No products in the cart.
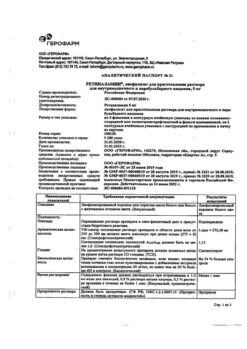
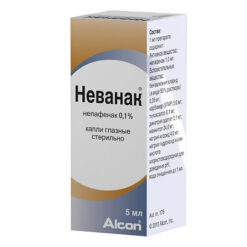
Brinzopt, eye drops 10 mg/ml 5 ml
€25.50 €21.25
Description
Increased intraocular pressure, Glaucoma
Brinzopt is used as monotherapy in adult patients who do not respond to beta-adrenoblockers or in adult patients for whom beta-adrenoblockers are contraindicated, or as adjunctive therapy to beta-adrenoblockers or prostaglandin analogues to reduce increased intraocular pressure in
– intraocular hypertension;
– open-angle glaucoma.
Indications
Indications
Brinzopt is used as monotherapy in adult patients who do not respond to beta-blockers, or in adult patients for whom beta-blockers are contraindicated, or as adjunctive therapy to beta-blockers or prostaglandin analogues to reduce elevated intraocular pressure in:
— intraocular hypertension;
– open-angle glaucoma.
Pharmacological effect
Pharmacological effect
Antiglaucoma drug – local carbonic anhydrase inhibitor
Special instructions
Special instructions
Systemic effects
Brinzolamide is a sulfonamide carbonic anhydrase inhibitor and, despite topical administration, is absorbed systemically. When applied topically, undesirable side reactions characteristic of sulfonamides may occur. If serious adverse reactions occur or signs of hypersensitivity occur, discontinue use of the drug.
Cases of acid-base imbalance have been reported with oral administration of carbonic anhydrase inhibitors. Brinzolamide has not been studied in premature neonates (less than 36 weeks’ gestation) or in infants less than 1 week of age. In patients with significant underdevelopment or dysfunction of the renal tubules, brinzolamide should be used only after a careful assessment of the risk/benefit ratio, because there is a risk of developing metabolic acidosis.
Oral carbonic anhydrase inhibitors may impair the ability of elderly patients to perform activities requiring alertness and/or physical coordination. Brinzolamide is absorbed systemically, so this effect may also occur with topical application.
Combination therapy
When used in patients receiving oral carbonic anhydrase inhibitor therapy and brinzolamide, there is a risk of additive effects of carbonic anhydrase inhibition. Concomitant use of brinzolamide and oral carbonic anhydrase inhibitors has not been studied and such use is not recommended.
The effect of brinzolamide was mainly analyzed when used concomitantly with timolol as an adjunctive therapy in the treatment of glaucoma. The intraocular pressure (IOP)-lowering effect of brinzolamide was also examined when brinzolamide was used as an add-on therapy to the prostaglandin analogue travoprost. There are no data on long-term use of brinzolamide as concomitant therapy to travoprost.
There are limited data on the use of brinzolamide in the treatment of patients with pseudoexfoliation glaucoma or pigmentary glaucoma. When treating such patients, care should be taken and IOP levels should be constantly monitored. Brinzolamide has not been studied in patients with angle-closure glaucoma and is therefore not recommended for use in these patients.
Studies of the possible effects of brinzolamide on corneal endothelial function in patients with impaired corneal function (particularly in patients with low endothelial cell counts) have not been conducted.
There have been no studies of the drug in patients who wear contact lenses, so close monitoring of such patients is recommended when using brinzolamide, as carbonic anhydrase inhibitors may affect corneal hydration and the use of contact lenses may increase the risk of corneal exposure. Careful observation is recommended in other similar cases associated with impaired corneal function, for example, in patients with diabetes mellitus.
There is evidence that benzalkonium chloride, which is commonly used as a preservative in ophthalmic preparations, may cause the development of punctate keratopathy and/or toxic ulcerative keratopathy. Since the drug contains benzalkonium chloride, careful monitoring is necessary during frequent or prolonged treatment with the drug in patients with dry eyes or corneal damage.
The effect of brinzolamide in patients wearing contact lenses has not been studied. This product contains benzalkonium chloride, which may cause irritation to the mucous membrane of the eye and has been reported to discolor soft contact lenses. Contact of the drug with soft contact lenses should be avoided. Patients should be warned that before using the drug it is necessary to remove contact lenses and install them no earlier than 15 minutes after instillation of the drug.
Possible adverse effects following discontinuation of brinzolamide treatment have not been studied; The expected period of effect of lowering intraocular pressure is 5-7 days.
