Subtotal: €2.18
Pharmacotherapeutic group: cephalosporin antibiotic.
To be sure to use the following medicines.
Pharmacological properties
Pharmacodynamics
Cephalosporin semisynthetic antibiotic of the first generation for parenteral use. It acts bactericidally by blocking the penicillin-binding proteins (e.g., transpeptidases), disrupts the synthesis of the cell wall of microorganisms. It has a wide spectrum of action. The prevalence of acquired resistance may vary geographically and also change over time, local information must be considered, especially in the treatment of severe infections.
Microorganisms sensitive to cefazolin.
Gram-positive aerobes: Staphylococcus aureus (sensitive to methicillin), Staphylococcus saprophyticus, Streptococcus pneumoniae, Streptococcus agalactiae, Streptococcus pyogenes, Corynebacterium diphtheria, Bacillus anthracis.
Gram-negative microorganisms: Veisseria meningitides, Neisserria gonorrhoeae, Shigella spp., Salmonella spp., Treponema spp., Leptospira spp.
Microorganisms that are moderately sensitive to cefazolin.
Gram-positive aerobes: Staphylococcus aus, Staphylococcus epidermidis, Staphylococcus haemolyticus*, Staphylococcus hominis*, Streptococcus pneumonia* (moderately sensitive to penicillins).
Gram-negative aerobes: Escherichia coli, Haemophilus influenza**, Klebsiella oxytoca***, Klebsiella pneumoniae, Proteus mirabilis.
Microorganisms with natural resistance to cefazolin.
Gram-positive aerobes: Enterococcus spp. , Staphylococcus aureus (resistant to methicillin), Staphylococcus pneumoniae (resistant to penicillin).
Gram-negative aerobes: Acinetobacter baumanii, Citrobacter freundii, Enterobacter spp., Morganella morganii, Moraxella catarrhalis, Proteus vulgaris, Pseudomonas aeruginosa, Serratia marcescens, Stenotrophomonas maltophilia.
Anaerobes: Bacteroides fragilis.
Other microorganisms: Chlamydia spp., Chlamydophila spp., Legionella spp., Mycoplasma spp.
Penicillin-resistant Streptococcus pneumoniae due to cross-resistance to cephalosporins are insensitive to cephalosporins, including cefazolin.
Pharmacokinetics
In oral administration cefazolin is not absorbed; therefore, the drug is used only parenterally. After intramuscular (i.m.) administration cefazolin is quickly absorbed from the injection site compared to most other cephalosporins, plasma concentrations of the drug are higher and remain longer. After a 1.0 g injection or intravenous (IV) injection, plasma concentrations of the drug are altered.
The drug’s binding to plasma proteins is 70-90%. Cefazolin penetrates well into various organs and tissues, including lungs, liver, skin and soft tissue, joints, heart, peritoneum, middle ear, tonsils, gall bladder wall, appendix as well as into body fluids. Very high concentrations of the drug are created in the kidneys – after administration of 1.0 g of cefazolin its concentration in the urine reaches 4000 mcg/ml. In absence of biliary obstruction, 90-120 minutes after drug administration, cefazolin is detected in bile at higher concentration than in blood plasma. It should be taken into account that in patients with impaired patency of the biliary tract, concentration of the drug in bile may be significantly lower than in plasma.
The drug penetrates through the placental barrier and is detected in breast milk. It penetrates into cerebrospinal fluid (CSF) in small amounts; against inflammation of the dura mater the concentration of the drug in CSF is 0 – 0.4 µg/ml. The drug passes through capillary membranes in the bones and reaches bactericidal concentrations in both healthy and affected bones with osteomyelitis.
The drug concentration in joint fluid is comparable to that in blood plasma. In therapeutic concentrations it is found in ascitic and pleural fluid, inflammatory exudate.
