No products in the cart.
Description
Pharmacotherapeutic group: antitumor drug, antimetabolite
ATX code: L01BC06
Pharmacological properties
Pharmacodynamics
Capecitabine is a fluoropyrimidine carbamate derivative, an oral cytostatic that is activated in tumor tissue and has a selective cytotoxic effect on it. In vitro capecitabine has no cytotoxic effect, in vivo it is converted into fluorouracil (FU), which undergoes further metabolism. PV formation occurs mainly in tumor tissue under the action of tumor angiogenic factor – thymidine phosphorylase, which minimizes the systemic effect of PV on healthy tissues of the body. Sequential enzymatic biotransformation of capecitabine into FP creates higher concentrations of the drug in tumor tissues than in the surrounding healthy tissues. After oral administration of capecitabine by a patient with colorectal cancer (N=8), the concentration of FP in tumor tissue was 3.2 times higher than its concentration in the surrounding healthy tissue (range 0.9 to 8.0).
The ratio of PV concentrations in tumor tissue to plasma was 21.4 (range 3.9 to 59.9), the ratio of its concentration in healthy tissues to plasma was 8.9 (range 3.0 to 25.8). Thymidine phosphorylase activity in the primary colorectal tumor is also 4 times higher than in adjacent healthy tissues.
Tumor cells from patients with breast, stomach, colorectal, cervical and ovarian cancers contain more thymidine phosphorylase capable of converting 5′-DFUR (5′-deoxy-5-fluoruridine) to FA than the corresponding healthy tissues.
Both healthy and tumor cells metabolize PV into 5-fluoro-2-deoxyuridine monophosphate (FDUMP) and 5-fluorouridine triphosphate (FUTP). These metabolites damage cells through two different mechanisms. First, FDUMF and the folate cofactor M5-10-methyltetrahydrofolate bind to thymidylate synthase (TS) to form a covalently bound tertiary complex. This binding inhibits the formation of thymidylate from uracil. Thymidylate is an essential precursor of thymidine triphosphate, which, in turn, is crucial for DNA synthesis, so that deficiency of this substance can lead to inhibition of cell division.
Second, during RNA synthesis, the core transcription enzymes can mistakenly include FUTP instead of uridine triphosphate (UTP). This metabolic “mistake” disrupts RNA processing and protein synthesis.
Pharmacokinetics
Intake
. After oral administration, capecitabine is rapidly and completely absorbed from the gastrointestinal tract (GIT), followed by its transformation into the metabolites, 5′-deoxy-5-fluorocytidine (5-DFCT) and 5′-DFUR. Simultaneous intake of food decreases the rate of absorption of capecitabine, but the area under the curve “concentration-time” (AUC) of 5′-DFTCT and the following metabolite, FP, is not significantly affected. When the drug was administered at a dose of 1250 mg/m² after a meal, the maximum plasma concentrations (Cmax) of capecitabine, 5′-DFCT, 5′-DFUR, FU, and the inactive metabolite alpha-fluorobeta alanine (FBAL) at day 14 were 4.47; 3.05; 12.1; 0.95 and 5.46 µg/mL, respectively. The time to reach was 1.5; 2.0; 2.0; 2.0 and 3.34 h, and the AUC0-∞ was 7.75; 7.24; 24.6; 2.03 and 36.3 μgxh/mL, respectively.
Distribution (protein binding)
In vitro studies in human plasma have shown that for capecitabine, 5′-DFCT, 5′-DFUR and FU the binding to proteins (mainly to albumin) is 54%, 10%, 62% and 10%, respectively
./p>
Metabolism
Metabolized in the liver under the influence of carboxylesterase to the metabolite 5′-DFCTC, which is then transformed into 5′-DFUR under the action of cytidine deaminase, which is mainly located in the liver and tumor tissues. Further transformation to active cytotoxic metabolite FU occurs mainly in tumor tissue under the action of tumor angiogenic factor – thymidine phosphorylase.
The AUC for FU is 6-22 times lower than after intravenous jet injection of FU at a dose of 600 mg/m². Capecitabine metabolites become cytotoxic only after conversion to FU and FU metabolites.
FU is further catabolized to form inactive metabolites, dihydro-5-fluorouracil (FUN2), 5-fluorouraidopropionic acid (FUPC) and FBAL; this process occurs under the influence of dihydropyrimidine dehydrogenase (DPD), whose activity limits the reaction rate.
The elimination half-life (T1/2) of capecitabine, 5′-DPCT, 5′-DFUR, FU, and FBAL is 0.85; 1.11; 0.66; 0.76, and 3.23 hours, respectively. Pharmacokinetic parameters of capecitabine, 5′-DFCT and 5′-DFUR are the same on days 1 and 14. The AUC of FU increases by 30-35% by day 14, and no longer increases (day 22). In the range of therapeutic doses, pharmacokinetic parameters of capecitabine and its metabolites, except for FP, are dose-dependent. After oral administration of capecitabine its metabolites are excreted mainly by the kidneys – 95.5%, by the intestine – 2.6%. The main metabolite in the urine is FBL, which accounts for 57% of the dose taken.
