No products in the cart.
Description
The drug Ceftazidime is an antibacterial drug of III generation cephalosporins group, it has a broad spectrum and acts bactericidally, disrupts cell wall synthesis of microorganisms, resistant to the action of most beta-lactamases. The drug is active against Gram-negative microorganisms: Haemophilus influenzae, Neisseria gonorrhoeae and other Neisseria spp. and most representatives of the family Enterobacteriaceae (Citrobacter spp., Enterobacter spp., Escherichia coli, Klebsiella pneumoniae and other Klebsiella spp, Morganella morganii and other Morganella spp., Proteus mirabilis (including indole-positive), Proteus vulgaris and other Proteus spp., Providena rettgeri and other Providena spp. and Serratia spp.), Acinetobacter spp., Haemophilus parainfluenzae (including ampicillin-resistant strains), Pasteurella multocida. Salmonella spp., Shigella spp. and Yersinia enterocolitica.
The drug ceftazidime has the highest activity among III generation cephalosporins against Pseudomonas aeruginosa and intrahospital infection. The drug is active against Gram-positive bacteria: Micrococcus spp., Streptococcus aureus, Streptococcus mitis, Streptococcus pneumoniae, Streptococcus pyogenes group A, Streptococcus viridans and other Streptococcus spp. (excluding Streptococcus faecalis); strains sensitive to methicillin: Staphylococcus aureus, Staphylococcus epidermidis.
The drug Ceftazidime is active against anaerobic bacteria: Bacteroides spp. (most strains of Bacteroides fragilis are resistant), Clostridium perfringens, Peptococcus spp., Peplostreptococcus spp. and Propionobacterium spp. The drug is not active against methicillin-resistant strains of Campilobacter spp., Chlamydia spp., Clostridium difficile, Enterococcus spp., Listeria monocytogenes and other Lisleria spp., Staphylococcus aureus and Staphylococcus epidermidis; Streptococcus faecalis.
Pharmacokinetics
After administration, the drug is rapidly distributed in the human body and reaches therapeutic concentrations in most tissues and fluids, including synovial, pericardial and peritoneal fluid as well as in bile, sputum and urine. Distribution also occurs in bones, myocardium, gallbladder, skin and soft tissues at concentrations sufficient to treat infectious diseases, especially in inflammatory processes that increase diffusion of the drug. It penetrates poorly through the intact blood-brain barrier, but the therapeutic level reached by the drug in the cerebrospinal fluid is sufficient to treat meningitis.
It binds irreversibly with plasma proteins (less than 15%), and has bactericidal effect only in free form. The degree of binding to proteins does not depend on the concentration. Maximal concentration after intramuscular introduction of 0.5 g or 1 g is 17 mkg/ml and 39 mkg/ml, when administered intravenously it is 42 mkg/ml and 69 mkg/ml, respectively. Time of reaching maximum concentration when administered intramuscularly is 1 h, when administered intravenously – by the end of the infusion. The drug concentration equal to 4 µg/ml is maintained for 6-8 hours. Therapeutic concentration in plasma is maintained for 8-12 hours.
Half-life in normal renal function is 1.8 hours; in impaired renal function 2.2 hours. The drug is not metabolized in the liver, hepatic dysfunction does not affect the pharmacodynamics and pharmacokinetics of the drug. The dose in such patients remains normal. It is excreted unchanged by the kidneys up to 80-90% (70% of the administered dose is excreted in the first 4 hours) during 24 hours by glomerular filtration and tubular secretion to an equal extent.
In case of impaired renal function it is recommended to reduce the dose. The volume of distribution is 0.21-0.28 l/kg. The drug accumulates in the soft tissues, kidneys, lungs, bones and joints, serous cavities.