_____________________
*In some regions the resistance rate of microorganisms may exceed 50%
**actual data on the prevalence of resistance are not available, in studies (older than 5 years) reported on the resistance rate of microorganisms > 50%
***in outpatient settings, the prevalence of resistance is less than 10%
Cefazolin is not metabolized in humans. Most of the administered drug is excreted with urine by glomerular filtration and tubular secretion in microbiologically active form. During the first 6 hours after administration, 60-90% of the drug is excreted with urine, during the day – 70-95% of the administered dose. A small part of the drug is excreted with bile. The elimination half-life in patients with renal dysfunction (T1/2) may be prolonged to 20-40 hours.
Indications
Bacterial infections caused by microorganisms sensitive to cefazolin:
respiratory tract infections;
urinary and genital tract infections;
biliary tract infections;
infections of the skin, soft tissues, bones and joints, including osteomyelitis;
bacterial endocarditis, sepsis;
intraoperative prevention of the development of infections (prophylactic administration of cefazolin can reduce the likelihood of developing an infection in the postoperative period).
Antibiotic susceptibility in vitro varies across geographic regions and over time, so local resistance information must be taken into account when choosing antibiotic therapy. If possible, the sensitivity of the pathogen to antibacterial drugs should be determined. Therapy can be started empirically, pending the results of an antibiotic susceptibility test.
Pharmacological effect
Pharmacotherapeutic group: antibiotic – cephalosporin.
ATX code: [J01DB04].
Pharmacological properties
Pharmacodynamics
Cephalosporin semisynthetic antibiotic of the first generation for parenteral use. It acts bactericidal, blocking penicillin-binding proteins (for example, transpeptidases), disrupts the synthesis of the cell wall of microorganisms. Has a wide spectrum of action. The prevalence of acquired resistance may vary geographically and may also change over time, and local information should be taken into account, especially when treating severe infections.
Microorganisms sensitive to cefazolin.
Gram-positive aerobes: Staphylococcus aureus (sensitive to methicillin), Staphylococcus saprophyticus, Streptococcus pneumoniae, Streptococcus agalactiae, Streptococcus pyogenes, Corynebacterium diphtheria, Bacillus anthracis.
Gram-negative microorganisms: Veisseria meningitides, Neisseria gonorrhoeae, Shigella spp., Salmonella spp., Treponema spp., Leptospira spp.
Microorganisms moderately sensitive to cefazolin.
Gram-positive aerobes: Staphylococcus aus, Staphylococcus epidermidis, Staphylococcus haemolyticus*, Staphylococcus hominis*, Streptococcus pneumonia* (moderately sensitive to penicillins).
Gram-negative aerobes: Escherichia coli, Haemophilus influenza**, Klebsiella oxytoca***, Klebsiella pneumoniae, Proteus mirabilis.
Microorganisms that are naturally resistant to cefazolin.
Gram-positive aerobes: Enterococcus spp. , Staphylococcus aureus (resistant to methicillin), Staphylococcus pneumoniae (resistant to penicillin).
Gram-negative aerobes: Acinetobacter baumanii, Citrobacter freundii, Enterobacter spp., Morganella morganii, Moraxella catarrhalis, Proteus vulgaris, Pseudomonas aeruginosa, Serratia marcescens, Stenotrophomonas maltophilia.
Anaerobes: Bacteroides fragilis.
Other microorganisms: Chlamydia spp., Chlamydophila spp., Legionella spp., Mycoplasma spp.
Penicillin-resistant Streptococcus pneumoniae due to cross-resistance to cephalosporins is insensitive to cephalosporins, including cefazolin.
Pharmacokinetics
When taken orally, cefazolin is not absorbed, so the drug is used only parenterally. After intramuscular (IM) administration, cefazolin is rapidly absorbed from the injection site, compared with most other cephalosporins, drug concentrations in blood plasma are higher and last longer. After intramuscular or intravenous (IV) administration of 1.0 g of the drug, its concentration in the blood plasma changes.
The binding of the drug to blood plasma proteins is 70 – 90%. Cefazolin penetrates well into various organs and tissues, including the lungs, liver, skin and soft tissues, joints, heart, peritoneum, middle ear, tonsils, gallbladder wall, appendix, as well as into physiological body fluids. Very high concentrations of the drug are created in the kidneys – after administration of 1.0 g of cefazolin, its concentration in the urine reaches 4000 mcg/ml. In the absence of biliary obstruction, 90-120 minutes after administration of the drug, cefazolin is found in bile in higher concentrations than in blood plasma. It should be taken into account that in patients with impaired patency of the biliary tract, the concentration of the drug in the bile may be significantly lower than the plasma concentration.