About 3% of the dose taken is excreted unchanged by the kidneys.
Combination therapy
Capecitabine had no effect on the pharmacokinetics of docetaxel or paclitaxel (Cmax and AUC) and no effect of docetaxel or paclitaxel on the pharmacokinetics of 5′-DFUR (the main metabolite of capecitabine).
Pharmacokinetics in Special Patient Groups
Gender, presence or absence of liver metastases prior to treatment, patient’s general status index, total bilirubin concentration, serum albumin, alanine aminotransferase (ALT) and aspartate aminotransferase (ACT) activity in patients with colorectal cancer had no significant effect on the pharmacokinetics of 5′-DFUR, FU and FBAL.
Patients with hepatic impairment due to metastatic liver injury
In patients with mild to moderate hepatic impairment due to metastases, there is no clinically significant change in the pharmacokinetics and bioactivation of capecitabine. There are no data on pharmacokinetics in patients with severe hepatic impairment.
Patients with impaired renal function
The results of a pharmacokinetic study show that in various degrees (from mild to severe) of renal impairment the pharmacokinetics of unchanged drug and FP are independent of creatinine clearance (CK). CK affects the AUC of 5′-DFUR (35% increase in AUC when CK decreases by 50%) and FBL (114% increase in AUC when CK decreases by 50%). FBAL is a metabolite with no antiproliferative activity; 5′-DFUR is a direct precursor of FU.
Elderly patients
Age has no effect on the pharmacokinetics of 5′-DFUR and FU. The AUC of FBL increased with age (a 20% increase in patient age was accompanied by a 15% increase in AUC of FBL), which is probably due to changes in renal function.
Race
The pharmacokinetics of capecitabine in patients of the Negro race are not different from those in patients of the Caucasian race.
Indications
Indications
Breast cancer
combination therapy with docetaxel for locally advanced or metastatic breast cancer, when chemotherapy that includes an anthracycline drug is ineffective;
monotherapy for locally advanced or metastatic breast cancer resistant to chemotherapy with taxanes or anthracyclines, or if there are contraindications to them.
Colorectal cancer
adjuvant therapy for stage III colon cancer after surgical treatment;
therapy for metastatic colorectal cancer.
Stomach cancer
First-line therapy for advanced gastric cancer.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antitumor agent, antimetabolite
ATX code: L01BC06
Pharmacological properties
Pharmacodynamics
Capecitabine is a fluoropyrimidine carbamate derivative, an oral cytostatic agent that is activated in tumor tissue and has a selective cytotoxic effect on it. In vitro, capecitabine does not have a cytotoxic effect; in vivo, it is converted to fluorouracil (FU), which is further metabolized. The formation of FU occurs predominantly in tumor tissue under the influence of the tumor angiogenic factor – thymidine phosphorylase, which minimizes the systemic effect of FU on healthy tissues of the body. The sequential enzymatic biotransformation of capecitabine into FU creates higher concentrations of the drug in tumor tissues than in surrounding healthy tissues. After oral administration of capecitabine to a patient with colorectal cancer (N=8), the concentration of FU in tumor tissue was 3.2 times greater than its concentration in adjacent healthy tissue (range, 0.9 to 8.0).
The ratio of FU concentrations in tumor tissue and plasma is 21.4 (range from 3.9 to 59.9), the ratio of its concentration in healthy tissues and plasma is 8.9 (range from 3.0 to 25.8). Thymidine phosphorylase activity in a primary colorectal tumor is also 4 times higher than in adjacent healthy tissues.
Tumor cells from patients with breast, gastric, colorectal, cervical and ovarian cancer contain more thymidine phosphorylase, which can convert 5′-DFUR (5′-deoxy-5-fluorouridine) into FU, than in corresponding healthy tissues.
Both healthy and tumor cells metabolize FU into 5-fluoro-2-deoxyuridine monophosphate (FdUMP) and 5-fluorouridine triphosphate (FUTP). These metabolites damage cells through two different mechanisms. First, FdUMP and the folate cofactor M5-10-methylenetetrahydrofolate bind to thymidylate synthase (TS) to form a covalently linked tertiary complex. This binding inhibits the formation of thymidylate from uracil. Thymidylate is an essential precursor to thymidine triphosphate, which in turn is essential for DNA synthesis, so a deficiency of this substance can lead to inhibition of cell division.
Secondly, during RNA synthesis, nuclear transcription enzymes may mistakenly include FUTP instead of uridine triphosphate (UTP). This metabolic “error” disrupts RNA processing and protein synthesis.
