No products in the cart.
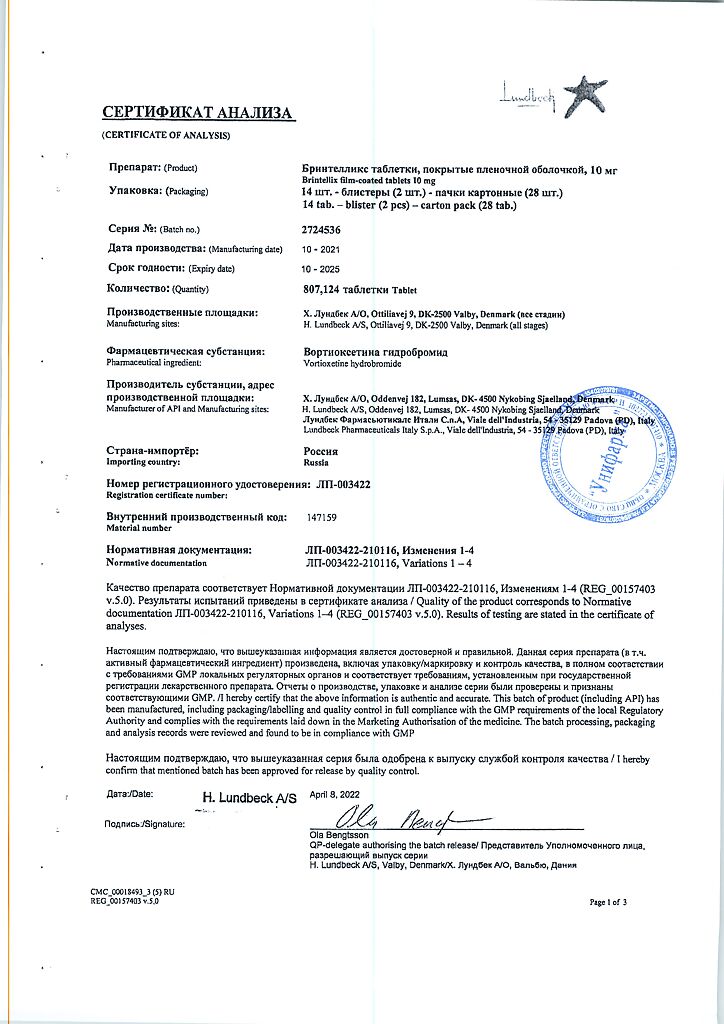
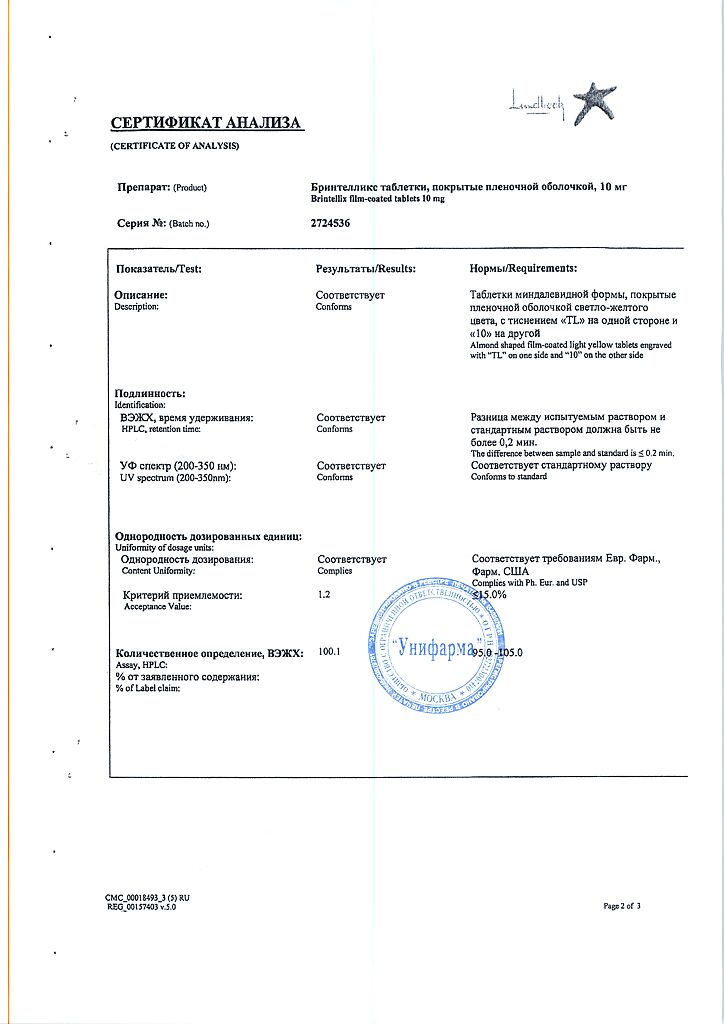
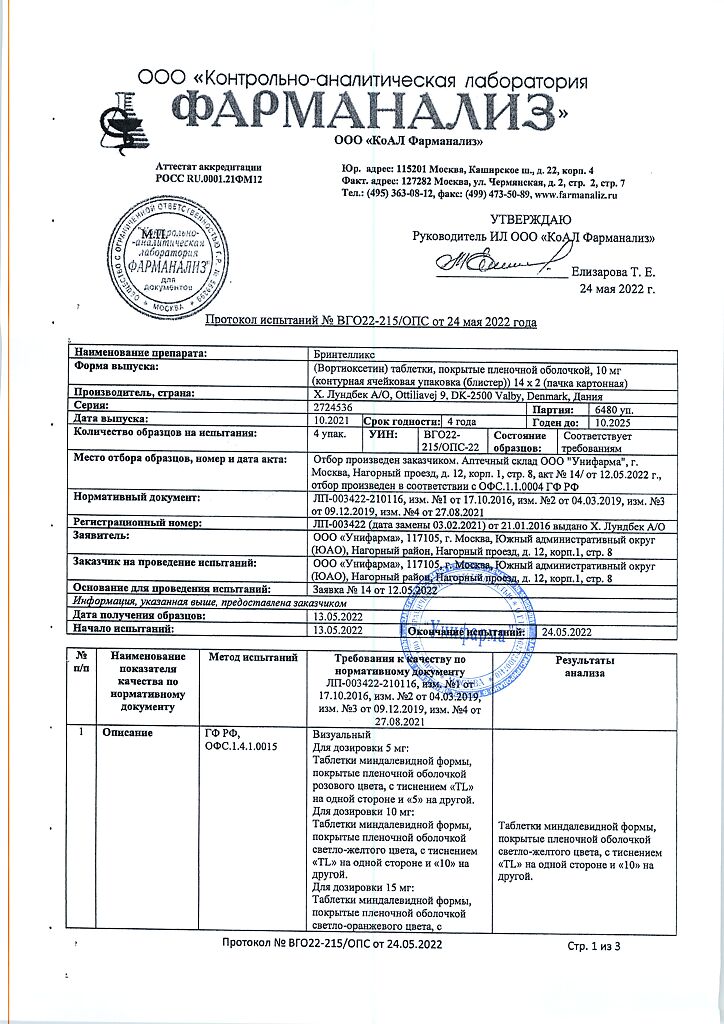
Brintellix, 10 mg 28 pcs.
€73.69 €61.41
Description
Pharmacodynamics
Mechanism of Action
The mechanism of action of vortioxetine is thought to be related to its multimodal activity, which is a combination of two pharmacological mechanisms: direct modulation of receptor activity and inhibition of the serotonin transporter (5-NT).
