No products in the cart.
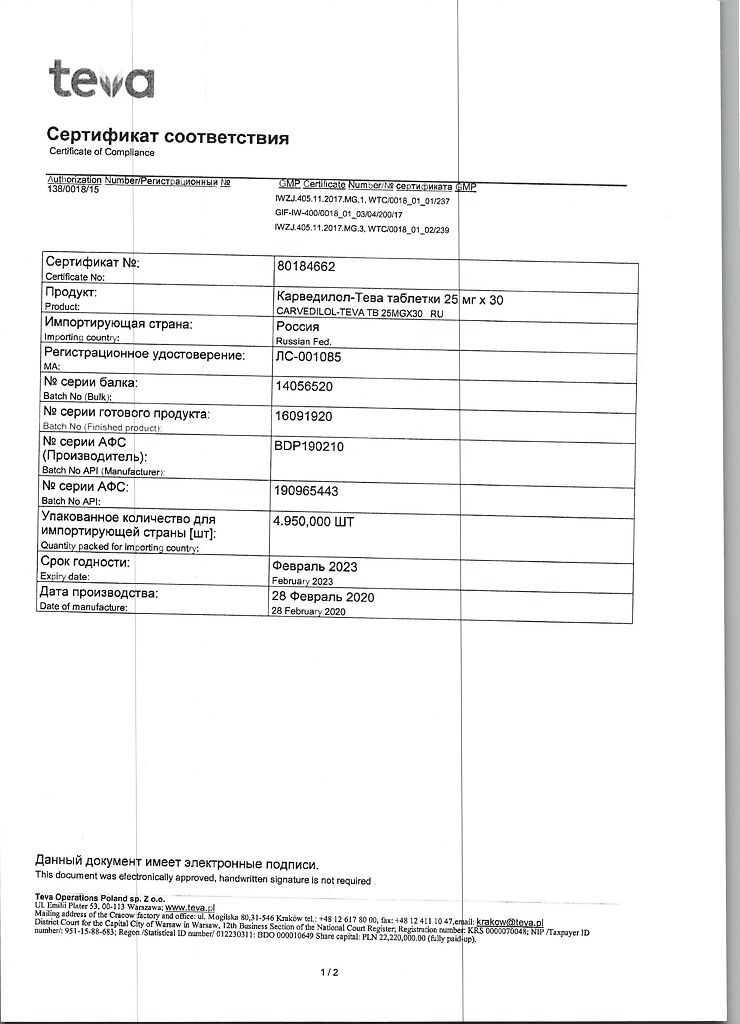
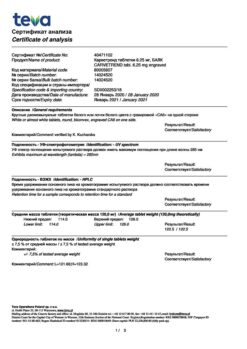
Carvedilol-Teva, tablets 25 mg 30 pcs
€8.29 €7.25
Description
Pharmacotherapeutic group: alpha and beta adrenoblocker
ATX code: C07AG02
Pharmacological properties
Pharmacodynamics. Carvedilol is a blocker of alpha1-, beta1-, beta2-adrenoreceptors, has an organoprotective effect. It has antiproliferative properties against the smooth muscle cells of the vascular walls; it is a racemic mixture of R(+) and S(-) stereoisomers, each with the same alpha-adrenoblocking properties. Due to the cardione-selective blocking of adrenoreceptors caused by the S(-) stereoisomer, carvedilol reduces blood pressure (BP), decreases heart rate (HR) and cardiac output, reduces pressure in the pulmonary arteries and in the right atrium. Due to blockade of alpha1-adrenoreceptors it causes peripheral vasodilation and reduces peripheral vascular resistance (PVR). It reduces the load on the heart muscle and prevents the development of angina attacks. In patients with chronic heart failure (CHF), it increases left ventricular ejection fraction and reduces the severity of disease symptoms. Similar effects are noted in patients with impaired left ventricular function.
Carvedilol has no intrinsic sympathomimetic activity and, like propranololol, has the property of membrane stabilization. The activity of the renin-angiotensin-aldosterone system (RAAS) is reduced, reducing the release of renin, so fluid retention (characteristic of selective alpha-adrenoblockers) rarely develops. The effect on BP and HR is most pronounced 1 to 2 hours after taking the drug.