Pharmacokinetics
Suction
After oral administration, capecitabine is rapidly and completely absorbed from the gastrointestinal tract (GIT), after which it is transformed into metabolites, 5′-deoxy-5-fluorocytidine (5-DFCT) and 5′-DFUR. Concomitant food intake reduces the rate of absorption of capecitabine, but the area under the concentration-time curve (AUC) of 5′-DFUR and the next metabolite, FU, is slightly affected. When taking the drug at a dose of 1250 mg/m² after a meal, the maximum plasma concentrations (Cmax) of capecitabine, 5′-DFCT, 5′-DFUR, FU and the inactive metabolite alpha-fluoro-beta alanine (FBAL) on the 14th day were 4.47, respectively; 3.05; 12.1; 0.95 and 5.46 µg/ml. The time to reach was 1.5; 2.0; 2.0; 2.0 and 3.34 hours, and AUC0-∞ – 7.75; 7.24; 24.6; 2.03 and 36.3 μgh/ml, respectively.
Distribution (protein binding)
An in vitro study in human plasma showed protein binding (mainly albumin) of 54%, 10%, 62% and 10% for capecitabine, 5′-DFCT, 5′-DFUR and FU, respectively.
Metabolism
Metabolized in the liver under the influence of carboxylesterase to the metabolite 5′-DFCT, which is then transformed into 5′-DFUR under the action of cytidine deaminase, located mainly in the liver and tumor tissues. Further transformation to the active cytotoxic metabolite FU occurs predominantly in tumor tissue under the influence of the tumor angiogenic factor – thymidine phosphorylase.
AUC for FU is 6-22 times less than after intravenous bolus administration of FU at a dose of 600 mg/m². Capecitabine metabolites become cytotoxic only after conversion to FU and FU metabolites.
Further, FU is catabolized to form inactive metabolites – dihydro-5-fluorouracil (FUN2), 5-fluororeidopropionic acid (FUPA) and FBAL; this process occurs under the influence of dihydropyrimidine dehydrogenase (DPD), the activity of which limits the rate of the reaction.
Removal
The half-life (T1/2) of capecitabine, 5′-DFCT, 5′-DFUR, FU and FBAL is 0.85, respectively; 1.11; 0.66; 0.76 and 3.23 hours, respectively. The pharmacokinetic parameters of capecitabine, 5′-DFCT and 5′-DFUR on days 1 and 14 are the same. The AUC of FU increases by 30-35% by the 14th day, and does not increase any further (day 22). In the range of therapeutic doses, the pharmacokinetic parameters of capecitabine and its metabolites, with the exception of FU, are dose-dependent. After taking capecitabine orally, its metabolites are excreted primarily by the kidneys – 95.5%, and by the intestines – 2.6%. The main metabolite in urine is FBAL, which accounts for 57% of the dose taken.
About 3% of the dose taken is excreted unchanged by the kidneys.
Combination therapy
There was no effect of capecitabine on the pharmacokinetics of docetaxel or paclitaxel (Cmax and AUC), or any effect of docetaxel or paclitaxel on the pharmacokinetics of 5′-DFUR (the main metabolite of capecitabine).
Pharmacokinetics in special groups of patients
Gender, the presence or absence of liver metastases before treatment, the index of the general condition of the patient, the concentration of total bilirubin, serum albumin, the activity of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) in patients with colon cancer did not have a significant effect on the pharmacokinetics of 5′-DFUR, FU and FBAL.
Patients with liver failure due to metastatic liver disease
In patients with mild to moderate liver dysfunction caused by metastases, there is no clinically significant change in the pharmacokinetics and bioactivation of capecitabine. Data on pharmacokinetics in patients with severe liver dysfunction are not available.
Patients with impaired renal function
The results of a pharmacokinetic study show that for varying degrees (from mild to severe) renal failure, the pharmacokinetics of the unchanged drug and FU are independent of creatinine clearance (CC). CC affects the AUC value of 5′-DFUR (increase in AUC by 35% – with a decrease in CC by 50%) and FBAL (increase in AUC by 114% with a decrease in CC by 50%). FBAL is a metabolite that does not have antiproliferative activity; 5′-DFUR is the immediate precursor of FU.
Elderly patients
Age does not affect the pharmacokinetics of 5′-DFUR and FU. FBAL AUC increased with age (a 20% increase in patient age was accompanied by a 15% increase in FBAL AUC), which is likely due to changes in renal function.
Race
The pharmacokinetics of capecitabine in black patients does not differ from that in Caucasian patients.
Special instructions
Special instructions
Dose-limiting adverse reactions are diarrhea, abdominal pain, nausea, stomatitis and hand-foot syndrome.