. Preclinical data show that vortioxetine is a 5-HT 3, 5-HT 7 and 5-HT 1D receptor antagonist, partial 5-HT 1B receptor agonist, 5-HT 1A receptor agonist and 5-HT transporter inhibitor, causing modulation of neurotransmission in several systems, including serotonin, noradrenaline, dopamine, histamine, acetylcholine, GABA and glutamate.
This multimodal activity is thought to provide antidepressant and anxiolytic effects as well as improved cognitive function, learning and memory in preclinical studies of vortioxetine. In addition, preclinical studies indicate that vortioxetine does not cause sexual dysfunction.
The exact contribution of each component of this mechanism to the observed pharmacodynamic profile remains unclear, so attention should be applied when extrapolating preclinical data directly to humans.
The serotonin transporter uptake by different daily doses of vortioxetine was found to be approximately 50% at the 5 mg dose, 65% at the 10 mg dose, and over 80% at the 20 mg dose. Vortioxetine clinically showed an antidepressant effect with a 50% capture of the 5-HT transporter.
Clinical efficacy and safety.
The efficacy of vortioxetine increases with increasing dose. In addition, vortioxetine in the 5-20 mg dose range has demonstrated efficacy in a wide range of depressive (on the MADRS scale) and anxiety (on the HAM-A scale) symptoms of depression.
Prevention of relapse.
The duration of the antidepressant effect was demonstrated in a relapse prevention study in which twice the risk of relapse was determined in the placebo group than in the vortioxetine group.
Elderly patients.
In the vortioxetine dose range of 5 to 20 mg per day, efficacy and tolerability in the elderly were consistent with results of studies in adults.
Patients with severe depression or high levels of anxiety symptoms.
Antidepressant efficacy has also been demonstrated in patients with severe depression (≥30 MADRS score) and in depressed patients with high levels of anxiety symptoms (≥20 HAM-A score) in short-term studies, including studies in elderly patients, and long-term relapse prevention studies.
Patients with inadequate response to SSRI/SRI treatment.
In a flexible dose comparison study in depressed patients after an inadequate treatment response to an existing SSRI/SIZZN episode, vortioxetine at a daily dose of 10-20 mg was statistically significantly more effective than agomelatine at 25-50 mg (MADRS scale), clinical significance was proven by the CGI-I and SDS scales.
Cognitive dysfunction in depression.
In studies of the drug’s effects on cognitive processes, it appears that the effects of vortioxetine are mainly due to direct effects on cognitive function rather than indirect effects through improvement of depression symptoms.
Quality of life and overall functioning.
Vortioxetine was superior to placebo on measures of quality of life and clinically significantly improved general health (on the EQ-5D scale) and measures of general functioning (on the SDS scale – work, social and family life) compared with placebo or the active comparison agent (agomelatine) . Moreover, the better effects compared to placebo on quality of life persisted over the long-term relapse prevention study.
Tolerability and safety.
The safety and tolerability of vortioxetine have been evaluated in short- and long-term studies for doses of 5-20 mg daily.
Vortioxetine did NOT increase the incidence of insomnia or drowsiness compared with placebo.
In a systematic evaluation of potential withdrawal symptoms, there was no clinically significant difference between vortioxetine and placebo in the frequency and nature of withdrawal symptoms after either a short-term (6-12 weeks) or long-term (24-64 weeks) treatment period.
In clinical trials with vortioxetine, the frequency of reported adverse sexual reactions was low and similar to placebo, the rates of therapy-related sexual dysfunction and overall ASEX scores had no clinically significant differences with placebo for sexual dysfunction symptoms at the recommended dose of vortioxetine, but high doses were associated with numerical increases in dysfunction.
In clinical trials similar to placebo, vortioxetine had no effect on body weight, heart rate or blood pressure.
There were no clinically significant changes in liver or kidney function scores in clinical studies.
Vortioxetine had no clinically significant effect on ECG parameters, including QT-, QTc-, PR-, and QRS-intervals, in patients with major depressive disorder. In a careful study of QTc among healthy volunteers, no potential for increased QTc interval was observed with doses up to 40 mg per day.
