No products in the cart.
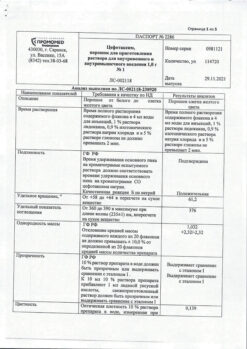
Cefotaxime, 1 g
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: Antibiotic-cephalosporin
ATX code: J01DD01
Pharmacokinetics
Absorption and distribution
In adults 5 min after a single intravenous (IV) injection of 1 g of cefotaxime the maximum concentration (Cmax) in blood plasma is 100 µg/ml. After intramuscular (i/m) injection of cefotaxime at the same dose Cmax in plasma is reached after 0.5 h and is 20 to 30 mcg/ml. Bioavailability of cefotaxime when administered intravenously is 100%, when administered intravenously – 90-95%.
Binding to plasma proteins (mainly albumin) is on average 25-40%.
Metabolism
Metabolized in the liver with the formation of the active metabolite desacetylcephotaxime (Ml), which has antibacterial activity, and inactive metabolites (M2, M3).
About 90% of the administered dose is excreted by the kidneys: 50% – unchanged, about 15-25% as the metabolite deacetylcephotaxime and 15-30% as inactive metabolites (M2-M3). 10% of the administered dose is excreted by the intestine. The half-life (T1/2) of cefotaxime is 1 h when administered by IV and 1-1.5 h when administered by IV/m.
In elderly patients over 80 years old the T1/2 of cefotaxime is increased to 2.5 h. The volume of distribution (Vd) does not change compared to young healthy volunteers.
In adults with impaired renal function, Vd is unchanged and T1/2 does not exceed 2.5 h, even in the last stages of renal failure.
In children the plasma concentration of cefotaxime and Vd are similar to those in adults receiving the same dose of the drug in mg kg weight. T1/2 of cefotaxime is 0.75 to 1.5 h.
In newborns and prematurely born children the plasma concentration of cefotaxime and Vd are similar to those in children. The average T1/2 of cefotaxime is 1.4 to 6.4 h.
Pharmacodynamics
A semi-synthetic antibiotic of the group of III generation cephalosporins. Cefotaxime acts bactericidally by disrupting the synthesis of the bacterial wall. It is also resistant to the action of most β-lactamases.
The following bacteria are usually sensitive to cefotaxime: Aeromonas hydrophila; Bacillus subtilis; Bordetella pertussis; Borrelia burgdorferi; Moraxella (Branhamella) catarrhalis; Citrobacter diversus*; Citrobacter freundii*; Clostridium perfringens; Corynebacterium diphtheriae; Escherichia coli; Enterobacter spp.*; Erysipelothrix insidiosa; Eubacterium spp.; Haemophilus spp. (penicillinase-producing and non-producing strains, including ampicillin-resistant strains); Klebsiella pneumoniae; Klebsiella oxytoca; Staphylococcus spp. (methicillin-sensitive, including penicillinase-producing and nonproducing strains); Morganella morgcinii; Neisseria gonorrhoeae (including penicillinase-producing and nonproducing strains); Neisseria meningitidis; Propionibacterium spp.Proteus mirabilis; Proteus vulgaris; Providencia spp.; Streptococcus spp. (including Streptococcus pneumoniae); Salmonella spp.; Serratia spp*; Shigella spp; Veillonella spp.*;Yersinia spp.*; Pseudomonas spp. (except Pseudomonas aeruginosa, Pseudomonas cepacia).
*Sensitivity depends on epidemiological data and on the level of resistance in each specific country.
The following are resistant to cefotaxime: Acinetobacter baumanii; Bacteroides fragilis; Clostridium difficile; Enterococcus spp.; Gram-negative anaerobes; Listeria monocytogenes; Staphylococcus spp. (methicillin-resistant strains); Pseudomonas aeruginosa, Pseudomonas cepacia; Stenotrophomonas maltophilia.
Indications
Indications
Cefotaxime is intended for the treatment of infections caused by microorganisms sensitive to the drug:
– respiratory tract infections;
– urinary tract infections;
– septicemia bacteremia;
– endocarditis;
– intra-abdominal infections (including peritonitis);
– meningitis (except listeria) and other infections of the central nervous system;
– infections of the skin and soft tissues;
– infections of bones and joints.