It is necessary to conduct careful medical monitoring for manifestations of toxicity in patients receiving therapy with capecitabine. Most adverse events are reversible and do not require complete discontinuation of the drug, although it may be necessary to adjust the dose or temporarily discontinue the drug.
Diarrhea: Treatment with Capecitabine may cause diarrhea, sometimes severe. Patients with severe diarrhea should be closely monitored, and if dehydration develops, rehydration or replacement of electrolytes should be performed. Standard antidiarrheal drugs (eg, loperamide) should be prescribed as early as medically indicated. According to the criteria of the National Cancer Institute of Canada (NCIC CTC, version 2), grade 2 diarrhea is defined as an increase in stool frequency up to 4-6 times a day or bowel movements at night, grade 3 diarrhea is defined as an increase in stool frequency up to 7-9 times a day or fecal incontinence and malabsorption syndrome, grade 4 diarrhea is defined as an increase in stool frequency up to 10 or more times a day, the appearance of visible blood in the stool, or the need for parenteral maintenance therapy. If necessary, reduce the dose of capecitabine.
Dehydration: Dehydration should be prevented or corrected as soon as it occurs. Dehydration can develop quickly in patients with anorexia, asthenia, nausea, vomiting or diarrhea.
Dehydration may cause acute renal failure, in some cases fatal, especially in patients with impaired renal function at the time of initiation of therapy or if the patient is taking capecitabine concomitantly with drugs that have nephrotoxic effects.
If grade 2 or higher dehydration develops, treatment with Capecitabine should be immediately interrupted and rehydration performed. Treatment should not be resumed until rehydration is completed and the factors that caused it are eliminated or corrected. The dose of the drug should be modified in accordance with the recommendations for adverse events leading to dehydration.
The spectrum of cardiotoxicity with capecitabine is similar to that with other fluoropyrimidines and includes myocardial infarction, angina, arrhythmias, cardiac arrest, heart failure and ECG changes, including cases of QT prolongation. These adverse events are more typical for patients suffering from coronary artery disease. Caution must be exercised in patients with a history of arrhythmia and angina pectoris.
During therapy with capecitabine, the development of hypo- or hypercalcemia was observed. Caution should be exercised when treating capecitabine in patients with previously diagnosed hypo- or hypercalcemia.
Caution should be exercised when treating patients with diseases of the central and peripheral nervous system with capecitabine (for example, in the presence of brain metastases or neuropathy), as well as in patients with diabetes mellitus and fluid and electrolyte imbalances, since during treatment with capecitabine, exacerbation of these diseases is possible.
In rare cases, unexpected severe toxicities (eg, stomatitis, diarrhea, neutropenia, and neurotoxicity) associated with FU are due to insufficient dihydropyrimidine dehydrogenase (DPD) activity. Thus, a connection between reduced DPD activity and more severe, potentially lethal FU toxicity cannot be ruled out.
During treatment with capecitabine, close monitoring should be performed for ocular complications such as keratitis and corneal lesions, especially in patients with a history of ocular disease. Treatment of the identified pathology should be carried out in accordance with the clinical situation. A manifestation of skin toxicity of the drug Capecitabine is the development of palmoplantar syndrome (synonyms – palmoplantar erythrodysesthesia or acral erythema caused by chemotherapy). The median time to toxicity in patients receiving capecitabine monotherapy was 79 days (range, 11 to 360 days), and severity ranged from grade 1 to grade 3. Hand-foot syndrome of the 1st degree does not interfere with the patient’s daily activities and is manifested by numbness, dysesthesia/paresthesia, tingling or redness of the palms and/or soles, and discomfort.
Grade 2 hand-foot syndrome is characterized by painful redness and swelling of the hands and/or feet, and the discomfort caused by these symptoms interferes with the patient’s daily activities. Grade 3 hand-foot syndrome is defined as moist desquamation, ulceration, blistering and sharp pain in the hands and/or feet, as well as severe discomfort that makes it impossible for the patient to carry out any daily activities. If grade 2 or 3 hand-foot syndrome occurs, capecitabine therapy should be interrupted until symptoms disappear or decrease to grade 1. If grade 3 syndrome occurs, subsequent doses of capecitabine should be reduced.
Vitamin B6 (pyridoxine) is not recommended for the symptomatic or secondary preventive treatment of hand-foot syndrome when using capecitabine in combination with cisplatin, as it may reduce the effectiveness of cisplatin. There is evidence of the effectiveness of dexapanthenol in preventing the development of hand-foot syndrome during therapy with capecitabine.
Capecitabine may cause hyperbilirubinemia. If, in connection with treatment with Capecitabine, hyperbilirubinemia >3.0 x ULN (upper limit of normal) or an increase in the activity of hepatic aminotransferases (ALT, AST) >2.5 x ULN is observed, treatment should be interrupted. Therapy can be resumed if the concentration of bilirubin and the activity of hepatic aminotransferases decrease below the specified limits.
