No products in the cart.
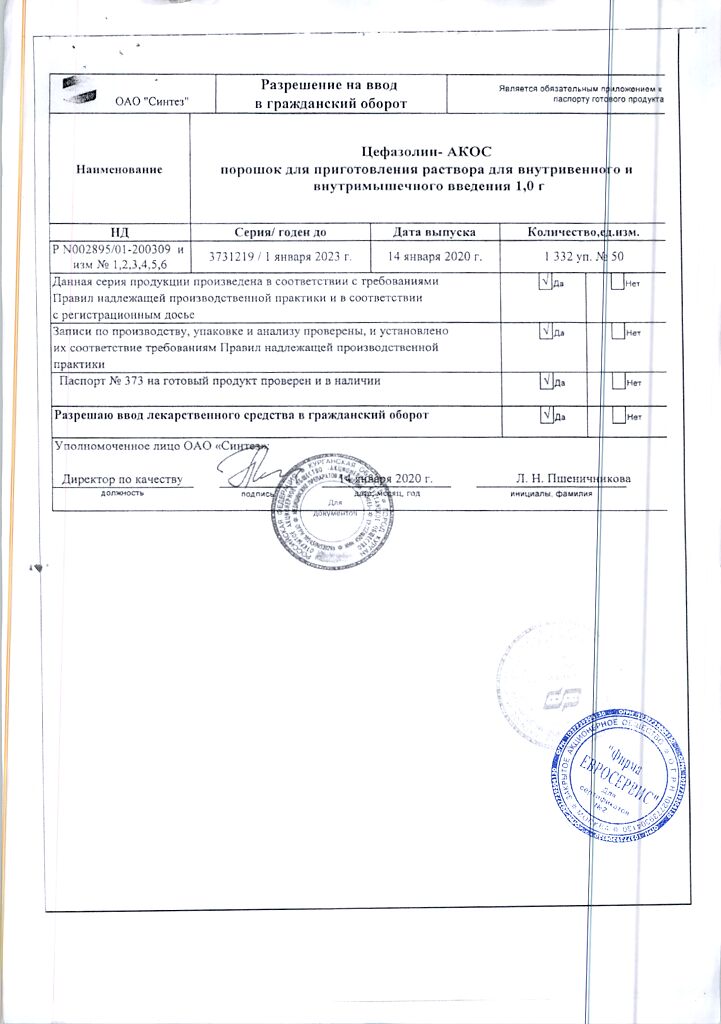
Cefazolin-ACOS, 1 g 50 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group
Cephalosporin antibiotic
ATX code: J01DB04
Pharmacodynamics:
A first generation cephalosporin antibiotic for parenteral use. It acts bactericidally by disrupting synthesis of the cell wall of microorganisms. It has a wide spectrum of action active against Gram-positive (Staphylococcus spp. Staphylococcus aureus (not producing and producing penicillinase) Streptococcus pneumoniae Corynebacterium diphtheriae Bacillus anthracis) and gram-negative (Neisseria meningitidis Neisseria gonorrhoeae Shigella spp. Salmonella spp. Escherichia coli Klebsiella spp. Treponema spp. Leptospira spp.) microorganisms. Active against Haemophilus influenzae some strains of Enterobacter spp. and Enterococcus spp.
Ineffective against Pseudomonas aeruginosa indole-positive strains of Proteus spp. Mycobacterium tuberculosis Serratia spp. anaerobic microorganisms methicillin-resistant strains of Staphylococcus spp.
Pharmacokinetics:
Time to maximum concentration (TCmax) with intramuscular injection at a dose of 0.5 and 1 g respectively – 2 and 1 h; maximum concentration (Cmax) – 38 and 64 mcg/ml; after intravenous administration, TCshah – at the end of infusion after intravenous administration of 1 g Cmax – 180 mcg/ml. It penetrates into the joints heart and vascular tissues in the abdomen kidneys and urinary tract placenta middle ear respiratory tract skin and soft tissues. Small amounts are excreted with breast milk.