Prevention of infections after surgical operations on the gastrointestinal tract, urological and obstetric-gynecological operations.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Antibiotic-cephalosporin
ATX code: J01DD01
Pharmacokinetics
Suction and distribution
In adults, 5 minutes after a single intravenous (IV) administration of 1 g of cefotaxime, the maximum concentration (Cmax) in blood plasma is 100 mcg/ml. After intramuscular (IM) administration of cefotaxime at the same dose, Cmax in blood plasma is reached after 0.5 hours and ranges from 20 to 30 mcg/ml. The bioavailability of cefotaxime with intravenous administration is 100%, with intramuscular administration it is 90–95%.
Binding to plasma proteins (mainly albumin) averages 25–40%.
Metabolism
Metabolized in the liver to form the active metabolite desacegilcefotaxime (Ml), which has antibacterial activity, and inactive metabolites (M2, M3).
Removal
About 90% of the administered dose is excreted by the kidneys: 50% unchanged, about 15–25% as a metabolite of desacetylcefotaxime and 15–30% as inactive metabolites (M2-MZ). 10% of the administered dose is excreted by the intestines. The half-life (T1/2) of cefotaxime is 1 hour with intravenous administration and 1–1.5 hours with intramuscular administration.
In elderly patients over 80 years of age, T1/2 of cefotaxime increases to 2.5 hours. The volume of distribution (Vd) does not change compared to young healthy volunteers.
In adults with impaired renal function, Vd does not change, and T1/2 does not exceed 2.5 hours, even in the last stages of renal failure.
In children, the plasma concentrations of cefotaxime and Vd are similar to those in adults receiving the same dose of the drug in mg kg body weight. T1/2 of cefotaxime ranges from 0.75 to 1.5 hours.
In newborns and prematurely born children, the plasma concentrations of cefotaxime and Vd are similar to those in children. The average half-life of cefotaxime ranges from 1.4 to 6.4 hours.
Pharmacodynamics
Semisynthetic antibiotic of the third generation cephalosporin group. Cefotaxime acts bactericidal by disrupting the synthesis of the bacterial wall. It is also resistant to most β-lactamases.
The following are usually sensitive to cefotaxime: Aeromonas hydrophila; Bacillus subtilis; Bordetella pertussis; Borrelia burgdorferi; Moraxella (Branhamella) catarrhalis; Citrobacter diversus*; Citrobacter freundii*; Clostridium perfringens; Corynebacterium diphtheriae; Escherichia coli; Enterobacter spp.*; Erysipelothrix insidiosa; Eubacterium spp.; Haemophilus spp. (penicillinase-producing and non-penicillinase-producing strains, including ampicillin-resistant); Klebsiella pneumoniae; Klebsiella oxytoca; Staphylococcus spp. (methicillin-sensitive, including penicillinase-producing and non-penicillinase-producing strains); Morganella morgcinii; Neisseria gonorrhoeae (including penicillinase-producing and non-penicillinase-producing strains); Neisseria meningitidis; Propionibacterium spp.; Proteus mirabilis; Proteus vulgaris; Providencia spp.; Streptococcus spp. (including Streptococcus pneumoniae); Salmonella spp.; Serratia spp*; Shigella spp; Veillonella spp.*;Yersinia spp.*; Pseudomonas spp. (except Pseudomonas aeruginosa, Pseudomonas cepacia).
* – sensitivity depends on epidemiological data and the level of resistance in each specific country.
Resistant to cefotaxime: Acinetobacter baumanii; Bacteroides fragilis; Clostridium difficile; Enterococcus spp.; gram-negative anaerobes; Listeria monocytogenes; Staphylococcus spp. (methicillin-resistant strains); Pseudomonas aeruginosa, Pseudomonas cepacia; Stenotrophomonas maltophilia.
Special instructions
Special instructions
Anaphylactic reactions
The prescription of cephalosporins requires the collection of an allergic history (allergic diathesis of hypersensitivity reaction to beta-lactam antibiotics).
If the patient develops a hypersensitivity reaction, treatment should be discontinued.
The use of cefotaxime is contraindicated in patients with a history of immediate hypersensitivity reaction to cephalosporins. If there is any doubt, the presence of a doctor during the first administration of the drug is mandatory due to a possible anaphylactic reaction.
There is a known cross-allergy between cephalosporins and penicillins, which occurs in 5-10% of cases. Anaphylactic reactions that develop in this situation can be serious or even fatal.