Indications
Indications
Infectious and inflammatory diseases caused by microorganisms sensitive to the drug:
severe infections, including nosocomial infections (septicemia, bacteremia, peritonitis, meningitis, infections in patients with reduced immunity, infected burns);
urinary tract infections (acute and chronic pyelonephritis, pyelitis, prostatitis, cystitis, urethritis /bacterial only/, kidney abscess);
lower respiratory tract infections (acute and chronic bronchitis, infected bronchiectasis, pneumonia caused by gram-negative bacteria, lung abscess, pleural empyema, lung infections in patients with cystic fibrosis);
infections of the skin and soft tissues (mastitis, wound infections, skin ulcers, cellulitis, erysipelas);
infections of bones and joints (septic arthritis, osteomyelitis, bacterial bursitis);
infections of the gastrointestinal tract, abdominal cavity and biliary tract (enterocolitis, retroperitoneal abscesses, diverticulitis, pelvic inflammation, cholecystitis, cholangitis, gallbladder empyema);
infections of the pelvic organs and female genital organs;
gonorrhea (especially with hypersensitivity to antibacterial drugs from the penicillin group);
infections of the ear, nose and throat (otitis media, sinusitis, mastoiditis).
Pharmacological effect
Pharmacological effect
The drug Ceftazidime is an antibacterial drug from the group of third-generation cephalosporins, has a broad spectrum and is bactericidal, disrupts the synthesis of the cell wall of microorganisms, and is resistant to the action of most beta-lactamases. The drug is active against gram-negative microorganisms: Haemophilus influenzae, Neisseria gonorrhoeae and other Neisseria spp. and most representatives of the family Enterobacteriaceae (Citrobacter spp., Enterobacter spp., Escherichia coli, Klebsiella pneumoniae and other Klebsiella spp., Morganella morganii and other Morganella spp., Proteus mirabilis (including indole-positive), Proteus vulgaris and other Proteus spp., Providenсia rettgeri and other Providenсia spp. and Serratia spp.), Acinetobacter spp., Haemophilus parainfluenzae (including strains resistant to ampicillin), Pasteurella multocida. Salmonella spp., Shigella spp. and Yersinia enterocolitica.
The drug Ceftazidime has the highest activity among third generation cephalosporins against Pseudomonas aeruginosa and nosocomial infections. The drug is active against gram-positive bacteria: Micrococcus spp., Streptococcus aureus, Streptococcus mitis, Streptococcus pneumoniae, Streptococcus pyogenes group A, Streptococcus viridans and other Streptococcus spp. (excluding Streptococcus faecalis); strains sensitive to methicillin: Staphylococcus aureus, Staphylococcus epidermidis.
The drug Ceftazidime is active against anaerobic bacteria: Bacteroides spp. (most strains of Bacteroides fragilis are resistant), Clostridium perfringens, Peptococcus spp., Peplostreptococcus spp. and Propionobacterium spp. The drug is not active against methicillin-resistant strains of Campilobacter spp., Chlamydia spp., Clostridium difficile, Enterococcus spp., Listeria monocytogenes and other Lisleria spp., Staphylococcus aureus and Staphylococcus epidermidis; Streptococcus faecalis.
Pharmacokinetics
After administration, the drug is rapidly distributed in the human body and reaches therapeutic concentrations in most tissues and fluids, including synovial, pericardial and peritoneal fluid, as well as in bile, sputum and urine. Distribution also occurs in the bones, myocardium, gall bladder, skin and soft tissues in concentrations sufficient to treat infectious diseases, especially in inflammatory processes that enhance the diffusion of the drug. It penetrates poorly through the intact blood-brain barrier, but the therapeutic level achieved by the drug in the cerebrospinal fluid is sufficient for the treatment of meningitis.
Reversibly binds to plasma proteins (less than 15%), and has a bactericidal effect only in its free form. The degree of protein binding does not depend on concentration. The maximum concentration with intramuscular administration of 0.5 g or 1 g after an hour is, respectively, 17 μg/ml and 39 μg/ml, with intravenous administration, respectively, 42 μg/ml and 69 μg/ml. The time to reach maximum concentration with intramuscular administration is 1 hour, with intravenous administration – by the end of the infusion. The concentration of the drug, equal to 4 mcg/ml, is maintained for 6-8 hours. Therapeutic concentration in blood plasma is maintained for 8-12 hours.