Concentration in gallbladder tissue and bile is significantly higher than in blood serum. With gallbladder obstruction the concentration in bile is lower than in plasma. The volume of distribution is 0.12 l/kg. Binding with plasma proteins is 85%. Half-life (T1/2) when administered intramuscularly is 1.8 hours, when administered intravenously is 2 hours. In patients with impaired renal function the T1/2 period is 20-40 hours. It is eliminated mainly by kidneys in unchanged form: during the first 6 hours – 60-90% after 24 hours – 70-95%. After intramuscular administration in doses of 0.5 and 1 g, Cmax in urine is 1 mg/ml and 4 mg/ml, respectively.
Indications
Indications
Bacterial infections caused by cefazolin-sensitive microorganisms:
– Respiratory tract infections;
– Urinary and genital tract infections;
– infections of the biliary tract;
– infections of the skin, soft tissues, bones and joints, including osteomyelitis;
– bacterial endocarditis, sepsis;
– intraoperative prophylaxis of the development of infections (prophylactic administration of cefazolin may reduce the likelihood of infection in the postoperative period).
The in vitro sensitivity of antibiotics varies by geographic region and over time, so local resistance information should be considered when choosing antibiotic therapy. If possible, antimicrobial sensitivity testing of the pathogen should be performed. Therapy may be initiated empirically, prior to antibiotic sensitivity test results.
Active ingredient
Active ingredient
Composition
Composition
Per 1 vial
Active substance:
Cefazolin sodium – 0.524 g, 1.048 g (in terms of cefazolin – 0.5 g, 1 g).
How to take, the dosage
How to take, the dosage
Cefazolin is intended for parenteral administration only – the drug should be administered intravenously (IV) (by trickle or drip) or deeply intramuscularly (intramuscular).
The doses of the drug and the duration of treatment are determined individually, taking into account the severity of the course and localization of the infection, as well as the potential sensitivity of the pathogen.
Average daily dose for adults is 1-4 g; number of times of administration is 3-4 times a day. Maximal daily dose is 6 g. Average duration of treatment is 7-10 days.
In accordance with the principles of antibiotic therapy, the course of treatment should be continued for at least 2-3 days after resolution of fever or until confirmation of eradication of the pathogen.
Prevention of intraoperative infections
The initial dose of cefazolin, 1 g, should be given 30 min-1 h before surgery by IV or IM. In case of prolonged operations (2 hours and longer) 0.5 g-1 g of the drug should be administered directly during the operation. Doses and times of administration depend on the type and duration of surgery. Within 24 hours after surgery we administer 0.5 g – 1 g of the drug by IV or IM with an interval of 6-8 hours.
If the possibility of infection poses a great danger to the patient (e.g., after cardiac surgery or major orthopedic surgery such as total joint replacement), it is recommended that the drug be continued for 3-5 days. It is important to adhere to the above timescales so that sufficient concentrations of the antibiotic are already present in the serum and tissues at the time of the surgical incision. If there is an increased risk of anaerobic infection (e.g., after colorectal surgery), additional use of a drug active against anaerobes is recommended.
Elderly patients
Dose adjustment is not required.
Use in children from 1 month to 18 years
For the treatment of most infections of mild to moderate severity, a daily dose of 25-50 mg/kg divided into 3-4 injections is sufficient.
In case of severe infections the daily dose can be increased to the maximum recommended dose of 100 mg/kg. The safety of using the drug in infants has not been established.
Interaction
Interaction
Cefazolin may decrease the effectiveness of oral contraceptives. For this reason, additional contraceptive measures should be used during treatment with the drug.
Cefazolin should not be used together with other antibacterial drugs with bacteriostatic action (e.g., tetracyclines, sulfonamides, erythromycin, chloramphenicol), because in in vitro studies antagonism between these drugs has been revealed.