In patients with a history of allergy to penicillins, the drug should be used with extreme caution. The patient’s condition should be carefully monitored when the drug is first administered due to a possible anaphylactic reaction.
If the first symptoms and signs of anaphylactic shock develop, you should immediately stop administering the drug. The patient should remain in the supine position with legs elevated. Slow intravenous administration of 01 mg (1 ml) of epinephrine (adrenaline) solution under control of pulse and blood pressure is indicated, as well as intravenous administration of human albumin plasma substitutes or balanced electrolyte solutions; subsequently – intravenous administration of glucocorticosteroids (for example, 250-1000 mg of hydrocortisone) once or, if necessary, repeatedly.
Supportive therapeutic measures should be carried out: artificial ventilation, oxygen inhalation, administration of antihistamines.
Diseases caused by Clostridium difficile (eg pseudomembranous colitis)
Diarrhea that is particularly severe and/or prolonged during treatment or in the first weeks after the end of treatment with various particularly broad-spectrum antibiotics may be a symptom of a disease caused by Clostridium difficile, the most severe form of which is pseudomembranous colitis. The diagnosis of this rare but possibly fatal disease is confirmed endoscopically and/or histologically. The most important method for confirming the diagnosis of pseudomembranous colitis is the identification of Clostridium difficile toxins in the stool. If a diagnosis of pseudomembranous colitis is suspected, cefotaxime should be stopped immediately and appropriate specific antibiotic therapy (for example, oral vancomycin or metronidazole) should be started immediately. Drugs that inhibit intestinal motility are contraindicated.
Encephalopathy
When using beta-lactam antibiotics, including cefotaxime, there is an increased risk of developing encephalopathy (which may include seizures, confusion, impaired consciousness, and movement disorders), especially in cases of overdose or renal failure.
Use of lidocaine as a solvent
When using lidocaine as a solvent, it is necessary to take into account the information presented in the “Contraindications” section.
Injection rate
The rate of administration of the drug should be monitored (See section “Method of administration and dosage”).
Kidney failure
In case of renal failure, the dose should be adjusted depending on creatinine clearance (See section “Dosage and Administration”).
Caution should be exercised when using cefotaxime and aminoglycosides simultaneously. Renal function should be monitored in all cases of combined use of cefotaxime with aminoglycosides and other nephrotoxic drugs in elderly patients or with renal impairment.
Sodium content
In patients requiring sodium restriction, the sodium content of cefotaxime sodium salt (482 mg/g) should be taken into account.
Hematopoietic disorders
During treatment with cefotaxime, leukopenia, neutropenia, and, more rarely, bone marrow hematopoietic failure, pancytopenia and agranulocytosis, may develop.
If the course of treatment lasts more than 10 days, the number of blood cells should be monitored. If these blood parameters deviate from the norm, the drug should be discontinued.
Laboratory tests
During therapy with cephalosporins, a positive Coombs test may occur. It is recommended to use glucose oxidase methods for determining the concentration of glucose in the blood due to the development of false positive results when using nonspecific reagents.
Impact on the ability to drive vehicles. Wed and fur.:
In the event of the development of such adverse reactions as dizziness and encephalopathy (which can manifest itself as convulsions, confusion, disturbances of consciousness, and movement disorders), patients should refrain from driving vehicles and operating machinery.
Active ingredient
Active ingredient
Cefotaxime
Composition
Composition
1 bottle contains:
Active ingredient
Cefotaxime sodium (in terms of cefotaxime) – 1 g.
Pregnancy
Pregnancy
Pregnancy
Cefotaxime penetrates the placental barrier. Studies conducted on animals did not reveal any teratogenic or fetotoxic effects of the drug. However, the safety of cefotaxime during pregnancy in humans has not been established; therefore, the drug should not be used during pregnancy.
Breastfeeding period
Cefotaxime passes into breast milk; therefore, if it is necessary to prescribe the drug, breastfeeding should be interrupted.
Contraindications
Contraindications
– Hypersensitivity to cefotaxime and other cephalosporins.
– For forms containing lidocaine as a solvent:
– hypersensitivity to lidocaine or other amide-type local anesthetic;
– intracardiac blockade without an established pacemaker;
– severe heart failure;
– intravenous administration;
– children under 25 years of age (intramuscular administration).
With caution:
In patients with a history of allergies to penicillins (risk of developing cross-allergic reactions);
when used simultaneously with aminoglycosides;
with renal failure.