Childhood.
The clinical studies in pediatric patients have not been conducted, therefore, the safety and efficacy of the drug. Brintellix for patients under the age of 18 years have not been established.
Pharmacokinetics
Absorption
Vortioxetine is slowly but well absorbed after oral administration and peak plasma concentrations are reached within 7-11 hours. An average C Max of 9-33 ng/ml has been observed after multiple doses of 5, 10, or 20 mg per day. The bioavailability is 75%. No effect of food intake on pharmacokinetics was observed.
Distribution
The mean volume of distribution (V SS) is 2600 L, indicating volumetric extravascular distribution. Vortioxetine binds strongly to plasma proteins (98-99%) and binding appears to be independent of plasma vortioxetine concentration.
Metabolism
Vortioxetine is extensively metabolized in the liver, primarily by oxidation and subsequent conjugation by glucuronic acid.
In vitro the cytochrome P450 isoenzymes CYP2D6, CYP3A4/5, CYP2C19, CYP2C9, CYP2A6, CYP2C8 and CYP2B6 are involved in the metabolism of vortioxetine. No inhibitory or inducing effects of vortioxetine in vitro on the CYP CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1 or CYP3A4 / 5 isoenzymes were observed. Vortioxetine is a weak P-gp substrate and inhibitor.
The main metabolite of vortioxetine is pharmacologically inactive.
Elimation
The elimination half-life is 66 hours. Approximately 2/3 of the inactive vortioxetine metabolite is excreted in the urine and about 1/3 in the feces. Only a small amount of vortioxetine is excreted in the feces. Stable concentrations in blood plasma are reached after 2 weeks.
Linearity/nonlinearity
The pharmacokinetics are linear and time-independent over the range of doses studied (2.5-60 mg daily). According to the half-life, the accumulation index is 5 to 6 based on an AUC of 0-24 after multiple doses of 5 to 20 mg per day.
Elderly Patients
In elderly healthy volunteers (aged ≥65 years, n = 20), vortioxetine effects were increased by 27% (C max and AUC) compared with young healthy control volunteers (aged ≤45 years) after several doses of 10 mg daily. No dose adjustment is required.
Renal Impairment
After a single dose of 10 mg vortioxetine, renal impairment (Cockroft-Gault formula, mild, moderate or severe, n = 8 per group) caused a slight increase in exposure (up to 30%) compared with that in control healthy volunteers. In patients with end-stage renal failure, only a small fraction of vortioxetine was lost during the dialysis process (AUC and C Max 13% and 27% lower; n = 8) after a single dose of 10 mg vortioxetine. No dose adjustment was required.
Hepatic Impairment
After a single dose of 10 mg vortioxetine, the effects of mild to moderate hepatic impairment (Child-Pugh, criteria A and B; n=8 in each group) on the pharmacokinetics of vortioxetine was not observed (AUC changes were less than 10%). No dose adjustment was required. Vortioxetine has not been studied in patients with severe hepatic impairment, and caution should be exercised when prescribing in these patients.
Weak CYP2D6 metabolizers
In weak CYP2D6 metabolizers, vortioxetine had about twice the plasma concentration of extensive metabolizers. In the presence of potent CYP3A4/2C9 inhibitors, the effect could potentially be higher.
Dose adjustment may be required, as in all patients, depending on individual response.
Indications
Indications
Treatment of major depressive disorder in adults.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Mechanism of action
The mechanism of action of vortioxetine is believed to be related to its multimodal activity, which is a combination of two pharmacological mechanisms: direct modulation of receptor activity and inhibition of the serotonin transporter (5-HT).
Preclinical data indicate that vortioxetine is a 5-HT 3, 5-HT 7 and 5-HT 1D receptor antagonist, a partial 5-HT 1B receptor agonist, a 5-HT 1A receptor agonist and a 5-HT transporter inhibitor, causing modulation of neurotransmission in several systems, including serotonin, norepinephrine, dopamine, histamine, acetylcholine, GABA and glutamate.