Active ingredient
Active ingredient
Brinzolamide
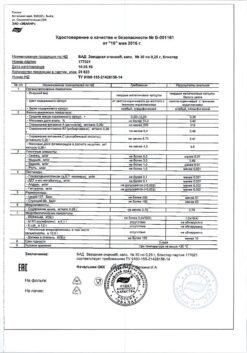
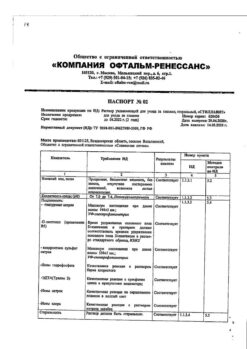
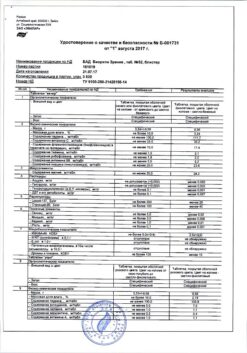
Composition
Composition
1 ml brinzolamide 10 mg
Excipients:
tyloxapol, carbomer 974P,
mannitol,
sodium chloride,
disodium edetate dihydrate,
benzalkonium chloride,
1M hydrochloric acid solution or 1M sodium hydroxide solution,
purified water.
Contraindications
Contraindications
– severe renal failure;
— hyperchloremic acidosis;
– hypersensitivity to the active substance or to any of the auxiliary components;
– hypersensitivity to sulfonamides.
Side Effects
Side Effects
In clinical studies involving more than 1800 patients receiving brinzolamide as monotherapy or in combination with timolol maleate 5 mg/mL, the most frequently occurring treatment-related adverse reactions were dysgeusia (5.8%) (bitter or unusual taste in the mouth after instillation) and temporary blurred vision (5.8%) lasting from a few seconds to a few minutes.
The frequency of adverse reactions was determined as follows: very common (≥1/10), common (≥1/100 and <1/10), uncommon (≥1/1000 and <1/100), rare (≥1/10,000 and <1/1000), very rare (<1/10,000), frequency unknown (cannot be determined based on available data). Adverse reactions in each group are presented by frequency and in descending order of severity/danger.Infectious and parasitic diseases: infrequently – nasopharyngitis, pharyngitis, sinusitis; frequency unknown – rhinitis.
From the hematopoietic system: infrequently – anemia.
From the immune system: frequency unknown – hypersensitivity reactions.
Mental disorders: uncommon – apathy, depression, depressed mood, decreased libido, nightmares, insomnia, nervousness.
From the nervous system: often – dysgeusia, headache; uncommon – drowsiness, motor dysfunction, amnesia, memory impairment, dizziness, paresthesia; frequency unknown – tremor, hypoesthesia, ageusia.
On the part of the organ of vision: often – blepharitis, blurred vision, eye irritation, eye pain, dry eyes, discharge from the eyes, itching of the eyes, sensation of a foreign body in the eyes, hyperemia; uncommon – corneal erosions, keratitis, punctate keratitis, keratopathy, corneal deposits, corneal staining, corneal epithelial defects, increased intraocular pressure, increased cup/disc ratio at the level of the optic nerve, corneal edema, conjunctivitis, ocular edema, inflammation of the meibomian glands, diplopia, glare, photophobia, photopsia, decreased visual acuity, allergic conjunctivitis, pterygium, scleral pigmentation, asthenopia, discomfort in the eyes, unusual sensations in the eye, dry keratoconjunctivitis, eye hypoesthesia, subconjunctival cysts, conjunctival hyperemia, itching of the eyelids, crusts on the edges of the eyelids, swelling of the eyelids, increased lacrimation; frequency unknown – visual impairment, eye inflammation, allergic manifestations, madarosis, erythema of the eyelids.
From the organ of hearing and vestibular apparatus: infrequently – ringing in the ears; frequency unknown – dizziness.
From the cardiovascular system: infrequently – cardiorespiratory distress syndrome, angina pectoris, bradycardia, palpitations, cardiac arrhythmia; frequency unknown – arrhythmia, tachycardia, hypertension, increased blood pressure, increased heart rate.
From the respiratory system: infrequently – shortness of breath, bronchial hyperreactivity, cough, nosebleeds, pharyngolaryngeal pain, irritation in the throat, nasal congestion, upper respiratory tract congestion, postnasal drip, runny nose, sneezing, dry nose; frequency unknown – bronchial asthma.
From the digestive system: often – xerostomia; uncommon – esophagitis, diarrhea, nausea, dyspepsia, upper abdominal pain, abdominal discomfort, stomach discomfort, flatulence, frequent bowel movements, gastrointestinal disorders, oral hypoesthesia, oral paresthesia.