In patients simultaneously taking Capecitabine and oral anticoagulants – coumarin derivatives, coagulation parameters (prothrombin time or INR) should be monitored and the dose of the anticoagulant should be adjusted accordingly.
Capecitabine can cause the development of serious skin reactions such as Stevens-Johnson syndrome and toxic epidermal necrolysis (Lyell’s syndrome), incl. with fatal outcome. If severe skin reactions develop while using capecitabine, the drug should be discontinued and not restarted.
Use of the drug in elderly and senile patients
The incidence of gastrointestinal toxicities in patients with colorectal cancer aged 60-79 years who received capecitabine monotherapy did not differ from that in the general patient population. In patients 80 years of age and older, reversible grade 3 and 4 gastrointestinal adverse events, such as diarrhea, nausea and vomiting, occurred more frequently. In patients ≥65 years of age receiving combination therapy with capecitabine and other antineoplastic agents, there was an increased incidence of grade 3 and 4 adverse reactions and adverse events leading to discontinuation of therapy compared with younger patients.
In an analysis of safety data in patients ≥60 years of age receiving combination therapy with capecitabine and docetaxel, there was an increase in the incidence of treatment-related grade 3 and 4 adverse events, serious adverse events, and early discontinuation of therapy due to adverse events compared with those in patients younger than 60 years of age.
Kidney failure
Caution should be exercised when prescribing capecitabine to patients with moderate renal impairment. As with fluorouracil treatment, the incidence of treatment-related grade 3 and 4 adverse events was higher in patients with moderate renal failure (creatinine clearance 30-50 ml/min).
Liver failure
Patients with hepatic impairment should be under close medical supervision during therapy with capecitabine. The effect of liver dysfunction not due to liver metastases or severe liver failure on the distribution of capecitabine is unknown.
Impact on the ability to drive vehicles and machinery
Some adverse reactions of the drug, such as dizziness, drowsiness or nausea, may adversely affect the ability to drive a car and perform potentially hazardous activities that require increased concentration and speed of psychomotor reactions. If the above adverse events occur, you should refrain from performing these activities.
Active ingredient
Active ingredient
Capecitabine
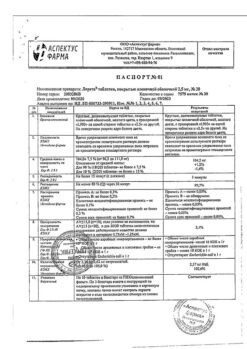
Composition
Composition
1 film-coated tablet contains:
Active ingredient:
capecitabine – 150.00 mg.
Excipients (core): microcrystalline cellulose – 78.00 mg; lactose monohydrate (milk sugar) – 59.40 mg; croscarmellose sodium – 9.00 mg; colloidal silicon dioxide – 2.10 mg; povidone-K25 – 4.50 mg; potato starch – 6.00 mg; magnesium stearate – 3.00 mg.
Shell composition: hypromellose – 5.13 mg; macrogol-4000 – 1.26 mg; titanium dioxide – 2.61 mg.
Pregnancy
Pregnancy
The drug is contraindicated for use during pregnancy and breastfeeding.
Reliable methods of contraception should be used during capecitabine therapy and for at least 3 months thereafter. If pregnancy occurs during therapy, the patient should be aware of the potential threat to the fetus.
Contraindications
Contraindications
Hypersensitivity to capecitabine or other components of the drug;
Hypersensitivity to fluorouracil or with a history of reported cases of unexpected or severe adverse reactions to treatment with fluoropyrimidine derivatives;
Established deficiency of dihydropyrimidine dehydrogenase (DPD), as for other fluoropyrimidines;
Concomitant use with sorivudine or its chemical analogues, for example, brivudine;
Severe liver failure;
Severe leukopenia, neutropenia (less than 1.5 × 109/l), thrombocytopenia (less than 100 × 109/l);
Severe renal failure (creatinine clearance less than 30 ml/min);
Pregnancy and breastfeeding period;
Children under 18 years of age (efficacy and safety of use have not been established).
If there are contraindications to any other drug in the combination therapy regimen, then this drug should not be used.
Side Effects
Side Effects
The most common side effects associated with capecitabine were gastrointestinal (GIT) disorders (diarrhea, nausea, vomiting, abdominal pain, stomatitis), hand-foot syndrome, fatigue, asthenia, anorexia, cardiotoxicity, worsening renal failure in patients with a history of renal impairment, and thrombosis/embolism. Side effects possibly causally related to the use of the drug are shown in Tables 4 and 5 indicating the frequency: very often (≥1/10), often (≥1/100-<1/10), infrequently (≥1/1000-<1/100), rarely (≥1/10000-<1/1000), very rarely (<1/10000).
