No products in the cart.
Carvedilol-Teva, tablets 6.25mg 30 pcs.
€5.92 €5.27
Description
Pharmacodynamics
Carvedilol blocks alpha-1-, beta-1- and beta-2-adrenoreceptors. It has vasodilatory, antianginal and antiarrhythmic effects. The vasodilatory effect is mainly due to blockade of alpha 1-receptors. Due to vasodilatation, it reduces total peripheral vascular resistance (TPRR). It has no sympathomimetic activity of its own and has membrane stabilizing properties.
The combination of vasodilation and blockade of beta-adrenoreceptors leads to the following effects: in patients with arterial hypertension the decrease of arterial pressure (AP) is not accompanied with increase of PPS, peripheral blood flow does not decrease (unlike beta-adrenoblockers). HR decreases insignificantly.
In patients with CHD it has antianginal action. It decreases pre- and post-loading on the heart. It has no expressed effect on lipid metabolism and the content of potassium, sodium and magnesium in the blood plasma. In patients with left ventricular dysfunction or circulatory insufficiency, it has a favorable effect on hemodynamic parameters and improves the ejection fraction and left ventricular size. It has an antioxidant effect by eliminating free oxygen radicals.
Pharmacokinetics
Carvedilol is rapidly and almost completely absorbed after oral administration from the gastrointestinal tract. It is almost completely bound to blood plasma proteins (98-99%). The plasma concentration is proportional to the dose taken. Bioavailability is about 25% due to high metabolism in the liver. Metabolites with high ability to block beta-adrenoreceptors are formed.
The maximum concentration in plasma is reached after 1 hour. The elimination half-life is 6-10 hours.
In elderly patients, the plasma concentration of carvedilol is approximately 50% higher than in younger patients. It is excreted mainly with bile. In patients with impaired liver function the bioavailability may increase to 80%. It penetrates through the placental barrier and is excreted with breast milk. Food slows absorption of the drug, but does not affect its bioavailability.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
1 tablet contains:
How to take, the dosage
How to take, the dosage
Ingestion, after meals, with water.
The dose of the drug is chosen individually. The treatment should start with low doses, gradually increasing until the optimal clinical effect is achieved. After the first administration of Carvedilol-Teva and after each dose increase to exclude possible arterial hypotension, it is recommended to measure the blood pressure 1 hour after taking the drug.
The therapy with Carvedilol-Teva should be stopped gradually, reducing the dose over 1-2 weeks.
If more than 2 weeks elapse after stopping therapy, it is recommended that the drug be restarted again at a lower dose.
Arterial hypertension
The initial dose is 12.5 mg once daily in the morning for the first 2 days, then 25 mg once daily. Subsequently, if necessary, the dose can be increased at intervals of at least 2 weeks, up to a maximum daily dose of 50 mg per day (divided into 2 doses).
Ischemic heart disease: prophylaxis of stable angina attacks The initial dose is 12.5 mg twice a day for the first 2 days, then 25 mg twice a day (morning and evening).
Chronic heart failure II and III functional class according to NYHA classification
The dose is adjusted individually, the doctor must be closely observed. The patient’s condition should be monitored during the first 2-3 hours after the first administration of the drug or after the first dose increase. The dose and use of other agents, such as digoxin, diuretics and angiotensin-converting enzyme (ACE) inhibitors should be adjusted before starting therapy with Carvedilol-Teva.
Patients should take the tablets with meals (to reduce the risk of orthostatic hypotension). The recommended starting dose is 3.125 mg twice daily. If this dose is well tolerated, it can be gradually (at 2 week intervals) increased to 6.25 mg twice a day, then to 12.5 mg twice a day, then to 25 mg twice a day.
Patients take the maximum tolerated dose. The maximum recommended dose for patients weighing less than 85 kg is 25 mg 2 times a day and for patients weighing more than 85 kg, 50 mg 2 times a day. Patients with chronic heart failure in order to prevent orthostatic hypotension are recommended to take the drug with meals. Before each increase of the dose the physician should examine the patient for possible increase of symptoms of chronic heart failure or vasodilatation.
If there is a transient increase in symptoms of chronic heart failure or fluid retention in the body, the dose of diuretics should be increased, although sometimes a reduction in the dose of Carvedilol-Teva or its temporary withdrawal is required. The dose of Carvedilol-Teva should not be increased until the symptoms of worsening heart failure or arterial hypotension are stabilized. If treatment with Carvedilol-Teva is interrupted for more than 1 week, its use should be resumed in a lower dose and then increased in accordance with the above recommendations. If treatment with Carvedilol-Teva has been interrupted for more than 2 weeks, therapy should be resumed at a dose of 3.125 mg twice daily, then the dose should be adjusted according to the above recommendations.
Elderly patients
There is no need for dose adjustment.
Patients with impaired renal function
The current data on pharmacokinetics in patients with various degrees of renal impairment (including renal failure) suggest that no dosage adjustment of Carvedilol is required in moderate to severe renal impairment.