Side Effects
Side Effects
Classification of undesirable side reactions by frequency of development according to the recommendations of the World Health Organization: very often (≥10%); often (≥1% and <10%); uncommon (≥01% and <1%); rare (≥001% and <01%); very rare (<001%); frequency is unknown (based on the available data, it is impossible to estimate the frequency of side effects).
Infectious and parasitic diseases: frequency unknown: superinfections. As with the prescription of other antibiotics, especially long-term use of cefotaxime can lead to excessive growth of insensitive microorganisms. The patient’s condition should be monitored regularly. If the development of superinfection occurs during cefotaxime therapy, appropriate measures should be taken.
Blood and lymphatic system disorders: uncommon: leukopenia, eosinophilia, thrombocytopenia. Frequency unknown: bone marrow hematopoiesis deficiency pancytopenia neutropenia agranulocytosis hemolytic anemia.
Immune system disorders: uncommon: Jarisch-Herxheimer reaction. As with the use of other antibiotics in the treatment of borreliosis, the development of a Jarisch-Herxheimer reaction is possible during the first days of therapy. There are reports of the occurrence of one or more symptoms after a few weeks of treatment for borreliosis: skin rash itching fever leukopenia increased activity of liver enzymes difficulty breathing discomfort in the joints. It should be borne in mind that to some extent these manifestations are consistent with the symptoms of the underlying disease for which the patient is receiving treatment. Frequency unknown: anaphylactic reactions, angioedema, bronchospasm, anaphylactic shock.
Nervous system disorders: uncommon: seizures. Frequency unknown: encephalopathy (for example, impaired consciousness, impaired motor activity), headache, dizziness.
Cardiac disorders: frequency unknown: arrhythmias (due to rapid bolus administration through a central venous catheter).
Gastrointestinal disorders: uncommon: diarrhea. Frequency unknown: nausea, vomiting, abdominal pain, pseudomembranous colitis.
Disorders of the liver and biliary tract: uncommon: increased activity of liver enzymes (alanine aminotransferase (ALT), aspartate aminotransferase (ACT), lactate dehydrogenase (LDH), gamma-glutamyltransferase (gamma-GT), alkaline phosphatase (ALP)) and/or bilirubin concentration. These laboratory abnormalities (which can also be explained by the presence of infection) in rare cases exceed the upper limit of normal by 2 times and indicate liver damage manifested by cholestasis and often asymptomatic. Frequency unknown: hepatitis (sometimes with jaundice).
Skin and subcutaneous tissue disorders: uncommon: rash, itching, urticaria. Frequency unknown: erythema multiforme Stevens-Johnson syndrome toxic epidermal necrolysis acute generalized exanthematous pustulosis.
Renal and urinary tract disorders: uncommon: decreased renal function/increased creatinine concentration, especially when used in combination with aminoglycosides. Frequency unknown: acute renal failure, interstitial nephritis.
General disorders and disorders at the injection site: often: pain at the injection site (with intramuscular administration). Uncommon: fever, inflammatory reactions at the injection site including phlebitis/thromphlebitis. Frequency unknown: with intramuscular administration, if lidocaine is used as a solvent, systemic reactions associated with lidocaine may develop, especially in cases of unintentional intravenous injection of the drug into highly vascularized tissues or in case of overdose.
Interaction
Interaction
Probenecid delays excretion and increases plasma concentrations of cephalosporins.
As with the use of other cephalosporins, cefotaxime may enhance the nephrotoxic effect of drugs with nephrotoxic effects (such as furosemide aminoglycosides).
Compatibility instructions: cefotaxime should not be mixed with other antibiotics (including aminoglycosides) either in the same syringe or in the same infusion solution.
The following solutions can be used for infusions (cefotaxime concentration 1 g / 250 ml): water for injection 09% sodium chloride solution 5% dextrose solution Ringer’s solution Yonosteril lactate.
Overdose
Overdose
There is a risk of developing reversible encephalopathy when using beta-lactam antibiotics including cefotaxime, especially in case of overdose or impaired renal function. There is no specific antidote. Cefotaxime can be removed by hemodialysis and is not removed by peritoneal dialysis.
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25°C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Belmedpreparaty, Belarus
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25°C. Store out of the reach of children. |
| Manufacturer | Belmedpreparaty, Belarus |
| Medication form | Powder for preparation of solution |
| Brand | Belmedpreparaty |
Other forms…
Related products
Buy Cefotaxime, 1 g with delivery to USA, UK, Europe and over 120 other countries.