Table 4. Adverse events reported in patients receiving capecitabine as monotherapy.
Organ systems
Very often (all degrees)
Often (all degrees)
Uncommon (severe and/or life-threatening (grades 3-4), or considered clinically significant)
Rarely
Infectious and parasitic diseases
–
Herpesvirus infections, nasopharyngitis, lower respiratory tract infections
Sepsis, urinary tract infections, cellulitis, tonsillitis, pharyngitis, candidiasis of the oral mucosa, influenza, gastroenteritis, fungal infections, infections, tooth abscess
–
Good quality-
new, malignant and unspecified neoplasms
–
–
Lipoma
–
From the blood and lymphatic system
–
Neutropenia, anemia
Febrile neutropenia, pancytopenia, granulocytopenia, thrombocytopenia, leukopenia, hemolytic anemia, increase in international normalized ratio, prolongation of prothrombin time
–
From the immune system
–
–
Increased sensitivity
–
Metabolism and nutrition
Anorexia
Dehydration, weight loss, loss of appetite
indigestion, diabetes mellitus, hypokalemia, hypertriglycerides-
demic
–
Mental disorders
–
Insomnia, depression
Confusion, panic attacks, decreased libido, depressed mood
–
From the nervous system
–
Headache, lethargy, dizziness (except vertigo), paresthesia, dysgeusia
Aphasia, memory impairment, ataxia, syncope, imbalance, sensory loss, peripheral neuropathy
–
From the side of the organ of vision
–
Increased lacrimation, conjunctivitis, eye irritation
Decreased visual acuity, diplopia
–
Hearing and labyrinth disorders
–
–
Vertigo, ear pain
–
From the side of the heart
–
–
Angina pectoris, incl. unstable, myocardial ischemia, arrhythmia, supraventricular arrhythmia (including atrial fibrillation), tachycardia, sinus tachycardia, palpitations
–
From the side of blood vessels
–
Thrombophlebitis
Deep vein thrombosis, increased/decreased blood pressure, petechiae, hot flashes, coldness of the distal extremities
–
From the respiratory system, chest organs and mediastinum
–
Shortness of breath, nosebleeds, cough, rhinorrhea
Pulmonary embolism, pneumothorax, hemoptysis, bronchial asthma, dyspnea on exertion
–
From the gastrointestinal tract
Diarrhea, vomiting, nausea, stomatitis (including ulcerative), abdominal pain
Gastrointestinal bleeding, constipation, upper abdominal pain, dyspepsia, flatulence, dry mouth
Intestinal obstruction, ascites, enteritis, gastritis, dysphagia, lower abdominal pain, esophagitis, abdominal discomfort, gastroeso-
phageal reflux, colitis, blood in stool
–
From the liver and biliary tract
–
Hyperbilirubi-
anemia, changes in liver function tests
Jaundice
–
From the skin and subcutaneous tissues
Palmoplantar erythrodysesthesia syndrome
Skin rash, alopecia, macular rash, erythema, dry skin, itching, skin hyperpigmentation, skin peeling, dermatitis, nail changes, pygmy disorder
Skin ulcers, blisters, radiation dermatitis, urticaria, photosensitive reactions
pregnancy, palmar erythema, facial edema, purpura
Skin cracks
From the musculoskeletal and connective tissue side
–
Limb pain, back pain, arthralgia
Joint swelling, bone pain, facial pain, joint stiffness, muscle weakness
–
From the kidneys and urinary tract
–
–
Hydronephrosis, urinary incontinence, hematuria, nocturia, increased plasma creatinine concentration
–
From the genital organs and breast
–
–
Vaginal bleeding
–
General and administration site disorders
Increased fatigue, asthenia, drowsiness
Fever, peripheral edema, malaise, weakness, chest pain
Swelling, chills, flu-like syndrome, fever, trembling.
–
Table 5. Adverse events reported in patients receiving capecitabine as part of combination therapy were in addition to those reported with capecitabine monotherapy or occurred at a higher frequency compared to capecitabine monotherapy.
