX: J01DB01 Cephalexin
A first generation cephalosporin antibiotic. It acts bactericidally, disrupts the synthesis of the cell wall of microorganisms. It is sufficiently resistant to penicillinases of gram-positive microorganisms, it is destroyed by beta-lactamases of gram-negative microorganisms.
Cephalexin is active against the following microorganisms in vitro: β-hemolytic streptococcus, Staphylococcus spp. (including coagulase-positive, coagulase-negative and penicillinase-producing strains). Streptococcus pneumoniae, Escherichia coli, Proteus mirabilis, Klebsiella spp., Haemophilus influenzae, Branhamella catarrhalis.
Cephalexin is active against Neisseria meningitidis, Neisseria gonorrhoeae, Shigella spp., Salmonella spp. but the clinical significance of this fact is limited. Ineffective against Enterococcus spp. (Enterococcus faecalis), Morganella morganii, Proteus vulgaris, Pseudomonas aeruginosa or Acinetobacter calcoaceticus, Serratia marcescens, Clostridium spp., Bacteroides fragilis.
He is not sensitive to cephalexin for methicillin-resistant staphylococci (in vitro), i.e. there is cross-resistance.
It is rapidly and well absorbed after oral administration. Bioavailability is 90-95%, eating slows absorption but does not affect its completeness.
The time to maximum concentration (TCmax) after oral administration of 0.25, 0.5 or 1 g is 1 h, the value of maximum concentration (Cmax) is 9, 18 and 32 mcg/ml, respectively. Therapeutic concentration is maintained for 4-6 hours.
The binding to plasma proteins is 10-15%. Volume of distribution is 0.26 l/kg.
It is distributed relatively evenly in different tissues and body fluids: lungs, liver, heart, kidneys, bile, gall bladder, bones, joints, respiratory tract. Passes poorly through the unchanged blood-brain barrier. It passes through the placenta, is excreted in small amounts with breast milk and is found in amniotic fluid. It is not metabolized.
Half-life (T1/2) is 0.9-1.2 hours. Total clearance is 380 ml/min.
Extracted by kidneys – 70-89% unchanged (2/3 – by glomerular filtration, 1/3 – by tubular secretion); in bile – 0.5%. Renal clearance is 210 ml/min. In case of impaired renal excretory function the blood concentration increases and the time of renal excretion lengthens. T1/2 after oral administration is 5-30 hours.
It is moderately excreted by hemodialysis and well excreted by peritoneal dialysis.
.
Indications
Indications
Infectious and inflammatory diseases caused by microorganisms sensitive to cephalexin: infections of the upper and lower respiratory tract (bronchitis, pneumonia, bronchopneumonia, pleural empyema and lung abscess); ENT organs (pharyngitis, otitis media, sinusitis, tonsillitis); genitourinary system (pyelonephritis, cystitis, urethritis, prostatitis, epididymitis, endometritis, gonorrhea, vulvovaginitis); skin and soft tissues (furunculosis, abscess, phlegmon, pyoderma, lymphadenitis, lymphangitis); bones and joints (including osteomyelitis).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Antibiotic-cephalosporin
ATX: J01DB01 Cephalexin
Pharmacodynamics:
First generation cephalosporin antibiotic. It has a bactericidal effect and disrupts the synthesis of the cell wall of microorganisms. Quite resistant to penicillinases of gram-positive microorganisms, destroyed by beta-lactamases of gram-negative microorganisms.
Cephalexin is active against the following microorganisms in vitro: β-hemolytic streptococcus, Staphylococcus spp. (including coagulase-positive, coagulase-negative and penicillinase-producing strains). Streptococcus pneumoniae, Escherichia coli, Proteus mirabilis, Klebsiella spp., Haemophilus influenzae, Branhamella catarrhalis.
Cephalexin is active against Neisseria meningitidis, Neisseria gonorrhoeae, Shigella spp., Salmonella spp., however, the clinical significance of this fact is limited. Ineffective against Enterococcus spp. (Enterococcus faecalis), Morganella morganii, Proteus vulgaris, Pseudomonas aeruginosa or Acinetobacter calcoaceticus, Serratia marcescens, Clostridium spp., Bacteroides fragilis.