In co-administration with cefazolin nephrotoxic properties of other antibacterial agents (e.g., aminoglycosides, colistin, polymyxin B); iodine-containing contrast agents may be increased; high doses of methotrexate; some antiviral drugs (e.g., acyclovir, foscarnet); pentamidine; cyclosporine; tacrolimus; platinum-containing drugs and diuretics (e.g., furosemide). If it is necessary to combine them with cefazolin, renal function should be carefully monitored.
Concomitant use with “loop” diuretics (e.g., furosemide) leads to blockade of tubular secretion of cefazolin, which leads to increased plasma concentrations. For this reason, co-administration of these drugs should be avoided.
When co-administration of cefazolin and probenecid the renal clearance of cefazolin is decreased, which leads to increased elimination time of cefazolin and increased plasma concentrations.
In rare cases cephalosporins can cause coagulation disorders. If coadministration with oral anticoagulants is necessary, especially in high doses, coagulogram parameters should be monitored.
Some cephalosporin antibiotics, such as cefamandole, cefotetan and cefazolin, by inhibiting intestinal microflora can disrupt metabolism of vitamin K, which reduces its formation in the body, especially in patients with baseline deficiency. It may be necessary to prescribe vitamin K preparations.
Concomitant use with drugs that reduce platelet aggregation (e.g., non-steroidal anti-inflammatory drugs) increases the risk of bleeding.
Cefazolin may cause disulfiram-like reactions when used concomitantly with ethanol.
Cefazolin is pharmaceutically incompatible with antibiotics of the group of aminoglycosides (gentamicin, kanamycin, amikacin, etc.); tetracyclines (oxytetracycline, tetracycline, etc.); colistimethago sodium; polymyxin B; erythromycin (in the form of glucoheptonate salt); barbiturate derivatives (amobarbital, pentobarbital); bleomycin; calcium salts (calcium glucoheptonate, calcium gluconate); cimetidine; ascorbic acid.
Special Instructions
Special Instructions
Hypersensitivity reactions
An allergologic history should be taken before starting cefazolin administration due to the possibility of cross-sensitivity between cephalosporins and other betalactam antibiotics. Severe, including fatal, allergic reactions have been described during cephazolin therapy. In case of severe hypersensitivity reactions it is necessary to cancel cefazolin, prescribe appropriate symptomatic therapy. The drug is contraindicated in patients with severe hypersensitivity reactions to cephalosporins or any other beta-lactam antibiotics in history.
Patients with a predisposition to allergic reactions (allergic rhinitis, bronchial asthma) should be monitored particularly closely, since the risk of hypersensitivity reactions increases with these conditions.
Diarrhea associated with antibiotic use
The development of severe and persistent diarrhea during treatment and in the first weeks after therapy may be a manifestation of pseudomembranous colitis caused by Clostridium difficile. Since this condition is life-threatening, cefazolin should be withdrawn immediately and specific antibacterial therapy (e.g., vancomycin or metronidazole) should be prescribed. Symptomatic supportive therapy is indicated, including correction of water-electrolyte balance, nutritional disorders. The use of drugs inhibiting intestinal peristalsis is contraindicated. In particularly severe cases, if the infection is resistant to the ongoing antibiotic therapy, colectomy may be required. Careful attention should be paid to the patient’s medical history, since there have been cases of pseudomembranous colitis within two months of antibiotic therapy.
Renal dysfunction
With regard to the cumulation of the drug in the body, in patients with reduced renal function the dose of the drug should be adjusted to the severity of renal failure (see also section “Dosage and administration”). Although the use of cefazolin rarely causes renal dysfunction and development of renal failure, it is recommended to assess renal function during the use of the drug, especially in patients in severe condition, when using high doses of the drug and/or other nephrotoxic drugs (e.g., aminoglycosides, “loop” diuretics).