Interaction
Interaction
Carvedilol may potentiate the effect of other simultaneously taken antihypertensive agents or drugs that have a hypotensive effect (nitrates).
In concomitant use of Carvedilol and diltiazem, cardiac conduction abnormalities and hemodynamic disorders may develop.
The concomitant use of carvedilol and digoxin increases the concentration of the latter and may increase atrioventricular conduction time.
Carvedilol may potentiate the effects of insulin and oral hypoglycemic agents, and the symptoms of hypoglycemia (especially tachycardia) may mask, therefore regular monitoring of blood sugar levels is recommended in diabetic patients.
Microsomal oxidation inhibitors (cimetidine) enhance and inducers (phenobarbital, rifampicin) weaken the hypotensive effect of carvedilol.
Drugs that reduce catecholamines (reserpine, monoamine oxidase inhibitors) increase the risk of arterial hypotension and marked bradycardia.
Concomitant use of cyclosporine increases the concentration of the latter (correction of the daily dose of cyclosporine is recommended).
The concomitant administration of clonidine may potentiate the antihypertensive and cardiac rhythm-relieving effects of carvedilol.
General anesthetics increase the negative inotropic and hypotensive effects of carvedilol.
Special Instructions
Special Instructions
The therapy should be prolonged and should not be stopped abruptly, especially in patients with coronary heart disease, as this may worsen the course of the underlying disease. If necessary, reduction of the drug dose should be gradual, over 1-2 weeks.
At the beginning of therapy with carvedilol or when increasing the drug dose, patients, especially elderly patients, may have an excessive decrease in blood pressure, predominantly when standing up. Correction of the drug dose is necessary. Patients with chronic heart failure may experience an increase in symptoms of heart failure and edema when adjusting the dose. In this case the dose of carvedilol should not be increased, it is recommended to prescribe high doses of diuretics until the patient’s condition stabilizes.
Continuous monitoring of electrocardiogram and blood pressure is recommended with simultaneous administration of carvedilol and slow calcium channel blockers, phenylalkylamine derivatives (verapamil) and benzodiazepine (diltiazem), and also with class I antiarrhythmic agents.
It is recommended to monitor renal function in patients with chronic renal failure, arterial hypotension and chronic heart failure.
If surgery is performed using general anesthesia, the anesthesiologist should be advised of prior therapy with Carvedilol.
Carvedilol does not affect blood glucose concentration and does not cause changes in glucose tolerance test in patients with insulin-independent diabetes mellitus.
At the time of treatment avoid the use of ethanol.
Patients with pheochromocytoma should be prescribed alpha-adrenoblockers before therapy.
Patients who wear contact lenses should note that the drug may cause decreased tear production.
It is not recommended to drive at the beginning of therapy and when increasing the dose of carvedilol. Other activities requiring high concentration and rapid psychomotor reactions should be refrained from.
Contraindications
Contraindications
With caution
Bronchospastic syndrome, chronic bronchitis, pulmonary emphysema, Prinz-metal angina, thyrotoxicosis, peripheral vascular occlusive disease, pheochromocytoma, psoriasis, renal failure, grade I atrioventricular block, extensive surgery and general anesthesia, diabetes, hypoglycemia, depression, myasthenia.
Side effects
Side effects
Central nervous system: headache, dizziness, syncopal states, muscle weakness (more often at the beginning of treatment), sleep disorders, depression, paresthesias.
Cardiovascular system disorders: bradycardia, orthostatic hypotension, angina pectoris, atrioventricular blockade, rare – “intermittent” claudication, peripheral circulation disorders, progression of heart failure.
Gastro-intestinal tract: dry mouth, nausea, abdominal pain, diarrhea or constipation, vomiting, increased “liver” transaminase activity.
Hematopoietic disorders: thrombocytopenia, leukopenia.
Urinary system disorders: severe renal dysfunction, edema.
Allergic reactions: skin allergic reactions (exanthema, urticaria, itching, rash), exacerbation of psoriatic rash, sneezing, nasal congestion, bronchospasm, shortness of breath (in predisposed patients).
Others: flu-like syndrome, pain in the extremities, decreased lacrimation, increased body weight.
Overdose
Overdose
Symptoms: decreased blood pressure (accompanied by dizziness or fainting), bradycardia. Dyspnea due to bronchospasm and vomiting may occur. In severe cases, cardiogenic shock, respiratory distress, confusion, conduction disorders are possible.
Treatment: monitoring and correction of vital signs should be carried out, if necessary – in the intensive care unit. Treatment is symptomatic. Intravenous use of m-cholinoblockers (atropine), adrenomimetics (epinephrine, norepinephrine) is advisable.
Pregnancy use
Pregnancy use
There have been no controlled studies of Carvedilol use in pregnant women; therefore, the drug may be administered to this category of patients only when the benefit to the mother exceeds the potential risk to the fetus.
Breastfeeding during treatment with Carvedilol is not recommended.