The drug penetrates the placental barrier and is found in breast milk. Penetrates into the cerebrospinal fluid (CSF) in small quantities; against the background of inflammation of the pia mater, the concentration of the drug in the CSF is 0 – 0.4 mcg/ml. The drug passes through the capillary membranes in the bones and reaches bactericidal concentrations in both healthy and osteomyelitis-affected bones.
The concentration of the drug in the joint fluid is comparable to the concentration in the blood plasma. In therapeutic concentrations it is found in ascitic and pleural fluids, inflammatory exudate.
_____________________
*in some regions the frequency of microorganism resistance may exceed 50%
**current data on the prevalence of resistance are not available; studies (more than 5 years old) have reported a resistance rate of microorganisms > 50%
***in community settings, the prevalence of resistance does not exceed 10%
Cefazolin is not metabolized in the human body. Most of the administered drug is excreted in the urine due to glomerular filtration and tubular secretion in a microbiologically active form. During the first 6 hours from the moment of administration, 60-90% of the drug is excreted in the urine, and within 24 hours – 70-95% of the administered dose. A small part of the drug is excreted from the body along with bile. The half-life in patients with impaired renal function (T1/2) can be extended to 20 – 40 hours.
Special instructions
Patients with a history of allergic reactions to penicillins or carbapenems may have increased sensitivity to cephalosporin antibiotics. If allergic reactions develop, administration of the drug should be stopped and appropriate desensitizing therapy should be prescribed.
If renal failure develops, the dose of the drug should be reduced and further treatment should be carried out under the control of the dynamics of urea nitrogen and creatinine in the blood.
During treatment with cefazolin, it is possible to obtain positive direct and indirect Coombs tests, as well as a false positive urine reaction to sugar.
When prescribing the drug, exacerbation of gastrointestinal diseases, especially colitis, is possible.
When thawed, the solution remains stable for 10 days when stored in a refrigerator (5 degrees C) or 48 hours at room temperature.
The safety of use in premature infants and children in the first year of life has not been established.
Active ingredient
Cefazolin
Composition
Powder for preparing a solution for intravenous and intramuscular administration.
Active ingredient: Cefazolin sodium in terms of cefazolin – 1.0 g.
Contraindications
hypersensitivity to cefazolin;
a history of severe hypersensitivity reactions (for example, anaphylactoid reactions) to cephalosporins or any other beta-lactam antibiotics (penicillins, monobactams, carbapenems);
neonatal period up to 1 month, including premature babies.
When using lidocaine solution as a solvent, see instructions for use of lidocaine.
With caution
Concomitant use of other nephrotoxic drugs, history of mild hypersensitivity reactions to penicillins.
Chronic renal failure, intestinal diseases (including a history of colitis), children’s age from 1 to 12 months.
Side Effects
In accordance with the classification of the World Health Organization (WHO), adverse reactions are presented according to the frequency of their development: very often (≥1/10); often (≥1/100, <1/10), infrequently (≥1/1000, 1/10000, <1/1000) and very rarely (<1/10000), frequency unknown - it was not possible to determine the frequency of occurrence based on available data.
Infections and parasitic infestations
uncommon: oral candidiasis (with long-term use);
rarely: genital candidiasis, vaginitis.
Blood and lymphatic system disorders
rarely: leukopenia, granulocytopenia, neutropenia, thrombocytopenia, leukocytosis, granulocytosis, monocytosis, lymphocytosis, thrombocytosis, lymphocytopenia, basophilia, eosinophilia. As a rule, these adverse events are short-term and reversible; very rarely: blood clotting disorders and, as a result, increased bleeding, anemia, agranulocytosis, aplastic anemia, pancytopenia, hemolytic anemia.