This multimodal activity is believed to provide antidepressant and anxiolytic effects, as well as improvements in cognitive function, learning and memory in preclinical studies of vortioxetine. In addition, preclinical studies indicate that vortioxetine does not cause sexual dysfunction.
The precise contribution of each component of this mechanism to the observed pharmacodynamic profile remains unclear, and caution must be exercised when extrapolating preclinical data directly to humans.
It was found that the uptake of the serotonin transporter by various daily doses of vortioxetine was approximately 50% with a dose of 5 mg, 65% with a dose of 10 mg, and more than 80% with a dose of 20 mg. Vortioxetine has been clinically shown to have antidepressant effects at 50% 5-HT transporter uptake.
Clinical efficacy and safety.
The effectiveness of vortioxetine increases with increasing dose. In addition, vortioxetine in doses of 5-20 mg has demonstrated effectiveness in a wide range of depressive (MADRS scale) and anxious (HAM-A scale) depressive symptoms.
Relapse prevention.
The duration of the antidepressant effect was demonstrated in a relapse prevention study, in which a twice as high risk of relapse was found in the placebo group than in the vortioxetine group.
Elderly patients.
In the dose range of vortioxetine from 5 to 20 mg per day, efficacy and tolerability in older adults corresponded to the results of studies in the adult population.
Patients with severe depression or high levels of anxiety symptoms.
Antidepressant efficacy has also been demonstrated in patients with severe depression (MADRS score ≥ 30) and in depressed patients with high levels of anxiety symptoms (HAM-A score ≥ 20) in short-term studies, including studies in elderly patients, and long-term relapse prevention studies.
Patients with an inadequate response to SSRI/SNRI treatment.
In a comparative study of flexible dosing in patients with depression after an inadequate response to treatment of an existing episode of SSRI/SNRI, vortioxetine at a daily dose of 10-20 mg was statistically significantly more effective than agomelatine at a dose of 25-50 mg (MADRS scale), clinical significance was demonstrated on the CGI-I and SDS scales.
Cognitive dysfunction in depression.
In studies of the drug’s effect on cognition, the effect of vortioxetine was found to be primarily due to direct effects on cognitive function rather than indirect effects through improvement of depressive symptoms.
Quality of life and general functioning.
Vortioxetine was superior to placebo on measures of quality of life and clinically significantly improved global health (EQ-5D) and global functioning (SDS – work, social and family life) compared with placebo or the active comparator (agomelatine). Moreover, the superior effects compared with placebo on quality of life were maintained throughout the long-term relapse prevention study.
Tolerability and safety.
The safety and tolerability of vortioxetine were assessed in short- and long-term studies at doses of 5-20 mg per day.
Vortioxetine did NOT increase the frequency of insomnia or somnolence compared to placebo.
In a systematic assessment of potential withdrawal symptoms, there was no clinically significant difference between vortioxetine and placebo in the frequency or nature of withdrawal symptoms after either short-term (6-12 weeks) or long-term (24-64 weeks) treatment periods.
In clinical trials of vortioxetine, the incidence of reported sexual adverse reactions was low and similar to placebo, rates of treatment-related sexual dysfunction and ASEX total scores were not clinically significant different from placebo for symptoms of sexual dysfunction at the recommended dose of vortioxetine, but high doses were associated with an increased incidence of dysfunction.
In clinical trials, vortioxetine had no effect on body weight, heart rate, or blood pressure, similar to placebo.
There were no clinically significant changes in liver and kidney function scores during the clinical studies.
Vortioxetine did not have any clinically significant effect on ECG parameters, including QT, QTc, PR and QRS intervals, in patients with major depressive disorder. In a rigorous QTc study in healthy volunteers, no potential for QTc prolongation was observed at doses up to 40 mg per day.
Childhood.