The half-life with normal renal function is 1.8 hours; if broken – 2.2 hours. The drug is not metabolized in the liver, liver dysfunction does not affect the pharmacodynamics and pharmacokinetics of the drug. The dose in such patients remains normal. Up to 80-90% is excreted unchanged by the kidneys (70% of the administered dose is excreted in the first 4 hours) during the day by glomerular filtration and tubular secretion to an equal extent.
If renal function is impaired, a dose reduction is recommended. The volume of distribution is 0.21-0.28 l/kg. The drug accumulates in soft tissues, kidneys, lungs, bones and joints, and serous cavities.
Special instructions
Special instructions
Patients with a history of allergic reactions to penicillins may have increased sensitivity to cephalosporin antibiotics.
During treatment, you should not drink ethanol.
When using the drug and 2-3 weeks after stopping treatment, diarrhea caused by Clostridium difficile may develop.
In mild cases, it is sufficient to discontinue treatment and use ion exchange resins (colestyramine, colestipol); in severe cases, replacement of loss of fluid, electrolytes and protein, and the appointment of vancomycin, bacitracin or metronidazole are indicated. You should not use medications that inhibit intestinal motility.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions due to the risk of dizziness.
Active ingredient
Active ingredient
Ceftazidime
Composition
Composition
1 bottle of powder for the preparation of solution for injection contains:
active ingredient:
1.0 g ceftazidime sodium carbonate pentahydrate (in terms of ceftazidime)
Pregnancy
Pregnancy
During pregnancy, the drug is used only if the expected benefit to the mother outweighs the potential risk to the fetus and child. When using the drug during lactation, breastfeeding should be discontinued.
Contraindications
Contraindications
hypersensitivity to the components of the drug Ceftazidime-AKOS;
hypersensitivity to cephalosporins and penicillins.
With caution: renal failure, history of colitis, malabsorption syndrome (increased risk of decreased prothrombin activity, especially in persons with severe renal and/or liver failure), simultaneous administration with a loop diuretic and an aminoglycoside, as well as in a newborn.
Side Effects
Side Effects
Allergic reactions: urticaria, chills or fever, rash, itching, bronchospasm, eosinophilia, Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell’s syndrome), angioedema, anaphylactic shock.
From the digestive system: nausea, vomiting, diarrhea, flatulence, abdominal pain, dysbacteriosis, increased activity of liver transaminases, alkaline phosphatase, hyperbilirubinemia, stomatitis, glossitis, pseudomembranous enterocolitis, oropharyngeal candidiasis, cholestasis.
From the hematopoietic system: eosinophilia, leukopenia, neutropenia, agranulocytosis, granulocytopenia, thrombocytopenia, hemolytic anemia, lymphocytosis, hemorrhages.
From the reproductive system: candidal vaginitis.
From the urinary system: impaired renal function, toxic nephropathy.
From the central nervous system: headache, dizziness, paresthesia, dizziness, seizures, encephalopathy, “fluttering tremor”.
Laboratory indicators: hypercreatininemia, increased urea concentration, false-positive urine reaction to glucose, false-positive direct Coombs reaction, increased prothrombin time.
Local reactions: with intravenous administration – phlebitis; with intramuscular injection – pain, burning, compaction at the injection site.
Other: nosebleeds, superinfection.
Interaction
Interaction
Pharmaceutically incompatible with aminoglycosides, heparin, vancomycin. Do not use sodium bicarbonate solution as a solvent. Loop diuretics, aminoglycosides, vancomycin, clindamycin reduce the clearance of ceftazidime, resulting in an increased risk of nephrotoxicity.
Pharmaceutically compatible with the following solutions: at concentrations from 1 to 40 mg/ml – sodium chloride 0.9%, sodium lactate, Hartmann’s solution, dextrose 5%, sodium chloride 0.225% and dextrose 5%, sodium chloride 0.45% and dextrose 5%, sodium chloride 0.9% and dextrose 5%, sodium chloride 0.18% and dextrose 4%, dextrose 10%, dextran 40:10% in sodium chloride solution 0.9%, dextran 40:10% in dextrose solution 5%, dextran 70:6% in sodium chloride solution 0.9%, dextran 70:6% in dextrose solution 5%. At concentrations of 0.05 to 0.25 mg/ml, ceftazidime is compatible with intraperitoneal dialysis solution (lactate).