Methicillin-resistant staphylococci are not sensitive to cephalexin (in vitro), i.e. cross-resistance occurs.
Pharmacokinetics:
After oral administration, it is quickly and well absorbed. Bioavailability is 90-95%, food intake slows down absorption, but does not affect its completeness.
The time to reach the maximum concentration (TCmax) after oral administration of 0.25, 0.5 or 1 g is 1 hour, the value of the maximum concentration (Cmax) is 9, 18 and 32 μg/ml, respectively. The therapeutic concentration is maintained for 4-6 hours.
Communication with plasma proteins is 10-15%. Volume of distribution – 0.26 l/kg.
Distributed relatively evenly in various tissues and body fluids: lungs, liver, heart, kidneys, bile, gall bladder, bones, joints, respiratory tract. It penetrates poorly through the unchanged blood-brain barrier. Passes through the placenta, is excreted in small quantities in breast milk, and is found in amniotic fluid. Not metabolized.
Half-life (T1/2) – 0.9-1.2 hours. Total clearance – 380 ml/min.
Excreted by the kidneys – 70-89% unchanged (2/3 – by glomerular filtration, 1/3 by tubular secretion); with bile – 0.5%. Renal clearance – 210 ml/min. If the excretory function of the kidneys is impaired, the concentration in the blood increases, and the time of excretion by the kidneys lengthens. T1/2 after oral administration – 5-30 hours.
Moderately excreted by hemodialysis, well by peritoneal dialysis.
Special instructions
Special instructions
Before starting treatment with cephalexin, it is necessary to obtain a detailed history regarding previous hypersensitivity reactions to penicillins, cephalosporins or other substances that cause an allergic reaction in the patient. Patients with a history of allergic reactions to penicillins and carbapenems may have increased sensitivity to cephalosporin antibiotics. If an allergic reaction develops, treatment with the drug should be stopped and appropriate measures taken.
Cases of pseudomembranous colitis have been described when taking antibiotics, the severity of which can vary from mild to life-threatening. Therefore, it is necessary to carry out a differential diagnosis of pseudomembranous colitis in patients with diarrhea that occurs during or after a course of antibiotic treatment. If diarrhea is prolonged or severe or the patient experiences abdominal cramps, treatment with the drug should be stopped immediately and the patient should be examined. You should not use medications that inhibit intestinal motility.
Cases of acute generalized exanthematous pustulosis occurring during treatment with cephalexin have been described. When prescribing the drug, patients should be informed of the signs and symptoms of acute generalized exanthematous pustulosis and closely monitored for skin reactions. If skin reactions characteristic of acute generalized exanthematous pustulosis develop, treatment with cephalexin should be stopped immediately. A significant proportion of cases of acute generalized exanthematous pustulosis were recorded during the first week of therapy.
Long-term use of cephalexin may lead to overgrowth of resistant microorganisms. If superinfections develop during treatment, appropriate measures must be taken.
During treatment with cephalexin, a positive direct Coombs test is possible. When treated with the drug, false-positive results for determining glucose in urine may be observed in tests based on the reduction of copper ions (with Benedict’s or Fehling’s solutions or with Clinitest tablets).
During the treatment period, it is not recommended to consume ethanol.
In patients with impaired renal function, accumulation is possible (adjustment of the dosage regimen is required).
In staphylococcal infections, cross-resistance exists between cephalosporins and isoxazolylpenicillins.
Impact on the ability to drive vehicles. Wed and fur.:
During the period of use of the drug, patients should be especially careful when driving and engaging in other potentially hazardous activities due to possible adverse reactions from the central nervous system, such as dizziness, agitation, convulsions, and hallucinations.