Immune system disorders
uncommon: fever, arthralgia;
very rarely: anaphylactic shock (development of laryngeal edema with narrowing of the airway, increased heart rate, shortness of breath, drop in blood pressure, swelling of the tongue, swelling of the face, anal and/or genital itching).
Metabolic and nutritional disorders
rarely: hyperglycemia or hypoglycemia.
Nervous system disorders
uncommon: development of seizures (in patients with impaired renal function when using the drug in high doses if the dosage regimen is not followed);
rarely: dizziness, malaise, general weakness, nightmares, vertigo, hyperactivity, nervousness or anxiety, insomnia or drowsiness, impaired color vision, confusion, increased convulsive activity of the brain.
Vascular disorders
rarely: “hot flashes”.
Respiratory, thoracic and mediastinal disorders
rarely: pleural effusion, chest pain, bronchospasm, shortness of breath, cough, development of acute respiratory distress syndrome, rhinitis.
Gastrointestinal disorders
often: loss of appetite, diarrhea, nausea, vomiting, abdominal pain;
very rarely: development of pseudomembranous colitis. This condition requires immediate initiation of treatment (see also section “Special Instructions”).
Liver and biliary tract disorders
rarely: transient increase in the activity of “liver” transaminases: alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase, gamma-glutamyltransferase, lactate dehydrogenase, increased concentration of bilirubin in the blood plasma, transient hepatitis, cholestatic jaundice.
Skin and subcutaneous tissue disorders
often: rash;
uncommon: erythema, exudative (multimorphic) erythema, urticaria, itching, angioedema (Quincke’s edema);
rarely: toxic epidermal necrolysis (Lyell’s syndrome), malignant exudative erythema (Stevens-Johnson syndrome).
Renal and urinary tract disorders
rarely: interstitial nephritis, proteinuria, transient increase in plasma urea concentration (usually in patients receiving therapy in combination with other nephrotoxic drugs), unspecified nephropathy and other manifestations of nephrotoxicity.
Influence on the results of laboratory and instrumental studies
frequency unknown: false-positive Coombs test, hypercreatininemia, increased prothrombin time, false-positive urine test for glucose.
General disorders and reactions at the injection site
often: pain at the injection site after intramuscular injection, sometimes with the development of compaction;
uncommon: thrombophlebitis and phlebitis – with intravenous administration.
Interaction
Cefazolin can reduce the effectiveness of oral contraceptives. For this reason, additional contraceptive measures should be used during treatment with the drug.
Cefazolin should not be co-administered with other antibacterial drugs that have a bacteriostatic effect (for example, tetracyclines, sulfonamides, erythromycin, chloramphenicol), since in vitro studies would reveal antagonism between these drugs.
When used together with cefazolin, the nephrotoxic properties of other antibacterial drugs (for example, aminoglycosides, colistin, polymyxin B), iodine-containing contrast agents, high doses of methotrexate, some antiviral drugs (for example, acyclovir, foscarnet), pentamidine, cyclosporine, tacrolimus, platinum-containing drugs and diuretics (for example, furosemide). If it is necessary to use them together with cefazolin, renal function should be carefully monitored.
When used simultaneously with loop diuretics (for example, furosemide), the tubular secretion of cefazolin is blocked, which leads to an increase in its concentration in the blood plasma. For this reason, the combined use of these drugs should be avoided.
When cefazolin and probenecid are co-administered, the renal clearance of cefazolin is reduced, which leads to an increase in the elimination time of the drug and an increase in its plasma concentration.
In rare cases, cephalosporins can cause bleeding disorders.
If combined use with oral anticoagulants is necessary, especially in high doses, coagulogram parameters should be monitored.
Some cephalosporin antibiotics, for example, cefamandole, cefotetan and cefazolin, by suppressing intestinal microflora, can disrupt the metabolism of vitamin K, which reduces its formation in the body, especially in patients with an initial deficiency.
Vitamin K supplements may be required.
When used simultaneously with drugs that reduce platelet aggregation (for example, nonsteroidal anti-inflammatory drugs), the risk of bleeding increases.
Cefazolin may cause disulfiram-like reactions when used concomitantly with ethanol.
