No products in the cart.
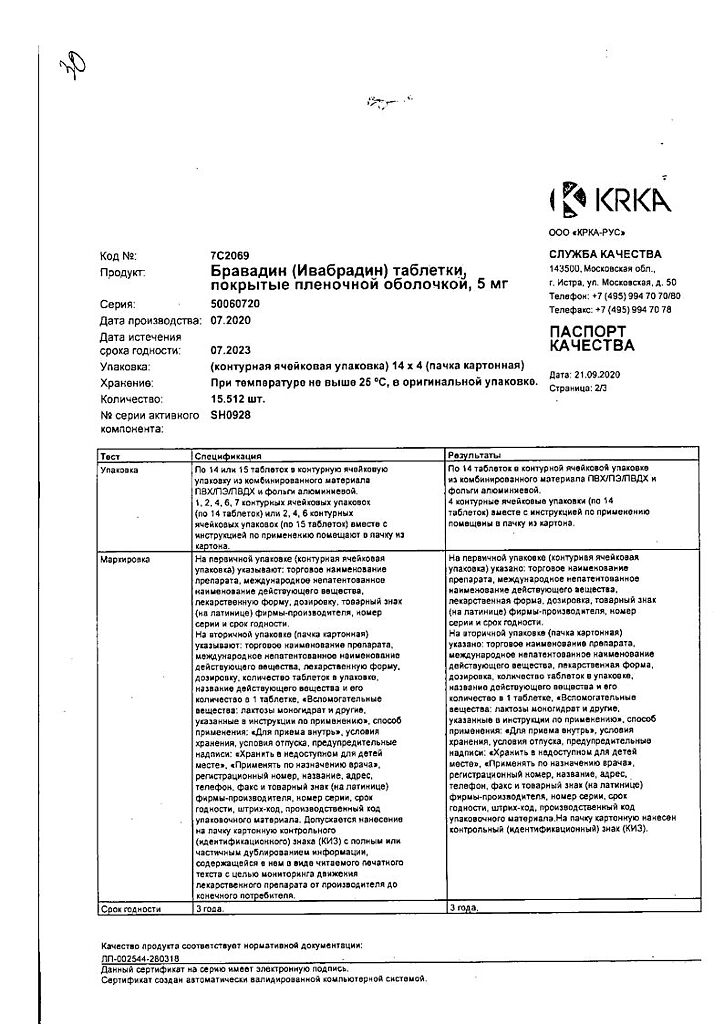
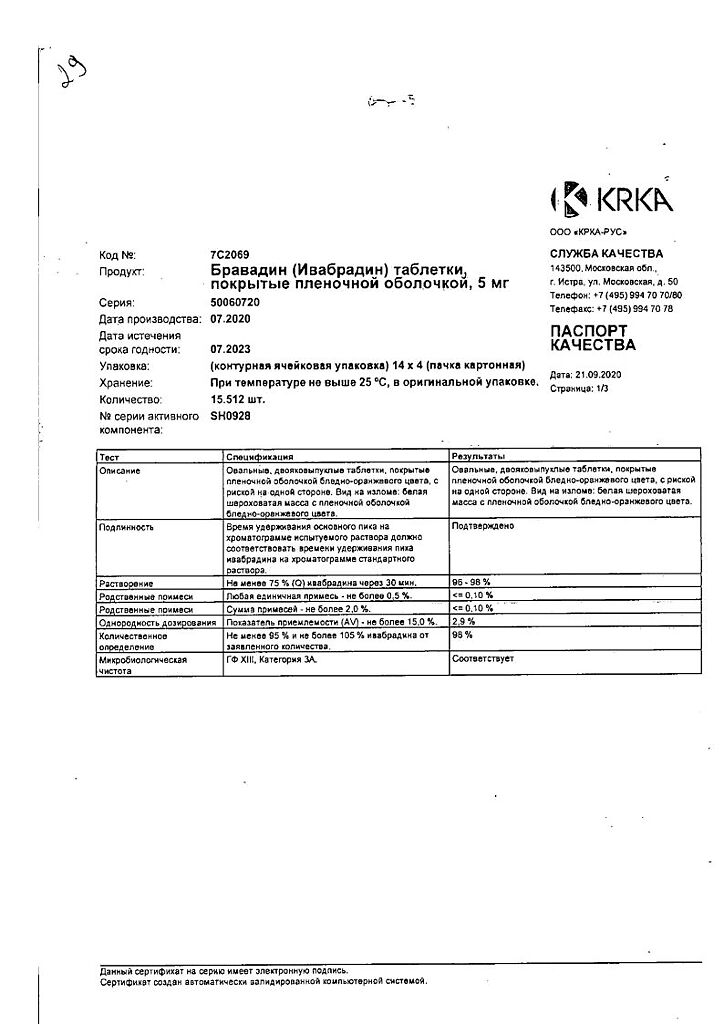
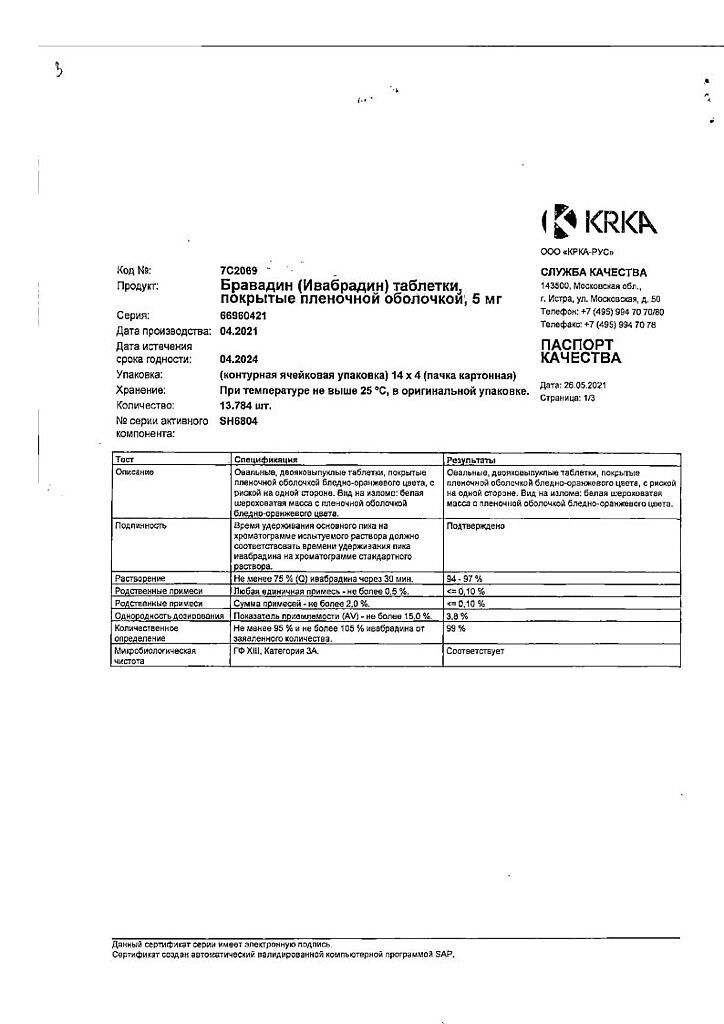
Bravadin, 5 mg 56 pcs.
€23.43 €19.52
Description
Heart failure, Arrhythmia, Angina
Symptomatic therapy of stable angina
Symptomatic therapy of stable angina in coronary heart disease (CHD) in adult patients with normal sinus rhythm and heart rate of at least 70 bpm:
– if intolerant or contraindicated to the use of beta-adrenoblockers;
– in combination with beta-adrenoblockers in inadequate control of stable angina against optimal dose of beta-adrenoblocker.