Carvedilol has no adverse effect on lipid profile, maintaining normal ratio of high and low density lipoproteins (HDL/LDL).
In patients with arterial hypertension and renal disease, carvedilol reduces renal vascular resistance without significant changes in glomerular filtration rate, renal plasma flow or electrolyte excretion. Peripheral blood flow is preserved, so that the coldness of the hands and feet, often noted with beta-adrenoblockers, rarely develops.
Pharmacokinetics. Carvedilol is rapidly absorbed after oral administration.
The maximum plasma concentration of carvedilol (Cmax) is reached after 1 hour. The absolute bioavailability of carvedilol is approximately 25%: carvedilol is a racemate consisting of two enantiomers, the S-stereoisomer is metabolized faster than the R-stereoisomer, the absolute bioavailability when ingested is 15% and 31%, respectively, the maximum plasma concentration of the R-stereoisomer is approximately 2 times higher than the S-stereoisomer.
Carvedilol has a high lipophilicity. Approximately 98-99% of it binds to plasma proteins. The volume of distribution is approximately 2 L/kg and is increased in patients with cirrhosis due to decreased “primary passage” effect through the liver.
Carvedilol is metabolized primarily in the liver by oxidation and conjugation to form a number of metabolites. It is metabolized by “first passage” through the liver.
The metabolism of carvedilol by oxidation is stereoselective. The R(+) isomer is metabolized primarily by the CYP2D6 and CYP1A2 isoenzymes, and the S(-) isomer primarily by the CYP2D9 isoenzyme and, to a lesser extent, by the CYP2D6 isoenzyme. Other cytochrome P450 isoenzymes involved in the metabolism of carvedilol include CYP3A4, CYP2E1, CYP2C19 isoenzymes.
The results of studies on the pharmacokinetics of carvedilol in humans have shown that the CYP2D6 isoenzyme plays a significant role in the metabolism of the R and S stereoisomers of carvedilol. Plasma concentrations of R and S stereoisomers are increased in patients with low CYP2D6 isoenzyme activity. The results of population pharmacokinetic studies confirmed the importance of CYP2D6 isoenzyme genotype in the pharmacokinetics of R and S stereoisomers of carvedilol. Thus, it was concluded that the genetic polymorphism of the CYP2D6 isoenzyme has some clinical relevance.
Demethylation and hydroxylation of the phenolic ring produce 3 metabolites that have less pronounced vasodilatory properties than carvedilol.
The elimination half-life (T½) is about 6 h, plasma clearance is about 500-700 ml/min. Carvedilolol is eliminated mainly in bile through the intestine and partially by the kidneys as metabolites.
Patient age has no statistically significant effect on the pharmacokinetics of carvedilol.
In patients with cirrhosis the bioavailability of Carvedilol increases by 80% due to reduced metabolism during “first passage” through the liver.
Carvedilolol penetrates through the placental barrier and into breast milk. Carvedilolol is almost not removed from the blood plasma by hemodialysis.
Indications
Indications
Arterial hypertension (in monotherapy or in combination with other antihypertensive drugs).
Coronary heart disease: prevention of attacks of stable angina.
Chronic heart failure of functional class II and III according to the NYHA classification (as part of combination therapy with diuretics, digoxin or angiotensin-converting enzyme inhibitors).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: alpha and beta adrenergic blocker
ATX code: C07AG02
Pharmacological properties
Pharmacodynamics. Carvedilol is a blocker of alpha1-, beta1-, beta2-adrenergic receptors and has an organoprotective effect. It has antiproliferative properties against smooth muscle cells of the vascular walls, is a racemic mixture of R (+) and S (-) stereoisomers, each of which has the same alpha-adrenergic blocking properties. Due to the cardionon-selective blocking of adrenergic receptors caused by the S(-) stereoisomer, carvedilol lowers blood pressure (BP), reduces heart rate (HR) and cardiac output, reduces pressure in the pulmonary arteries and in the right atrium. Due to the blockade of alpha1-adrenergic receptors, it causes peripheral vasodilation and reduces peripheral vascular resistance (PVR). Reduces the load on the heart muscle and prevents the development of angina attacks. In patients with chronic heart failure (CHF), it increases the left ventricular ejection fraction and reduces the severity of symptoms of the disease. Similar effects were noted in patients with impaired left ventricular function.