Cefazolin is pharmaceutically incompatible with aminoglycoside antibiotics (gentamicin, kanamycin, amikacin, etc.), tetracyclines (oxytetracycline, tetracycline, etc.), sodium colistimethate, polymyxin B, erythromycin (in the form of glucoheptonate salt), barbituric derivatives (amobarbital, pentobarbital), bleomycin, calcium salts (calcium glucoheptonate, calcium gluconate), cimetidine, ascorbic acid.
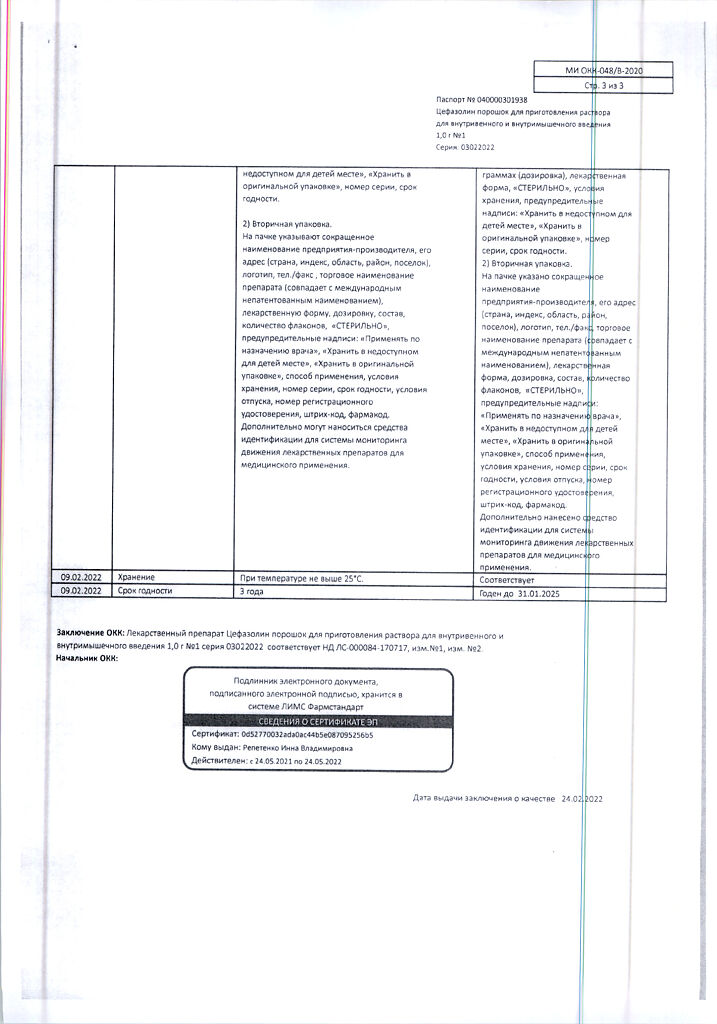
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 5°C.
Shelf life
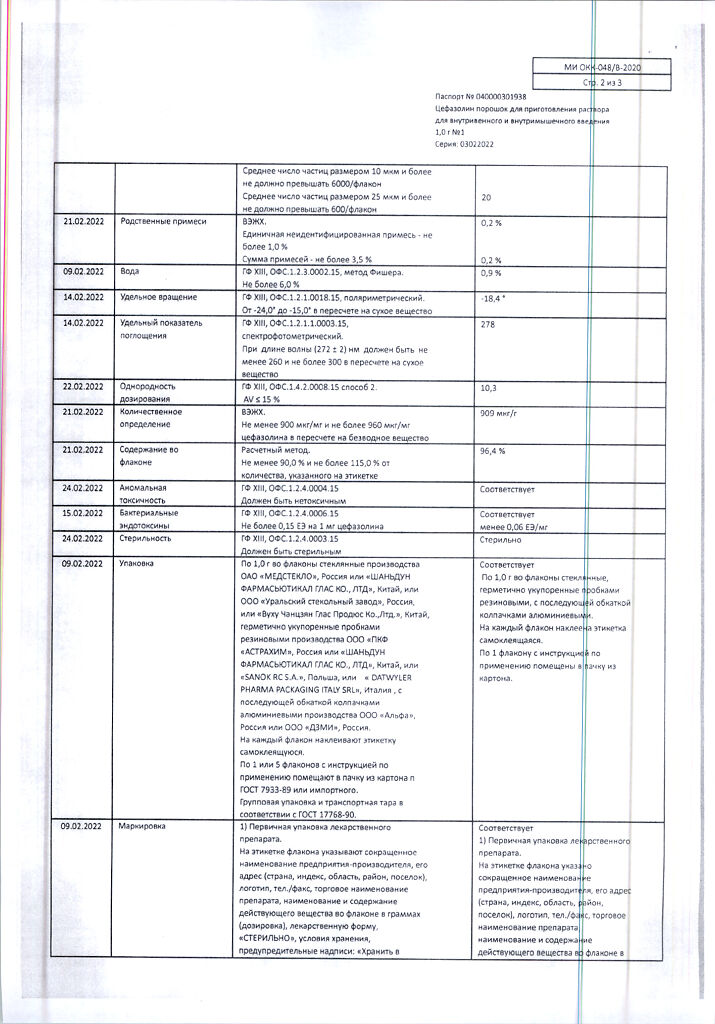
3 years.