The therapy of chronic heart failure (CHF)
Therapy of CHF of functional class II-IV according to NYHA classification with systolic dysfunction in patients with sinus rhythm and HR of at least 70 bpm in combination with standard therapy, including therapy with beta-adrenoblockers, or with intolerance or contraindications to the use of beta-adrenoblockers.
Indications
Indications
Symptomatic treatment of stable angina
Symptomatic treatment of stable angina in coronary artery disease (CHD) in adult patients with normal sinus rhythm and heart rate of at least 70 beats/min:
· if you are intolerant or have contraindications to the use of beta-blockers;
· in combination with beta-blockers in case of inadequate control of stable angina pectoris against the background of the optimal dose of beta-blocker.
Therapy of chronic heart failure (CHF)
Treatment of CHF II-IV functional class according to the NYHA classification with systolic dysfunction in patients with sinus rhythm and heart rate of at least 70 beats/min in combination with standard therapy, including therapy with beta-blockers, or in case of intolerance or contraindications to the use of beta-blockers.
Pharmacological effect
Pharmacological effect
antianginal agent
Special instructions
Special instructions
Moderately severe liver failure (7-9 points on the Child-Pugh scale), severe renal failure (creatinine clearance less than 15 ml/min), congenital prolongation of the QT interval (see section “Interaction with other drugs”), simultaneous use of drugs that prolong the QT interval, simultaneous use of grapefruit juice, recent stroke, pigmentary degeneration of the retina. (retinitispigmentosa), arterial hypotension, CHF functional class IV according to the NYHA classification, simultaneous use with potassium-sparing diuretics (see section “Interaction with other drugs”).
Contraindicated for persons under 18 years of age (the effectiveness and safety of the drug in this age group have not been established).
Use in patients over 75 years of age
For patients aged 75 years and older, the recommended starting dose of Bravadin is 2.5 mg (1/2 tablet 5 mg) 2 times a day. In the future, it is possible to increase the dose of Bravadin.
Renal dysfunction
For patients with CC more than 15 ml/min, the recommended initial dose of Bravadin is 10 mg per day (1 tablet of 5 mg 2 times a day) (see section “Pharmacokinetics”). Depending on the therapeutic effect, after 3-4 weeks of use, the dose of Bravadin can be increased to 15 mg (1 tablet of 7.5 mg 2 times a day).
Due to the lack of clinical data on the use of Bravadin in patients with CC less than 15 ml/min, the drug should be used with caution.
Liver dysfunction
In patients with mild liver failure (less than 7 points on the Child-Pugh scale), the usual dosage regimen is recommended.
Caution should be exercised when using Bravadin in patients with moderate liver failure (7-9 points on the Child-Pugh scale).
The drug Bravadin is contraindicated in patients with severe liver failure (more than 9 points on the Child-Pugh scale), since the use of the drug Bravadin in such patients has not been studied (a significant increase in the concentration of the drug in the blood plasma can be expected) (see sections “Contraindications” and “Pharmacokinetics”).
Lack of benefit on clinical outcomes in patients with symptomatic stable angina
Ivabradine is indicated only for symptomatic treatment of stable angina because ivabradine does not have a beneficial effect on the incidence of cardiovascular events (eg, myocardial infarction or cardiovascular death) in patients with angina.
Heart rate control
Given the significant variability of heart rate during the day, before starting therapy with ivabradine or before increasing the dose of ivabradine in a patient receiving the drug, resting heart rate should be assessed by one of the following methods: serial measurement of heart rate at rest, resting ECG, or 24-hour ambulatory ECG monitoring. Such an assessment should also be carried out in patients with a low heart rate (especially if the heart rate becomes less than 50 beats/min) or after a dose reduction of ivabradine.
Heart rhythm disturbances
Ivabradine is not effective for treating or preventing heart rhythm problems. The effectiveness of ivabradine is reduced by the development of tachyarrhythmia (for example, ventricular or supraventricular tachycardia). Ivabradine is not recommended for use in patients with atrial fibrillation (atrial fibrillation) or other arrhythmias affecting sinus node function.