Clinical studies have not been conducted among pediatric patients, hence the safety and effectiveness of the drug. Brintellix has not been established for use in patients under 18 years of age.
Pharmacokinetics
Absorption
Vortioxetine is slowly but well absorbed after oral administration and peak plasma concentrations are reached within 7-11 hours. After repeated dosing of 5, 10 or 20 mg per day, an average Cmax of 9-33 ng/ml was observed. Bioavailability is 75%. No effect of food intake on pharmacokinetics was observed.
Distribution
The mean volume of distribution (V SS) is 2600 L, indicating voluminous extravascular distribution. Vortioxetine is highly bound to plasma proteins (98-99%) and binding appears to be independent of plasma concentrations of vortioxetine.
Metabolism
Vortioxetine is extensively metabolized in the liver, mainly through oxidation and subsequent conjugation with glucuronic acid.
In vitro, cytochrome P450 isoenzymes CYP2D6, CYP3A4/5, CYP2C19, CYP2C9, CYP2A6, CYP2C8 and CYP2B6 are involved in the metabolism of vortioxetine. No inhibitory or inducing effects of vortioxetine in vitro on the CYP isoenzymes CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1 or CYP3A4/5 were observed. Vortioxetine is a weak P-gp substrate and inhibitor.
The main metabolite of vortioxetine is pharmacologically inactive.
Removal
The half-life is 66 hours. Approximately 2/3 of the inactive metabolite vortioxetine is excreted in the urine and about 1/3 in the feces. Only a small amount of vortioxetine is excreted in the feces. Steady-state plasma concentrations are achieved after 2 weeks.
Linearity/nonlinearity
Pharmacokinetics are linear and independent of time in the dose range studied (2.5-60 mg per day). According to the half-life, the accumulation index is 5 to 6 based on AUC 0-24 after multiple doses of 5 to 20 mg per day.
Elderly patients
In older healthy volunteers (age ≥ 65 years, n = 20), exposure to vortioxetine was increased by 27% (Cmax and AUC) compared to young healthy control volunteers (age ≤ 45 years) after multiple doses of 10 mg daily. No dose adjustment is required.
Kidney failure
After a single dose of 10 mg vortioxetine, renal impairment (Cockcroft-Gault formula, mild, moderate or severe, n = 8 per group) caused a slight increase in exposure (up to 30%) compared with that in a control group of healthy volunteers. In patients with end-stage renal disease, only a small fraction of vortioxetine was lost during the dialysis process (AUC and Cmax 13% and 27% lower; n = 8) after a single dose of 10 mg vortioxetine. No dose adjustment is required.
Liver failure
After a single 10 mg dose of vortioxetine, there was no effect of mild to moderate hepatic impairment (Child-Pugh criteria A and B; n=8 in each group) on the pharmacokinetics of vortioxetine (changes in AUC were less than 10%). No dose adjustment is required. Vortioxetine has not been studied in patients with severe hepatic impairment and caution should be exercised when prescribing to these patients.
Poor metabolizers of CYP2D6
In poor CYP2D6 metabolizers, plasma concentrations of vortioxetine were approximately twice as high as in extensive metabolizers. In the presence of potent CYP3A4/2C9 inhibitors, the effect could potentially be greater.
Dose adjustment may be necessary, as in all patients, depending on individual response.
Active ingredient
Active ingredient
Vortioxetine
Contraindications
Contraindications
Hypersensitivity to the active substance or any component of the drug.
Concomitant use with non-selective MAO inhibitors (MAO) or selective MAO-A inhibitors.
Side Effects
Side Effects
The most common adverse reaction was nausea. Adverse reactions were usually mild or moderate and were observed during the first two weeks of treatment. Reactions were generally transient and did not usually lead to discontinuation of therapy. From the digestive system (eg nausea) were more often observed in women than in men.
The adverse reactions listed below are defined as:
very often (≥ 1/10),
often (≥ 1/100 to < 1/10),
uncommon (≥ 1/1000 to < 1/100),
rare (≥ 1/10,000 to < 1/1000),
very rare (< 1/10,000)
unknown (frequency cannot be determined from available data).