Do not use after the expiration date stated on the package.
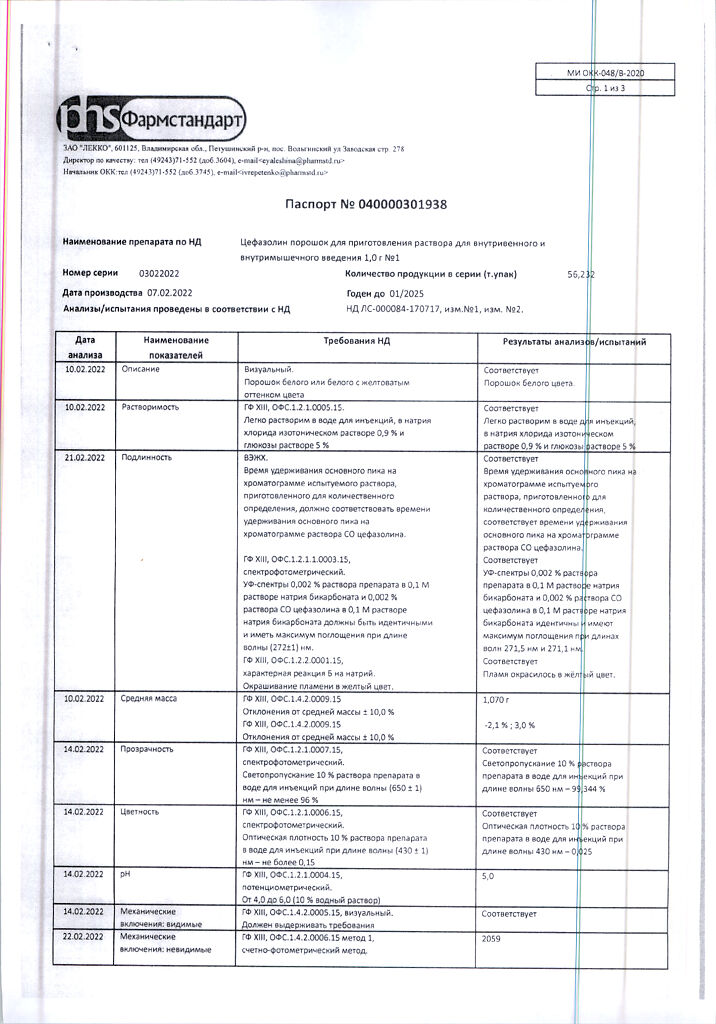
Manufacturer
Lecco CJSC, Russia
| Shelf life | 3 years. Do not use after the expiration date printed on the package. |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 5 ° C. |
| Manufacturer | Lekko ZAO, Russia |
| Medication form | Powder for preparation of solution |
| Brand | Lekko ZAO |
Related products
Buy Cefazolin, 1 g with delivery to USA, UK, Europe and over 120 other countries.