Patients taking ivabradine are at increased risk of developing atrial fibrillation. Atrial fibrillation was more common among patients who were taking amiodarone or class I antiarrhythmic drugs concomitantly with ivabradine.
During ivabradine therapy, patients should be clinically monitored for atrial fibrillation (paroxysmal or persistent). For clinical indications (for example, worsening of angina, the appearance of palpitations, irregular heart rhythm), ECG monitoring should be included in routine monitoring. Patients should be informed about the signs and subjective symptoms of atrial fibrillation and the need to consult a doctor if such symptoms occur.
If atrial fibrillation occurs during therapy with ivabradine, the relationship between the expected benefit and the possible risk of continued use of ivabradine should be carefully reconsidered.
Patients with CHF and intraventricular conduction disorders (left or right bundle branch block) and ventricular dyssynchrony should be under close medical supervision
Use in patients with bradycardia
The use of Bravadin is contraindicated in patients with a heart rate less than 70 beats/min at rest before starting therapy.
If, when using the drug Bravadin, the resting heart rate decreases to less than 50 beats/min or the patient experiences symptoms associated with bradycardia (dizziness, fatigue or a marked decrease in blood pressure), the dose of the drug must be reduced.
If, when the dose of Bravadin is reduced, the heart rate remains less than 50 beats/min or symptoms associated with bradycardia persist, therapy with Bravadin should be discontinued.
Combined use as part of antianginal therapy
The simultaneous use of the drug Bravadin with BMCCs that reduce the pulse (verapamil, diltiazem) is not recommended. When used simultaneously with nitrates or BMCC, dihydropyridine derivatives (amlodipine), no changes in the safety profile of the therapy were observed. It has not been established that simultaneous use with BMCA, dihydropyridine derivatives, increases the effectiveness of ivabradine.
CHF
The possibility of using the drug Bravadin is considered only in patients with stable CHF. When using the drug Bravadin in patients with CHF IV functional class according to the NYHA classification, caution should be exercised due to the limited amount of data on use in this group of patients.
Stroke
The use of Bravadin immediately after a stroke is not recommended due to the lack of data on effectiveness and safety during this period.
Visual functions
The drug Bravadin affects the function of the retina. There is no evidence of toxic effects of long-term use of bravadin on the retina (see section “Pharmacodynamics”). If any visual disturbances not described in these instructions occur, use of the drug Bravadin should be discontinued. Caution should be exercised when using Bravadin in patients with retinal pigmentary degeneration.
Arterial hypotension
Bravadin should be used with caution in patients with arterial hypotension (insufficient clinical data).
The use of Bravadin is contraindicated in patients with severe arterial hypotension (systolic blood pressure less than 90 mm Hg and diastolic blood pressure less than 50 mm Hg).
Atrial fibrillation (atrial fibrillation) – heart rhythm disturbances
There is no proven increase in the risk of developing severe bradycardia with the use of Bravadin when restoring sinus rhythm during pharmacological cardioversion. However, due to the lack of sufficient data, if it is possible to delay elective electrical cardioversion, the use of Bravadin should be discontinued 24 hours before it is performed.
Use in patients with congenital long QT syndrome or in patients taking drugs that prolong the QT interval
The drug Bravadin is not used in patients with congenital long QT syndrome, as well as in patients taking drugs that prolong the QT interval. If concomitant use is necessary, strict ECG monitoring is required.
A decrease in heart rate due to the use of the drug Bravadin can aggravate the prolongation of the QT interval and provoke the development of a severe form of arrhythmia, in particular, polymorphic ventricular tachycardia of the “pirouette” type.
Patients with hypertension who require changes in antihypertensive therapy
In a clinical study, cases of increased blood pressure were more common in the group of patients taking ivabradine (7.1%) compared to the placebo group (6.1%).