From the side of nutrition and metabolism:
Common: Decreased appetite
From the mental side:
Common: Pathological dreams
Uncommon: Bruxism
From the nervous system:
Common: Dizziness
From the cardiovascular system:
Uncommon: Blush
From the digestive system:
Very common: Nausea
Common: Diarrhea, constipation, vomiting
From the skin and subcutaneous tissue:
Common: Generalized itching
Uncommon: Night sweats
Interaction
Interaction
Vortioxetine is metabolized in the liver mainly by oxidation and subsequent conjugation with glucuronic acid. In vitro, the cytochrome P450 isoenzymes CYP2D6, CYP3A4/5, CYP2C19, CYP2C9, CYP2A6, CYP2C8 and CYP2B6 are involved in the metabolism of vortioxetine.
The influence of other drugs on the action of vortioxetine. Irreversible non-selective MAO inhibitors
Due to the risk of serotonin syndrome, vortioxetine is contraindicated in any combination with irreversible non-selective MAO inhibitors. Treatment with vortioxetine should not be started until at least 14 days after stopping treatment with irreversible non-selective MAO inhibitors. Vortioxetine should be discontinued at least 14 days before starting treatment with irreversible non-selective MAO inhibitors.
Revolving selective MAO-A inhibitor (moclobemide). The combination of vortioxetine with a reversible selective MAO-A inhibitor such as moclobemide is contraindicated. Careful monitoring for serotonin syndrome is necessary during concurrent use.
Reversible non-selective MAO inhibitor (linezolid). The combination of vortioxetine with a weak, reversible and non-selective MAO inhibitor, such as the antibiotic linezolid, is contraindicated. Careful monitoring for serotonin syndrome is necessary during concurrent use.
Non-circulating selective MAO-B inhibitors (selegiline, rasagiline). Despite the lower expected risk of serotonin syndrome (than with MAO-A inhibitors), the combination of vortioxetine with irreversible MAO-B inhibitors such as selegiline or rasagiline should be used with caution. Careful monitoring for serotonin syndrome is necessary during concurrent use.
Serotonergic drugs.
Concomitant administration with serotonergic drugs (for example, tramadol, sumatriptan and other triptans) can lead to serotonin syndrome.
St. John’s wort.
Concomitant use of serotonergic antidepressants and herbal remedies containing St. John’s wort may lead to an increased incidence of adverse reactions, including serotonin syndrome.
Medicines that lower the seizure threshold.
Serotonergic antidepressants may lower the seizure threshold. Caution is recommended during the simultaneous use of other drugs that can lower the seizure threshold (such as antidepressants (TCAs, SSRIs, SNRIs), antipsychotics (phenothiazines, thioxanthenes, butyrophenones), mefloquine, bupropion and tramadol).
ECT (electroconvulsive therapy).
There is no clinical experience with the concomitant use of vortioxetine with ECT, so caution is advisable.
Cytochrome P450 inhibitors.
When administered together with 150 mg bupropion (a strong CYP2D6 inhibitor) twice daily for 14 days in healthy volunteers, the exposure to vortioxetine was increased by 2.3-fold for AUC. Coadministration was more likely to result in an increased incidence of adverse events when bupropion was added to vortioxetine than when vortioxetine was added to bupropion. Depending on the patient’s individual sensitivity, low-dose vortioxetine may be considered when adding strong CYP2D6 inhibitors (e.g., bupropion, quinidine, fluoxetine, paroxetine) to therapy.
When co-administered with vortioxetine after 6 days of ketoconazole 400 mg per day (inhibitor of CYP3A4/5 and P-glycoprotein) or fluconazole 200 mg per day (inhibitor of CYP2C9, CYP2C19 and CYP3A4/5), a 1.3-fold and 1.5-fold increase in the AUC of vortioxetine was observed in healthy volunteers, respectively. No dose adjustment is required.