Carvedilol does not have intrinsic sympathomimetic activity and, like propranolol, has membrane stabilizing properties. The activity of the renin-angiotensin-aldosterone system (RAAS) is reduced, reducing the release of renin, so fluid retention (characteristic of selective alpha-blockers) rarely develops. The effect on blood pressure and heart rate is most pronounced 1 to 2 hours after taking the drug.
Carvedilol does not adversely affect the lipid profile, maintaining a normal ratio of high-density lipoprotein to low-density lipoprotein (HDL/LDL).
In patients with arterial hypertension and kidney disease, carvedilol reduces renal vascular resistance without significant changes in glomerular filtration rate, renal plasma flow or electrolyte excretion. Peripheral blood flow is preserved, so cold hands and feet, often noted when taking beta-blockers, rarely develops.
Pharmacokinetics. Carvedilol is rapidly absorbed after oral administration.
The maximum concentration of carvedilol in blood plasma (Cmax) is achieved after 1 hour. The absolute bioavailability of carvedilol is about 25%: carvedilol is a racemate consisting of two enantiomers, the S-stereoisomer is metabolized faster than the R-stereoisomer, the absolute bioavailability after oral administration is 15% and 31%, respectively, the maximum plasma concentration of the R-stereoisomer is approximately 2 times higher than the S-stereoisomer.
Carvedilol is highly lipophilic. Approximately 98-99% of it binds to blood plasma proteins. The volume of distribution is approximately 2 L/kg and is increased in patients with cirrhosis due to a decrease in the first pass effect through the liver.
Carvedilol is metabolized primarily in the liver by oxidation and conjugation to form a number of metabolites. Metabolized during the “first pass” through the liver.
The metabolism of carvedilol by oxidation is stereoselective. The R(+) isomer is metabolized mainly by the CYP2D6 and CYP1A2 isoenzymes, and the S(-) isomer mainly by the CYP2D9 isoenzyme and, to a lesser extent, by the CYP2D6 isoenzyme. Other isoenzymes of cytochrome P450 involved in the metabolism of carvedilol include isoenzymes CYP3A4, CYP2E1, CYP2C19.
The results of studies of the pharmacokinetics of carvedilol in humans showed that the CYP2D6 isoenzyme plays a significant role in the metabolism of the R and S stereoisomers of carvedilol. Plasma concentrations of R and S stereoisomers increase in patients with low CYP2D6 isoenzyme activity. The results of population pharmacokinetic studies confirmed the importance of the genotype of the CYP2D6 isoenzyme in the pharmacokinetics of R and S stereoisomers of carvedilol. Thus, it was concluded that the genetic polymorphism of the CYP2D6 isoenzyme has some clinical significance.
As a result of demethylation and hydroxylation of the phenolic ring, 3 metabolites are formed, which have less pronounced vasodilating properties than carvedilol.
The half-life (T½) is about 6 hours, plasma clearance is about 500-700 ml/min. Carvedilol is excreted mainly with bile through the intestines and partially by the kidneys in the form of metabolites.
Patient age does not have a statistically significant effect on the pharmacokinetics of carvedilol.
In patients with liver cirrhosis, the bioavailability of carvedilol increases by 80% due to a decrease in the severity of first-pass metabolism through the liver.
Carvedilol penetrates the placental barrier and into breast milk. Carvedilol is almost not removed from blood plasma during hemodialysis.
Special instructions
Special instructions
The drug Carvedilol-Teva is recommended to be taken for the treatment of CHF, as an addition to standard therapy for CHF with diuretics, ACE inhibitors or cardiac glycosides, only after selecting the dose of the diuretic. It can also be used in patients intolerant to ACE inhibitors.
At the beginning of therapy with Carvedilol-Teva or after increasing its dose, orthostatic hypotension and dizziness, sometimes with syncope, may sometimes develop, especially in patients with heart failure, elderly patients and those taking other antihypertensive drugs or diuretics at the same time. These effects can be prevented by using an initial low dose of Carvedilol-Teva and gradually increasing to a maintenance dose, as well as taking the drug with food. Patients should be explained how to avoid orthostatic hypotension (get up carefully from a lying or sitting position; if dizziness develops, sit or lie down).