The development of bacterial resistance and superinfections
Long-term use of cefazolin may provoke the emergence of resistant strains of bacteria. Patients should be closely monitored for the possibility of superinfection and appropriate measures should be taken if this occurs.
Decreased blood clotting and bleeding
In rare cases during the use of cefazolin decreased blood clotting is possible. Risk factors include vitamin K deficiency, parenteral nutrition, renal and/or hepatic insufficiency, thrombocytopenia, anticoagulant therapy. In addition, diseases such as hemophilia, gastric and/or duodenal mucosal ulceration may cause the development or increase the severity of bleeding. Therefore, it is necessary to monitor coagulogram values in patients with the known presence of these diseases. If a decrease in blood clotting is detected, therapy with vitamin K (10 mg/week) should be prescribed.
Preventive therapy in children
Cefazolin should not be used in premature and newborn children within 1 month of life since to date there are no data to confirm its safety in this patient population.
The sodium content
1 g of cefazolin contains approximately 48 mg of sodium, which must be considered when using the drug in patients on a sodium-restricted diet.
Impact on laboratory parameters
False-positive urine glucose concentrations with Benedict or Fehling reagent may occur with cefazolin use, as well as false-positive results of direct and indirect Coombs test.
Peripheral blood counts should be monitored with long-term use of the drug.
Taking ethanol during treatment
Because of the possibility of disulfiram-like reactions with cefazolin, patients should refrain from alcohol during treatment.
Intrathecal administration
Cefazolin should not be administered intrathecally due to the possibility of severe toxic effects on the central nervous system (including seizures).
Influence on the ability to drive vehicles, mechanisms
The effect of cefazolin on the ability to drive vehicles and operate mechanisms has not been revealed. Nevertheless, since with the use of cefazolin such side effects as nausea, vomiting, dizziness and seizures may occur, caution should be exercised while performing these activities and abstain from them in case of development of such adverse events.
Contraindications
Contraindications
– hypersensitivity to cephazolin;
– history of severe hypersensitivity reactions (e.g., anaphylactoid reactions) to cephalosporins or any other beta-lactam antibiotics (penicillins, monobactams, carbapenems);
– period of newborn infancy up to 1 month, including premature infants.
When using lidocaine solution as a solvent – see the lidocaine instructions for use.
With caution
– co-administration of other nephrotoxic drugs;
– history of non-serious hypersensitivity reactions to penicillins;
– chronic renal insufficiency;
– bowel disease (including history of colitis).
– bowel disease (including a history of colitis);
– childhood age from 1 to 12 months.
Side effects
Side effects
According to the World Health Organization (WHO) classification, adverse reactions are presented according to their frequency of occurrence: Very common (>1/10), common (>1/100, < 1/10), infrequent (>1/1000, < 1/100), rare (>1/10000, < 1/1000) and very rare (< 1/10000), frequency unknown – the incidence could not be determined from available data.
Infections and parasitic infestations:
Infrequent – oral candidiasis (with long-term use); rarely – genital candidiasis, vaginitis.
Disorders of the blood and lymphatic system:
Rarely, leukopenia, granulocytopenia, neutropenia, thrombocytopenia. leukocytosis, granulocytosis, monocytosis, lymphocytosis. thrombocytosis, lymphocytopenia. basophilia, eosinophilia. As a rule, these adverse events are transient and reversible; very rarely – disorders of blood clotting and, as a consequence, increased bleeding, anemia, agranulocytosis, aplastic anemia, pancytopenia, hemolytic anemia.
Disorders of the immune system:
Infrequent – fever, arthralgia; very rare – anaphylactic shock (development of laryngeal edema with narrowing of the airway lumen, increased heart rate, dyspnea, decreased blood pressure, tongue swelling, facial edema, anal and/or genital itching).
Metabolic and nutritional disorders:
Rarely, hyperglycemia or hypoglycemia.