Similarities
Similarities
Additional information
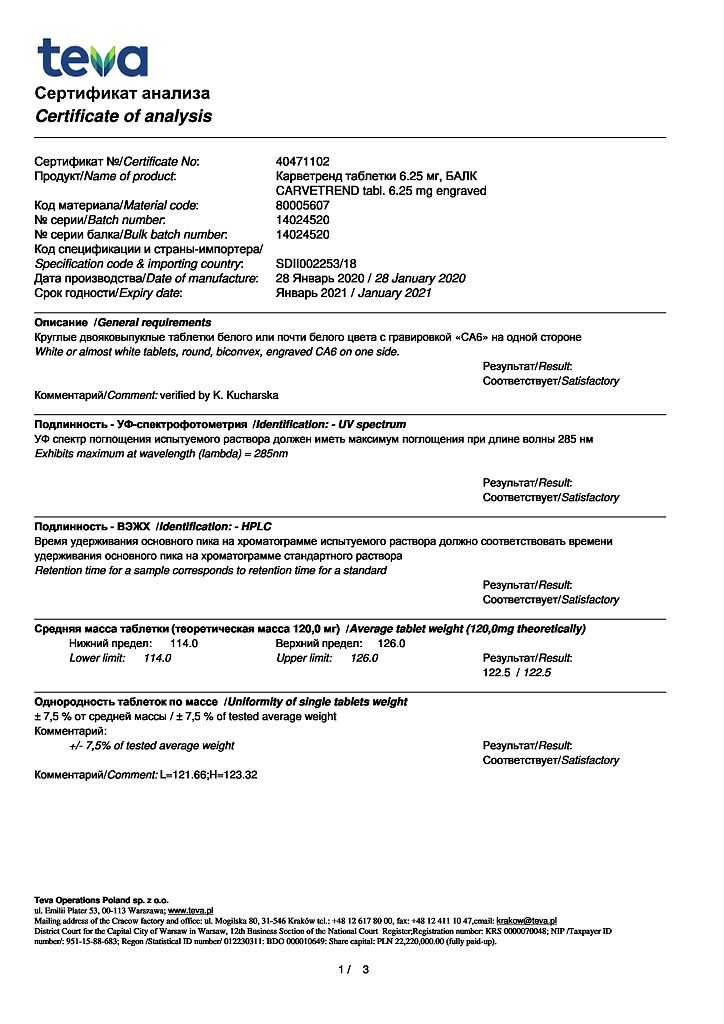
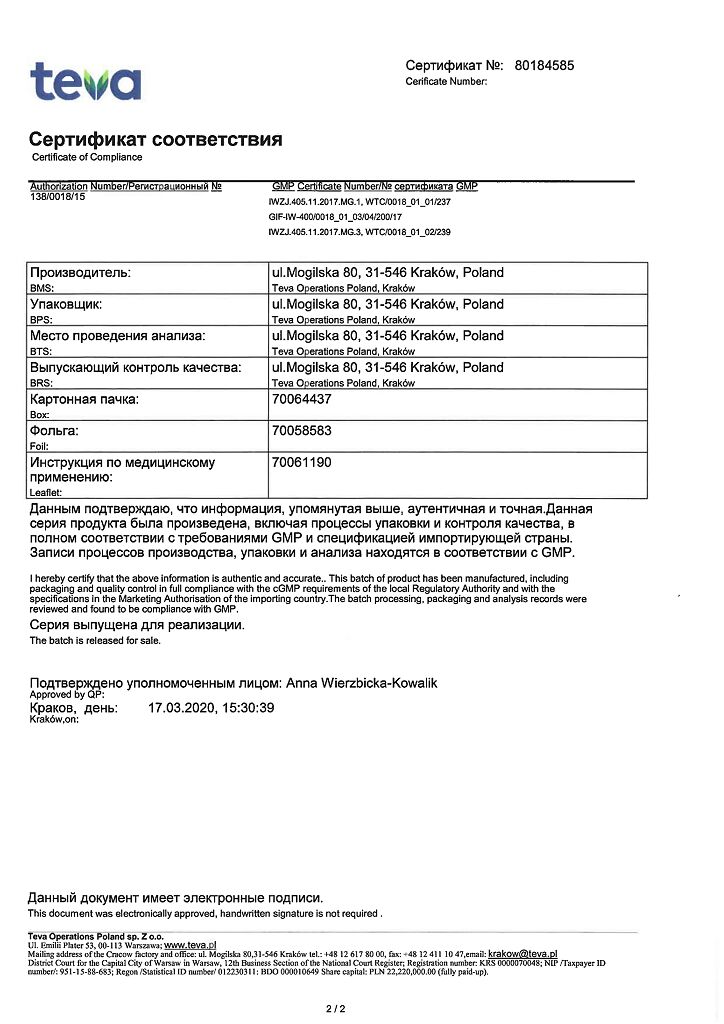
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a light-protected place, at a temperature not exceeding 25 °C |
| Manufacturer | Teva Operations Poland Sp. z o.o., Poland |
| Medication form | pills |
| Brand | Teva Operations Poland Sp. z o.o. |
Related products
Buy Carvedilol-Teva, tablets 6.25mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.