Patients with CHF can take Carvedilol-Teva only if their condition is successfully controlled with drugs from the group of cardiac glycosides and/or diuretics. If during treatment the course of CHF worsens, it is necessary to increase the dose of the diuretic, and reduce the dose of Carvedilol-Teva or temporarily stop its use (see section “Dosage and Administration”).
Alpha and beta blockers can mask the symptoms of hypoglycemia in patients with diabetes mellitus, as well as the manifestations of thyrotoxicosis in patients with thyroid diseases, reducing the manifestations of tachycardia. In patients with CHF, blood glucose concentrations may increase or decrease.
When performing general anesthesia for patients taking alpha- and beta-blockers, it is necessary to use narcotic analgesics with minimal inotropic effect, or first (gradually!) cancel the alpha- and beta-blocker.
In some cases, carvedilol may cause liver dysfunction. If liver failure develops, the use of Carvedilol-Teva should be discontinued. As a rule, after discontinuation of the drug, liver function returns to normal.
Alpha and beta blockers for COPD can aggravate bronchial obstruction, so they should not be used in patients with COPD.
Alpha and beta blockers can worsen the clinical picture of peripheral arteriopathy, psoriasis and anaphylactic reactions and enhance the body’s reaction during allergy tests.
Alpha and beta blockers can provoke pain in patients with Prinzmetal’s angina.
Patients with pheochromocytoma can take alpha- and beta-blockers only after alpha-blocker therapy has been initiated.
If therapy with Carvedilol-Teva (as with other alpha and beta blockers) is abruptly discontinued, increased sweating, tachycardia, shortness of breath and worsening of angina may develop. Patients most at risk for these reactions are those with angina pectoris, who may develop myocardial infarction. When discontinuing the drug Carvedilol-Teva, the dose is reduced gradually over 1-2 weeks.
If more than 2 weeks have passed since stopping therapy, it is recommended to resume taking the drug at low doses.
Patients wearing contact lenses should be aware that the drug may cause a decrease in tear production.
If the number of heart contractions decreases to 50 beats/min, the drug should be discontinued.
The drug Carvedilol-Teva is not recommended for patients under 18 years of age, because The effectiveness and safety of Carvedilol-Teva in this group of patients has not been established.
Impact on the ability to drive vehicles and machinery
Care must be taken when driving vehicles and engaging in potentially hazardous activities, due to the fact that side effects may develop that can affect concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Carvedilol
Composition
Composition
1 tablet contains-
active ingredient: carvedilol 3.125 mg, 6.25 mg, 12.50 mg or 25.00 mg;
excipients: microcrystalline cellulose 28.000/56.00/112.00/224.00 mg, lactose monohydrate 16.770/33.54/67.08/134.16 mg, low-substituted hyprolose 4.545/9.09/18.18/36.36 mg, corn starch 6.360/12.72/25.44/50.88 mg, talc 0.300/0.60/1.20/2.40 mg, colloidal silicon dioxide 0.340/0.68/1.36/2.72 mg, magnesium stearate 0.560/1.12/2.24/4.48 mg.
Pregnancy
Pregnancy
Data on the use of Carvedilol-Teva during pregnancy are limited.
Animal studies indicate reproductive toxicity; potential risk to humans is unknown.
Beta-blockers reduce placental blood flow, have an adverse effect on the development of the embryo, and can cause arterial hypotension, bradycardia and hypoglycemia in the fetus.
Carvedilol-Teva should not be used during pregnancy unless absolutely necessary and the potential benefit to the mother justifies the risk to the fetus.
It is unknown whether carvedilol passes into breast milk, but most lipophilic beta-blockers are excreted into breast milk to varying degrees. If it is necessary to use the drug Carvedilol-Teva during lactation, breastfeeding should be stopped.
Contraindications
Contraindications
Hypersensitivity to carvedilol or other components of the drug; chronic obstructive pulmonary disease (COPD); bronchial asthma or bronchospasm (history); chronic heart failure of functional class IV according to the NYHA classification, acute and chronic heart failure (CHF) in the stage of decompensation, requiring intravenous administration of inotropic agents; Prinzmetal’s angina; cardiogenic shock; severe bradycardia (less than 50 beats/min at rest), sick sinus syndrome (including sinoauricular block), atrioventricular (AV) block of II-III degree (except for patients with an artificial pacemaker); end-stage occlusive peripheral vascular disease; clinically significant liver dysfunction, metabolic acidosis; patients receiving intravenous therapy with verapamil or diltiazem, due to the possibility of developing severe bradycardia (less than 40 beats/min) and arterial hypotension; severe arterial hypotension (systolic blood pressure less than 85 mm Hg); lactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome; breastfeeding period; age under 18 years (safety and effectiveness have not been established), pheochromocytoma (without simultaneous use of alpha-blockers).