Organ system
Very often (all degrees)
Often (all degrees)
Infectious and parasitic diseases
–
Herpes zoster, urinary tract infections, oral candidiasis, upper respiratory tract infections, rhinitis, influenza, infections, oral herpes
From the blood and lymphatic system
Neutropenia (including grade 3-4 neutropenia associated with fever above 38°C), leukopenia, anemia, thrombocytopenia
Myelosuppression, febrile neutropenia
From the immune system
–
Increased sensitivity
Metabolism and nutrition
Loss of body weight, loss of appetite
Hypokalemia, hyponatremia, hypomagnesemia, hypo/hypercalcemia, hyperglycemia
Mental disorders
–
Sleep disorders, anxiety
From the nervous system
Paresthesia, dysesthesia, peripheral neuropathy, peripheral sensory neuropathy, dysgeusia, headache
Neurotoxicity, tremor, neuralgia, hypoesthesia
From the side of the organ of vision
Increased tear production
Visual disturbances, blurred vision, dry eyes, eye pain
Hearing and labyrinth disorders
–
Ringing in the ears, hearing loss
From the side of the heart
–
Atrial fibrillation, myocardial ischemia (including myocardial infarction)
From the side of blood vessels
Edema of the lower extremities, increased blood pressure, thrombosis/embolism
Hyperemia, low blood pressure, hypertensive crisis, hot flashes, phlebitis
From the respiratory system, chest organs and mediastinum
Sore throat, laryngopharyngeal dysesthesia
Nosebleeds, rhinorrhea, pain in the pharynx and larynx, dysphonia
From the gastrointestinal tract
Constipation, dyspepsia
Upper gastrointestinal bleeding, hiccups, oral ulcers, gastritis, bloating, gastroesophageal reflux, oral pain, dysphagia, rectal bleeding, lower abdominal pain, dysesthesia, paresthesia and hypoesthesia in the mouth, abdominal discomfort
From the liver and biliary tract
–
Liver dysfunction
From the skin and subcutaneous tissues
Alopecia, nail changes
Hyperhidrosis, erythematous rash, urticaria, night sweats
From the musculoskeletal and connective tissue side
Myalgia, arthralgia, pain in limbs
Jaw pain, muscle spasms, trismus, muscle weakness
From the kidneys and urinary tract
–
Hematuria, proteinuria, decreased creatinine clearance, dysuria
General and administration site disorders
Fever, weakness, lethargy (grade 3-4), increased sensitivity to high and low temperatures
Pain, inflammation of the mucous membrane, pain in the extremities, chills, chest pain, flu-like syndrome, bruising
Laboratory and instrumental data
–
Hyperbilirubinemia, increased activity of alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, hypercreatininemia
Others
–
Contusion
Cases of liver failure and cholestatic hepatitis have been reported in clinical studies and with the use of capecitabine. A cause-and-effect relationship with capecitabine has not been established.
Post-registration experience
Visual disorders: rarely – unspecified stenosis of the lacrimal canaliculus, corneal damage, including keratitis, punctate keratitis.
Nervous system disorders: very rarely – toxic leukoencephalopathy.
From the liver and biliary tract: rarely – liver failure, cholestatic hepatitis.
Cardiac disorders: rarely – ventricular fibrillation, prolongation of the QT interval, ventricular tachysystolic arrhythmia of the “pirouette” type, bradycardia.
Vascular disorders: rarely – vasospasm.
From the skin and subcutaneous fat: rarely – systemic lupus erythematosus (cutaneous form); very rarely – Stevens-Johnson syndrome and toxic epidermal necrolysis.
From the kidneys and urinary tract: rarely – acute renal failure as a result of dehydration, including death.
Description of selected adverse drug reactions
Diarrhea
Diarrhea was observed in 50% of patients during capecitabine therapy. A meta-analysis of 14 clinical trials involving more than 4,700 patients treated with capecitabine identified covariates that were statistically associated with an increased risk of diarrhea: increasing the initial dose of capecitabine (in grams), increasing the study period of treatment (in weeks), increasing patient age (every 10 years), and female gender. Covariates statistically associated with a reduced risk of diarrhea: increasing the cumulative dose of capecitabine (0.1 • kg) and increasing the relative dose intensity in the first 6 weeks of treatment.
Patients with severe diarrhea should be closely monitored with rehydration and restoration of fluid and electrolyte balance if dehydration occurs. According to indications, it is recommended to take standard antidiarrheal drugs (for example, loperamide) as early as possible.
Cardiotoxicity
In addition to the side effects presented in Tables 4 and 5, the following adverse reactions were observed with capecitabine monotherapy with an incidence of less than 0.1%: cardiomyopathy, heart failure, sudden death and ventricular extrasystole.
Encephalopathy
During monotherapy with capecitabine, the development of encephalopathy was observed with an incidence of less than 0.1%.
Adverse reactions in special patient groups
Elderly patients
Elderly patients aged ≥60 years receiving capecitabine alone or in combination with docetaxel had an increased incidence of grade 3-4 adverse reactions and serious adverse reactions compared with patients aged <60 years. The majority of patients aged ≥60 years receiving combination therapy with docetaxel experienced earlier discontinuation of treatment due to adverse reactions compared with patients aged <60 years. A meta-analysis of 14 clinical studies involving more than 4,700 patients treated with capecitabine found that as the patient's age increased (every 10 years), the risk of developing hand-foot syndrome and diarrhea increased, while the risk of developing neutropenia, on the contrary, decreased.