Active ingredient
Active ingredient
Cephalexin
Composition
Composition
Each capsule contains:
Active substance:
Cephalexin monohydrate (in terms of cephalexin) – 250 mg;
Excipients:
Methylcellulose (methocel A15) – 4.2 mg, calcium stearate monohydrate – 3 mg, potato starch – up to the weight of the capsule contents 300 mg;
Capsule composition: gelatin – 80.751 mg, glycerol – 0.122 mg, purified water – 13.92 mg, methyl parahydroxybenzoate – 0.35 mg, propyl parahydroxybenzoate – 0.089 mg, titanium dioxide – 0.644 mg, sodium lauryl sulfate – 0.056 mg, sunset yellow dye E110 – 0.013 mg, quinoline yellow dye E104 – 0.055 mg.
Pregnancy
Pregnancy
The use of the drug during pregnancy is possible only if the expected benefit to the mother outweighs the potential risk to the fetus.
If it is necessary to use the drug during breastfeeding, breastfeeding should be discontinued.
Contraindications
Contraindications
Hypersensitivity (including to other beta-lactam antibiotics), children under 10 years of age (for this dosage form).
With caution:
Renal failure, pseudomembranous colitis (history).
Side Effects
Side Effects
Allergic reactions: rash, urticaria, Quincke’s edema, erythema multiforme, eosinophilia, toxic epidermal necrolysis, Stevens-Johnson syndrome, anaphylactic shock.
From the skin: acute generalized exanthematous pustulosis.
From the digestive system: abdominal pain, dry mouth, anorexia, nausea, vomiting, diarrhea, flatulence, gastritis, toxic hepatitis, cholestatic jaundice, increased activity of liver transaminases and alkaline phosphatase, increased bilirubin concentration, intestinal candidiasis, oral cavity, pseudomembranous colitis.
From the nervous system: dizziness, weakness, headache, agitation, hallucinations, convulsions.
From the genitourinary system: interstitial nephritis, itching of the genitals and anus, vaginitis, vaginal discharge, genital candidiasis.
From the hematopoietic organs: leukopenia, neutropenia, thrombocytopenia, pancytopenia, agranulocytosis, aplastic anemia, hemolytic anemia.
From the musculoskeletal system: arthralgia, arthritis.
Laboratory indicators: increase in prothrombin time.
Other: fever.
Interaction
Interaction
When used simultaneously with furosemide. ethacrynic acid, nephrotoxic antibiotics (for example, aminoglycosides, polymyxins), phenylbutazone increases the risk of kidney damage.
Medicines that reduce tubular secretion increase the concentration of the drug in the blood and slow down its elimination.
When used simultaneously with metformin, dose adjustment of the latter may be required.
Salicylates and indomethacin slow down the elimination of cephalexin.
Reduces the prothrombin index, enhances the effect of indirect anticoagulants.
Hypokalemia has been described in a patient with leukemia taking cytotoxic drugs when prescribed gentamicin and cephalexin.
Overdose
Overdose
Symptoms: Vomiting, nausea, epigastric pain, diarrhea, hematuria.
Treatment: Activated carbon, maintaining airway patency, monitoring vital functions: blood gas composition, electrolyte balance.
Storage conditions
Storage conditions
In a place protected from light, at a temperature of 2-25°C.