With caution
AV blockade of the first degree, diabetes mellitus, hypoglycemia, thyrotoxicosis, occlusive diseases of peripheral vessels, pheochromocytoma (with simultaneous use of alpha-blockers), depression, myasthenia gravis, psoriasis, extensive surgical interventions, general anesthesia, renal failure, pregnancy.
Side Effects
Side Effects
The incidence of side effects that develop when taking carvedilol is classified according to the recommendations of the World Health Organization: very often – at least 10%; often – at least 1%, but less than 10%; infrequently – not less than 0.1%, but less than 1%; rarely – not less than 0.01%, but less than 0.1%; very rarely – less than 0.01%, including individual messages.
The incidence of some side effects, such as dizziness, marked decrease in blood pressure, bradycardia and visual disturbances, is dose-dependent. These effects develop more often in patients with CHF. The most common side effect of carvedilol is dizziness with or without orthostatic hypotension, which occurs in approximately 6% of patients.
If serious side effects develop, treatment with the drug should be discontinued.
From the hematopoietic and lymphatic systems: rarely – thrombocytopenia; very rarely – leukopenia.
From the nervous system: very often – dizziness, headache (especially at the beginning of treatment); often – depressed mood, depression; rarely – sleep disturbances, changes in mood/thought, paresthesia, myasthenia gravis, loss of consciousness.
From the senses: often – decreased lacrimation and eye irritation (pay attention when using contact lenses); very rarely – visual disturbances, eye irritation.
From the cardiovascular system: very often – heart failure, orthostatic hypotension; often – peripheral vascular disease, increased blood pressure, anemia, syncope, presyncope, bradycardia; rarely – worsening of heart failure (especially with increasing dose), coldness of the hands and feet, decreased blood pressure, fainting, conduction disturbances, palpitations, worsening of angina, occlusive disorders of the peripheral circulation, intermittent claudication, peripheral edema.
From the respiratory system: often – pneumonia, bronchitis, upper respiratory tract infections, pulmonary edema; rarely – shortness of breath, bronchospasm (in predisposed patients), nasal congestion.
From the digestive system: often – nausea, abdominal pain (up to 2%), diarrhea, dry oral mucosa; rarely – loss of appetite, vomiting, flatulence, constipation; very rarely – dryness of the oral mucosa, increased activity of “liver” transaminases (alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyltransferase).
From the skin: infrequently – skin lesions such as psoriasis and lichen planus; very rarely – exacerbation of psoriasis, alopecia, exfoliative dermatitis.
From the musculoskeletal system: rarely – pain in muscles, bones, spine.
From the urinary system: often – urinary tract infections, renal failure and impaired renal function in patients with diffuse vasculitis and/or impaired renal function; rarely – urinary disorders; very rarely – severe renal dysfunction.
From the metabolic side: often – weight gain, hypercholesterolemia, in patients with existing diabetes mellitus – hyperglycemia or hypoglycemia; rarely – increased triglyceride concentrations
Other: often – pain, general weakness; uncommon – hypersensitivity reactions (itching, rash, urticaria), decreased potency; very rarely – “flushes” of blood to the skin of the face, sneezing, flu-like syndrome.
Rare cases of urinary incontinence in women have been reported, reversible after discontinuation of the drug.
During post-marketing use of carvedilol, serious skin reactions were identified – toxic epidermal necrolysis, Stevens-Johnson syndrome.
Interaction
Interaction
During treatment with Carvedilol-Teva, patients are not recommended to drink alcohol, because ethanol may potentiate the side effects of carvedilol.
When carvedilol and digoxin are taken concomitantly, the concentration of digoxin in the blood plasma increases by approximately 16% and AV conduction time may increase. At the beginning of therapy with carvedilol, when selecting its dose or discontinuing the drug, regular monitoring of the concentration of digoxin in the blood plasma is recommended.