Floor
In female patients, there is a statistically significant increase in the risk of developing hand-foot syndrome and diarrhea; the risk of developing neutropenia is reduced.
Patients with impaired renal function
Patients with pre-treatment renal impairment who received capecitabine monotherapy experienced an increased incidence of treatment-related grade 3 and 4 adverse reactions compared with patients with normal renal function. Patients with moderate renal insufficiency were more likely to require dose reductions compared to patients without renal insufficiency and with mild renal insufficiency, respectively, and were more likely to experience premature discontinuation of treatment.
Interaction
Interaction
Coumarin anticoagulants
In patients taking capecitabine concomitantly with coumarin anticoagulants (warfarin and phenprocoumon), coagulation abnormalities and/or bleeding have been reported several days to months after the start of capecitabine therapy, and in some cases within one month after its completion.
In a drug interaction study, following a single 20 mg dose of warfarin, capecitabine increased the AUC of S-warfarin by 57% and the international normalized ratio (INR) by 91%. In patients concomitantly taking capecitabine and coumarin anticoagulants, coagulation parameters (prothrombin time or INR) should be carefully monitored and the dose of the anticoagulant should be adjusted according to these parameters.
Cytochrome CYP2C9 substrates
No specific drug interaction studies have been conducted between capecitabine and other drugs metabolized by the CYP2C9 isoenzyme of the cytochrome P450 system. Caution should be exercised when administering capecitabine with these drugs.
Phenytoin
Increased plasma concentrations of capecitabine and phenytoin have been reported when administered concomitantly with capecitabine. Specific studies of drug-drug interactions between capecitabine and phenytoin have not been conducted, but it is assumed that the mechanism of interaction is based on the suppression of the CYP2C9 isoenzyme under the influence of capecitabine (see above “Coumarin anticoagulants”). In patients receiving concomitant phenytoin and capecitabine, phenytoin plasma concentrations should be regularly monitored.
Antacids
When assessing the pharmacokinetic parameters of capecitabine when taken simultaneously with antacids containing aluminum hydroxide and magnesium hydroxide, a slight increase in the concentration of capecitabine and one of the metabolites (5′-DFCT) in the blood plasma was noted. The three main metabolites of capecitabine (5′-DFUR, FU and FBAL) were not affected by the studied agents.
Calcium folinate (Leucovorin)
Calcium folinate does not affect the pharmacokinetic properties of capecitabine and its metabolites. However, it is possible that the toxic effect of capecitabine may be enhanced due to the effect of calcium folinate on the pharmacodynamics of capecitabine.
Sorivudin and its analogues
The literature describes a clinically significant drug interaction between sorivudine and FU, which is based on the inhibitory effect of sorivudine on DPD. This interaction can lead to a fatal increase in the toxicity of fluoropyrimidines. Therefore, capecitabine should not be used concomitantly with sorivudine or its structural analogues such as brivudine. A minimum of four weeks should be maintained between the end of therapy with sorivudine or its structural analogs (including brivudine) and the start of treatment with capecitabine.
Oxaliplatin
Clinically significant difference in exposure to capecitabine or oxaliplatin metabolites (free platinum or total platinum) when used in combination
capecitabine and oxaliplatin, regardless of the presence of bevacizumab, were not noted.
Bevacizumab
There was no clinically significant effect of bevacizumab on the pharmacokinetics of capecitabine or its metabolites.
Allopurinol
An interaction has been noted between allopurinol and FU with a possible decrease in the effectiveness of FU. In this regard, the simultaneous use of capecitabine and allopurinol should be avoided.
Interferon alpha
The maximum tolerated dose of capecitabine is 2000 mg/m² per day when co-administered with interferon 2-alpha (3 million IU/m² per day) compared to a capecitabine dose of 3000 mg/m² per day when administered alone.
Radiation therapy
The maximum tolerated dose of capecitabine in monotherapy with a standard dosing regimen is 3000 mg/m², when combined with radiation therapy in the treatment of colorectal cancer (with a continuous therapy regimen or 5-day courses from Monday to Friday for 6 weeks) – 2000 mg/m² per day.
Overdose
Overdose
Symptoms: Symptoms of acute overdose include nausea, vomiting, diarrhea, inflammation of the mucous membrane (mucositis), gastrointestinal irritation and bleeding, and bone marrow suppression.
Treatment: treatment of overdose should include a standard set of therapeutic and supportive measures aimed at correcting clinical symptoms and preventing possible complications.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Pharmasintez JSC, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 ° C. Keep out of reach of children. |
| Manufacturer | Pharmasintez JSC, Russia |
| Medication form | pills |
| Brand | Pharmasintez JSC |
Related products
Buy Capecitabine 150 mg 60 pcs. with delivery to USA, UK, Europe and over 120 other countries.