The effect of a single 40 mg dose of omeprazole (CYP2C19 inhibitor) on the pharmacokinetics of long-term use of vortioxetine in healthy volunteers was not observed.
The combination of strong CYP3A4 and CYP2C9 inhibitors has not been studied in patients who are poor CYP2D6 metabolizers, but increased exposure to vortioxetine in such patients is likely to be expected.
Inducers of cytochrome P450.
When a single dose of 20 mg vortioxetine was administered concomitantly after 10 days of rifampicin 600 mg daily (a CYP isoenzyme inducer), a 72% reduction in vortioxetine AUC was observed in healthy volunteers. Depending on the individual patient’s response, dose adjustment may be necessary if a cytochrome P450 inducer (eg rifampicin, carbamazepine, phenytoin) is added to vortioxetine treatment.
Acetylsalicylic acid.
The effect of repeated administration of acetylsalicylic acid 150 mg per day on the pharmacokinetics of vortioxetine in healthy volunteers was not observed.
Effect of vortioxetine on the action of other drugs. Anticoagulants and antiplatelet agents. There were no significant effects on plasma international normalized ratio, prothrombin, or R-/S-warfarin compared with placebo when vortioxetine was coadministered with a fixed dose of warfarin in healthy volunteers.
In addition, there was no significant inhibitory effect compared with placebo on platelet aggregation when coadministered with aspirin at a dose of 150 mg per day after taking vortioxetine in healthy volunteers. However, as with other serotonergic agents, caution should be exercised when vortioxetine is used in combination with oral anticoagulants or antiplatelet agents due to a potential increased risk of bleeding due to pharmacodynamic interactions.
Alcohol.
There was no effect on the pharmacokinetics of vortioxetine or ethanol, as well as significant impairment of cognitive function compared to placebo after administration of vortioxetine in doses of 20 mg or 40 mg with simultaneous single administration of ethanol 0.6 g/kg in healthy volunteers. However, like other drugs that act on the central nervous system, the use of vortioxetine in combination with alcohol is not recommended.
Cytochrome P450 substrates.
In vitro, vortioxetine did not show the potential to inhibit or induce cytochrome P450 isoenzymes. An inhibitory effect of vortioxetine on cytochrome P450 isoenzymes CYP2C19 (omeprazole, diazepam), CYP3A4/5 (ethinyl estradiol, midazolam), CYP2B6 (bupropion), CYP2C9 (tolbutamide, S-warfarin), CYP1A2 (caffeine) or CYP2D6 (dextromethorphan) was found in healthy volunteers.
There was no significant impairment of cognitive function compared with placebo after the use of vortioxetine concomitantly with 10 mg diazepam.
There was no significant effect on sex hormone levels compared to placebo following concomitant use of vortioxetine with a combined oral contraceptive (ethinyl estradiol 30 mcg/levonorgestrel 150 mcg).
Lithium, tryptophan.
There was no clinically significant effect of exposure to stable concentrations of lithium after concomitant use with vortioxetine in healthy volunteers. However, there have been reports of enhanced effects when serotonergic antidepressants are used together with lithium or tryptophan, so the simultaneous use of vortioxetine with these drugs should be used with caution.
Overdose
Overdose
Experience is limited. Taking vortioxetine in the dose range from 40 to 75 mg caused an exacerbation of the following side effects:
Nausea
Postural vertigo
Diarrhea
Abdominal discomfort
Generalized itching
Drowsiness and blush
Treatment should be symptomatic and include appropriate monitoring. Medical supervision in specialized settings is recommended.
Manufacturer
Manufacturer
H. Lundbeck A/O, Denmark
Additional information
| Manufacturer | Х. Lundbeck A/O, Denmark |
|---|---|
| Medication form | pills |
| Brand | Х. Lundbeck A/O |
Related products
Buy Brintellix, 10 mg 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.