Carvedilol may potentiate the effect of insulin and oral hypoglycemic agents, including sulfonylureas, and the symptoms of hypoglycemia (especially tachycardia) may be masked; therefore, regular monitoring of blood glucose concentrations is recommended in patients with diabetes mellitus.
Carvedilol enhances the effect of antihypertensive drugs (ACE inhibitors, thiazide diuretics, vasodilators).
Concomitant use with drugs that reduce the content of catecholamines (reserpine, monoamine oxidase inhibitors) increases the risk of a pronounced decrease in blood pressure and severe bradycardia.
When carvedilol was used in renal transplant patients who developed chronic vascular graft rejection, a moderate increase in mean cyclosporine trough concentrations was observed. To maintain cyclosporine concentrations within the therapeutic range, the dose of cyclosporine had to be reduced in approximately 30% of patients (on average by 20%), and no dose adjustment was required in the remaining patients. Due to the marked individual variations in the required daily dose of cyclosporine, careful monitoring of cyclosporine plasma concentrations is recommended after initiation of carvedilol therapy and, if necessary, appropriate adjustment of the daily dose of cyclosporine.
Concomitant use of carvedilol with blockers of “slow” calcium channels (dihydropyridine derivatives) can lead to severe heart failure and severe arterial hypotension.
Sympathomimetics, which have alpha- and beta-adrenomimetic effects, when used simultaneously with carvedilol, increase the risk of arterial hypertension and severe bradycardia.
Verapamil, diltiazem and other antiarrhythmic drugs (propranolol, amiodarone), when used simultaneously with carvedilol, may increase the risk of AV conduction disorders.
With the simultaneous use of carvedilol and diltiazem, isolated cases of conduction disturbances were observed (rarely with disturbances in hemodynamic parameters). As with other drugs with beta-blocking properties, the use of carvedilol together with calcium channel blockers such as verapamil and diltiazem is recommended under ECG and blood pressure monitoring.
Concomitant use with clonidine may potentiate the antihypertensive and negative chromotropic effects of carvedilol.
Inhibitors of microsomal oxidation (cimetidine, ketoconazole, fluoxetine, haloperidol, verapamil, erythromycin) enhance, and inducers (barbiturates, rifampicin) weaken the hypotensive effect of carvedilol.
Nitrates and beta-blockers (eg, in the form of eye drops) may potentiate the antihypertensive effect of carvedilol.
General anesthesia agents enhance the negative inotropic and hypotensive effects of carvedilol.
Ergotamine increases vasoconstriction when used simultaneously with carvedilol.
Nonsteroidal anti-inflammatory drugs reduce the antihypertensive effect of carvedilol.
Overdose
Overdose
Symptoms: marked decrease in blood pressure (systolic blood pressure 80 mm Hg or less), severe bradycardia (less than 50 beats/min), respiratory dysfunction (including bronchospasm), heart failure, cardiogenic shock, cardiac arrest, generalized convulsions, vomiting, confusion.
Treatment: it is necessary to monitor and correct the vital functions of the body, if necessary, in the intensive care unit.
During the first hours after an overdose, induce vomiting and rinse the stomach. Place the patient on his back (with legs elevated), for severe bradycardia – atropine 0.5-2 mg intravenously, for treatment-resistant bradycardia, an operation to install an artificial cardiac pacemaker is indicated; with a pronounced decrease in blood pressure – norepinephrine (norepinephrine); for bronchospasm, beta-agonists are used for inhalation (if ineffective – intravenously) or aminophylline intravenously.
For seizures, diazepam or clonazepam is administered slowly intravenously.
Since in case of severe overdose with symptoms of shock, the half-life of carvedilol may be prolonged and carvedilol may be removed from the depot, it is necessary to continue maintenance therapy for a sufficiently long time. The duration of maintenance therapy depends on the severity of the overdose and should be continued until the patient’s clinical condition has stabilized.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Teva Operations Poland Sp. z o.o., Poland
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C. Keep out of the reach of children. |
| Manufacturer | Teva Operations Poland Sp. z o.o., Poland |
| Medication form | pills |
| Brand | Teva Operations Poland Sp. z o.o. |
Other forms…
Related products
Buy Carvedilol-Teva, tablets 25 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.