From the skin and subcutaneous tissue: uncommon – urticaria, rash, maculopapular skin rash, generalized itching, hair loss, feeling of skin tightness; frequency unknown – dermatitis, erythema.
From the musculoskeletal system: infrequently – back pain, muscle spasms, myalgia; frequency unknown – arthralgia, pain in the extremities.
From the urinary system: infrequently – renal colic; frequency unknown – pollakiuria.
From the reproductive system: infrequently – erectile dysfunction.
Laboratory data: infrequently – hyperchloremia; frequency unknown – abnormal results of liver function tests.
General and local reactions: infrequently – pain, discomfort in the chest, asthenia, fatigue, feeling of malaise, anxiety, irritability; frequency unknown – chest pain, peripheral edema, malaise, foreign body sensation in the eye.
In short-term clinical trials, side effects were observed in approximately 12.5% of pediatric patients; most of them were local in nature and represented non-serious reactions from the organs of vision, such as conjunctival hyperemia, irritation of the mucous membrane of the eyes, discharge from the eyes and increased lacrimation.
Dysgeusia (bitter or unusual taste in the mouth after instillation) is the most common systemic side effect associated with brinzolamide observed in clinical studies. Most likely this is due to eye drops entering the nasopharynx through the nasolacrimal duct. After instillation, pressing the inner corner of the eye with a finger to close the nasolacrimal duct or gently closing the eyelids may help reduce the incidence of this effect.
Brinzolamide is a sulfonamide carbonic anhydrase inhibitor and is absorbed systemically. The use of systemic carbonic anhydrase inhibitors is usually associated with the occurrence of undesirable effects from the gastrointestinal tract, nervous system, hematopoietic system, kidneys and phenomena related to metabolism. When applied topically, the same type of adverse events may occur as with oral use of carbonic anhydrase inhibitors.
No unexpected adverse events were reported when brinzolamide was used in combination therapy with travoprost. Adverse events reported during combination therapy are also observed when each drug is used in monotherapy.
Interaction
Interaction
Specific studies of the interaction of brinzolamide with other drugs have not been conducted.
In clinical studies, brinzolamide was used in combination with prostaglandin analogues and timolol-based ophthalmic drugs; There were no cases of unwanted interactions. The interaction between brinzolamide and miotics or adrenergic receptor agonists has not been analyzed in combination therapy for glaucoma.
Brinzolamide is a carbonic anhydrase inhibitor and, despite topical administration, is absorbed systemically. Cases of acid-base imbalance have been reported with the use of oral carbonic anhydrase inhibitors. The potential for this interaction should be considered in patients receiving brinzolamide.
Cytochrome P450 isoenzymes that are responsible for the metabolism of brinzolamide include CYP3A4 (major), CYP2A6, CYP2C8 and CYP2C9. CYP3A4 inhibitors such as ketoconazole, itraconazole, clotrimazole, ritonavir and troleandomycin can be expected to inhibit the CYP3A4 metabolism of brinzolamide.
Caution should be exercised when coadministering CYP3A4 inhibitors. However, accumulation of brinzolamide is unlikely because it is excreted primarily through the kidneys. Brinzolamide is not an inhibitor of cytochrome P450 isoenzymes.
Overdose
Overdose
No cases of overdose have been reported.
Symptoms: Electrolyte imbalance, acidosis and adverse effects from the nervous system may develop.
Treatment: symptomatic and supportive therapy. It is recommended to monitor plasma electrolyte levels (especially potassium) and blood pH levels.
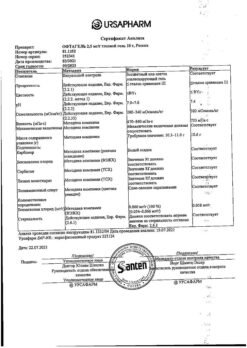
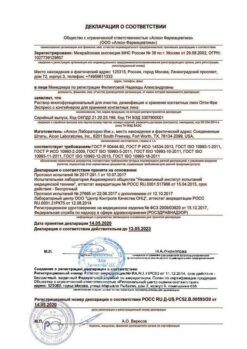
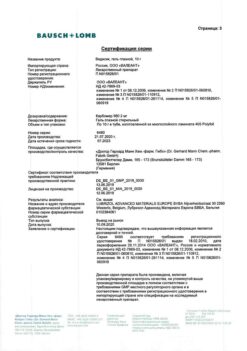
Manufacturer
Manufacturer
K.O.Rompharm Company S.R.L., Romania
Additional information
| Manufacturer | C.O.Rompharm Company S.R.L., Romania |
|---|---|
| Medication form | eye drops |
| Brand | C.O.Rompharm Company S.R.L. |
Related products
Buy Brinzopt, eye drops 10 mg/ml 5 ml with delivery to USA, UK, Europe and over 120 other countries.