Shelf life
Shelf life
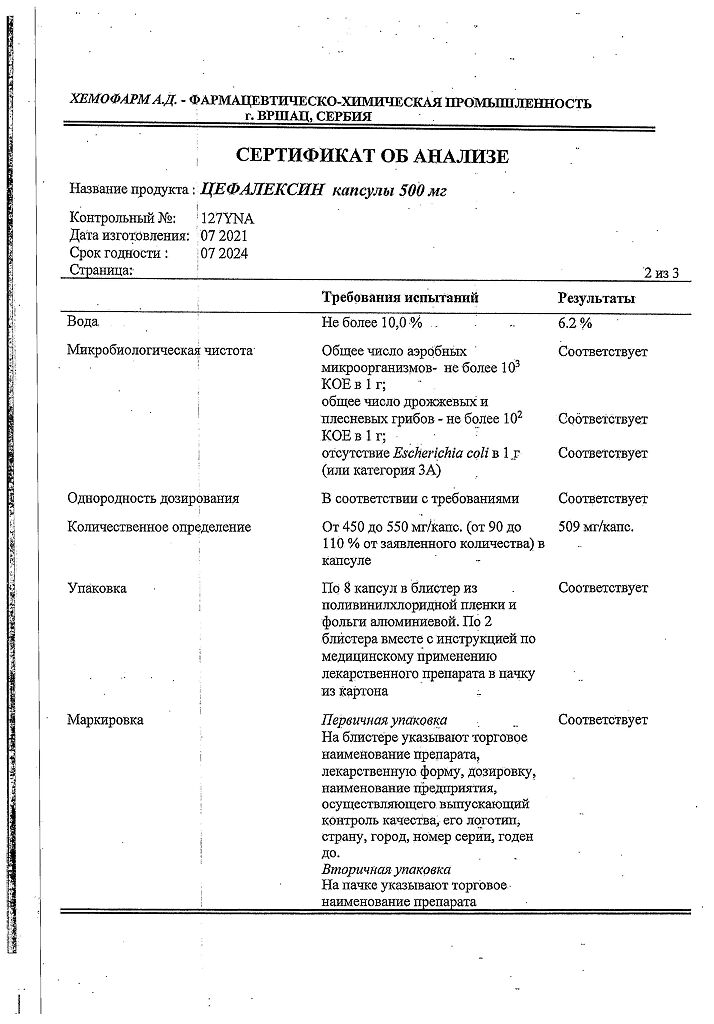
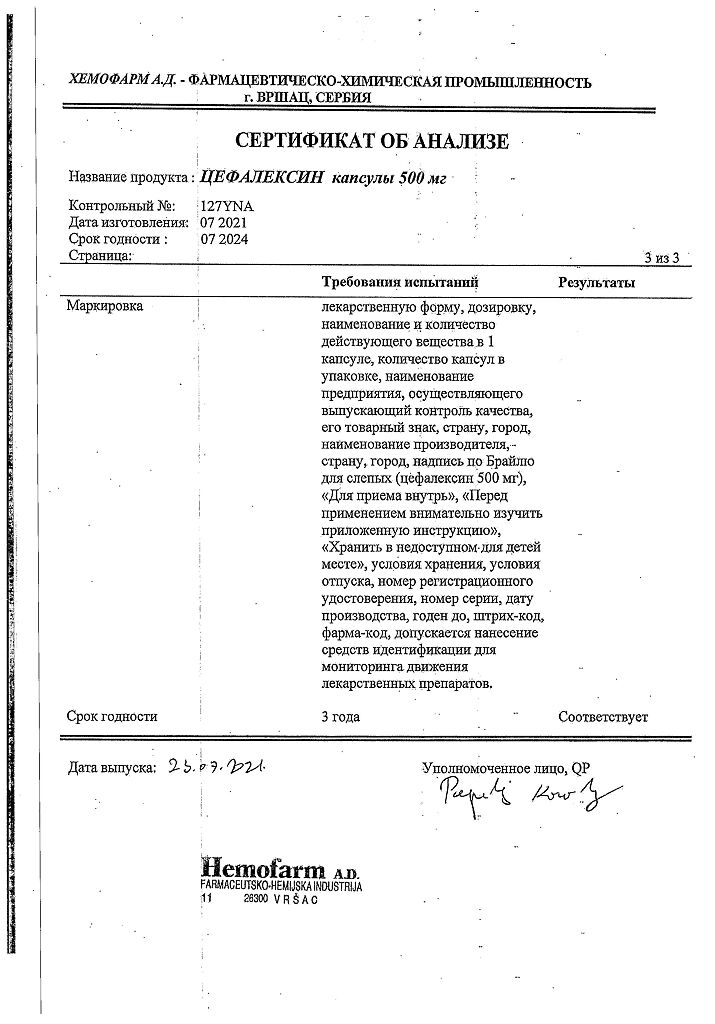
3 years.
Manufacturer
Manufacturer
Hemomont D.O.O, Montenegro
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | In a light-protected place at 2-25°C. |
| Manufacturer | Chemomet D.O.O., Montenegro |
| Medication form | capsules |
| Brand | Chemomet D.O.O. |
Related products
Buy Cephalexin, 500 mg capsules 16 pcs with delivery to USA, UK, Europe and over 120 other countries.