For intramuscular administration, ceftazidime can be diluted with a solution of lidocaine hydrochloride 0.5% or 1%. Both components remain active when ceftazidime is added to the following solutions (ceftazidime concentration 4 mg/ml): hydrocortisone (hydrocortisone sodium phosphate) 1 mg/ml in sodium chloride 0.9% solution or dextrose solution 5%, cefuroxime (cefuroxime sodium) 3 mg/ml in sodium chloride 0.9% solution, cloxacillin (cloxacillin sodium) 4 mg/ml in 0.9% sodium chloride solution, heparin 10 IU/ml or 50 IU/ml in 0.9% sodium chloride solution, potassium chloride 10 mEq/l or 40 mEq/l in 0.9% sodium chloride solution. When mixing a solution of ceftazidime (500 mg in 1.5 ml of water for injection) and metronidazole (500 mg/100 ml), both components retain their activity.
Overdose
Overdose
Symptoms: pain, inflammation, phlebitis at the injection site, dizziness, paresthesia, headache, convulsions in patients with renal failure, hypercreatininemia, hyperbilirubinemia, thrombocytosis, thrombocytopenia, eosinophilia, leukopenia, prolongation of prothrombin time.
Treatment: symptomatic therapy is carried out, in case of renal failure – peritoneal dialysis or hemodialysis.
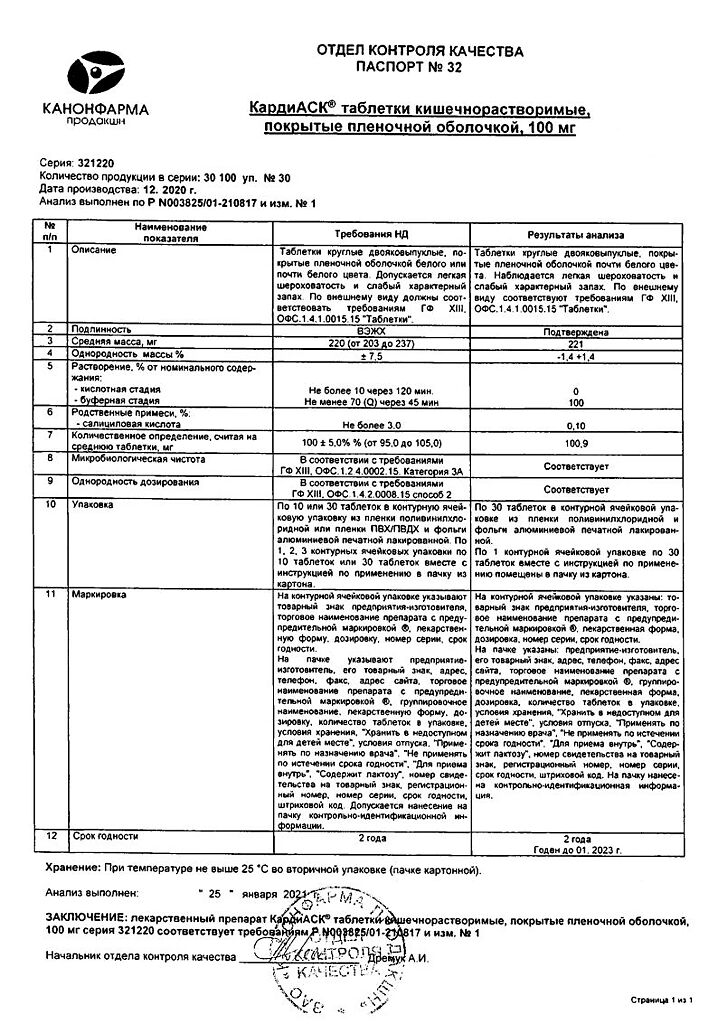
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature below 25 °C
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
Sintez, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature below 25 °C |
| Manufacturer | Sintez OAO, Russia |
| Medication form | Powder for preparation of solution |
| Brand | Sintez OAO |
Related products
Buy Ceftazidime-Akos, 1 g with delivery to USA, UK, Europe and over 120 other countries.