Nervous system disorders:
Infrequent – development of seizures (in patients with impaired renal function when the drug is used in high doses if the dosing regimen is not followed); rare – dizziness, malaise, general weakness, nightmares, vertigo, hyperactivity, nervousness or anxiety, insomnia or drowsiness, color vision disturbance, confusion, increased seizure activity of the brain.
Vascular disorders:
Rarely – “hot flashes”.
Respiratory system, chest and mediastinum disorders:
Rarely – pleural effusion, chest pain, bronchospasm, shortness of breath, cough, development of acute respiratory distress syndrome, rhinitis.
Gastrointestinal disorders:
Often – loss of appetite, diarrhea, nausea, vomiting, abdominal pain; very rarely – development of pseudomembranous colitis. This condition requires immediate start of treatment (see also section “Special indications”).
Liver and biliary tract disorders:
Rarely – transient increase of “liver” transaminases activity: alanine aminotransferase (ALT), aspartate aminotransferase (ACT), alkaline phosphatase, gamma-glutamyltransferase, lactate dehydrogenase, increased concentration of bilirubin in blood plasma, transient hepatitis, cholestatic jaundice.
Dermal and subcutaneous tissue disorders:
Often – rash; infrequently – erythema, exudative (polymorphic) erythema, urticaria, pruritus, angioedema (Quincke’s edema); rarely – toxic epidermal necrolysis (Lyell syndrome), malignant exudative erythema (Stevens-Johnson syndrome).
Rarely – interstitial nephritis, proteinuria, transient increase of urea concentration in plasma (usually in patients treated in combination with other nephrotoxic agents), nephropathy unspecified and other manifestations of nephrotoxicity.
Impact on the results of laboratory and instrumental studies:
Frequency unknown – false positive Coombs reaction, hypercreatininemia, increased prothrombin time, false positive urine glucose reaction.
General disorders and reactions at the site of administration:
Often, pain at the injection site after IUI, sometimes with development of thickening; infrequent, thrombophlebitis and phlebitis (when IUI).
Overdose
Overdose
Symptoms
Headache, vertigo, paresthesia, agitation, myoclonias, seizures.
Laboratory signs: increased plasma creatinine and urea concentrations, increased “hepatic” transaminase activity and bilirubin concentrations, positive Coombs reaction, thrombocytopenia or thrombocytosis, eosinophilia, leukopenia and increased prothrombin time.
Treatment
In case of seizures cefazolin should be withdrawn immediately, vital signs should be carefully monitored, symptomatic therapy should be administered if necessary, anticonvulsants may need to be prescribed if seizures develop. In case of severe overdose and ineffectiveness of other methods of treatment hemodialysis may be performed. Peritoneal dialysis is not effective.
Pregnancy use
Pregnancy use
Pregnancy
Cefazolin penetrates through the placenta. Preclinical studies of cefazolin in animals have shown no direct or indirect reproductive toxicity. However, because there is insufficient data on the safety of cefazolin, the use of cefazolin in pregnancy is acceptable only if the expected benefit to the mother exceeds the potential risk to the fetus.
Breastfeeding
Cefazolin penetrates into breast milk in very small amounts; when cefazolin is used in therapeutic doses, the effect on the newborn is unlikely. If a breastfed infant develops diarrhea or candidiasis symptoms, the decision should be made whether to stop breastfeeding or to discontinue the drug.
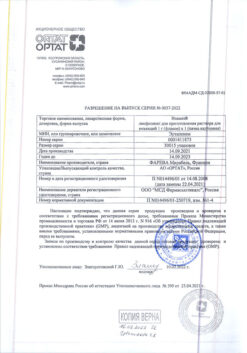
Similarities
Similarities
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25 °С. Store out of the reach of children. |
| Manufacturer | Sintez OAO, Russia |
| Medication form | Powder for preparation of solution |
| Brand | Sintez OAO |
Related products
Buy Cefazolin-ACOS, 1 g 50 pcs with delivery to USA, UK, Europe and over 120 other countries.