Such cases occurred especially often immediately after a change in antihypertensive therapy, were temporary in nature and did not affect the effectiveness of ivabradine therapy. When changing antihypertensive therapy in patients with CHF taking Bravadin, blood pressure should be monitored at certain intervals.
Moderate liver failure
Caution should be exercised when using Bravadin in patients with moderate liver failure (7-9 points on the Child-Pugh scale).
Severe renal failure
Caution should be exercised when using Bravadin in patients with severe renal failure (creatinine clearance less than 15 ml/min).
Special information on excipients
The drug Bravadin contains lactose, so the drug is contraindicated in patients with lactase deficiency, lactose intolerance, and glucose-galactose malabsorption syndrome.
A study was conducted to evaluate the possible effect of ivabradine on driving ability in healthy volunteers, and the results showed no changes in driving ability. However, in the post-marketing period, cases of deterioration in the ability to drive vehicles due to symptoms associated with visual impairment have been reported.
The drug Bravadin can cause a temporary change in light perception (mainly in the form of photopsia), which should be taken into account when driving vehicles or other mechanisms when there is a sharp change in light intensity, especially at night.
Active ingredient
Active ingredient
Ivabradin
Composition
Composition
for 1 tablet 5 mg/7.5 mg:
Core:
Active ingredient:
Ivabradine hydrobromide 5.864 mg/8.796 mg, which corresponds to ivabradine 5 mg/7.5 mg
Excipients:
Lactose monohydrate, microcrystalline cellulose, povidone-K30, croscarmellose sodium, colloidal silicon dioxide, magnesium stearate
Film shell:
Opadry orange 03H325991
1Composition of Opadry orange 03H32599:
Hypromellose, titanium dioxide (E171), talc, propylene glycol, iron oxide yellow (E172), iron oxide red (E172)
Pregnancy
Pregnancy
Pregnancy
Animal studies have demonstrated the presence of reproductive toxicity, embryotoxicity and teratogenicity.
The drug Bravadin is contraindicated for use during pregnancy due to insufficient safety data.
Breastfeeding period
The use of Bravadin during breastfeeding is contraindicated.
It is not known whether ivabradine passes into breast milk.
If it is necessary to use the drug Bravadin during lactation, breastfeeding should be discontinued.
Contraindications
Contraindications
· Hypersensitivity to ivabradine or any of the auxiliary components of the drug.
· Heart rate at rest is less than 70 beats/min (before treatment).
· Cardiogenic shock.
· Acute myocardial infarction.
· Severe arterial hypotension (systolic blood pressure less than 90 mm Hg and diastolic blood pressure less than 50 mm Hg).
· Severe liver failure (more than 9 points on the Child-Pugh scale).
· Sick sinus syndrome.
· Sinoatrial blockade.
· Unstable or acute heart failure.
· Pacemaker dependence (conditions in which the heart rhythm is controlled solely by the pacemaker).
· Unstable angina.
· Atrioventricular (AV) block of II and III degrees.
· Concomitant use with potent inhibitors of the cytochrome P4503A4 isoenzyme system, such as antifungals of the azole group (ketoconazole, itraconazole), macrolide antibiotics (clarithromycin, erythromycin for oral administration, josamycin, telithromycin), HIV protease inhibitors (nelfinavir, ritonavir) and nefazodone (see sections “Pharmacokinetics” and “Interaction with other drugs”).
· Concomitant use with verapamil or diltiazem, which are moderate inhibitors of the CYP3A4 isoenzyme that have the ability to reduce heart rate (see section “Interaction with other drugs”).
· Pregnancy, breastfeeding and use in women of reproductive age who do not comply with reliable contraceptive measures (see section “Use during pregnancy and breastfeeding”).
· Age up to 18 years (the effectiveness and safety of the drug in this age group have not been established).
· Lactase deficiency, lactose intolerance, glucose-galactose malabsorption syndrome.
Side Effects
Side Effects
Ivabradine was studied in clinical studies involving nearly 45,000 patients. The most common side effects of ivabradine, changes in light perception (phosphenes) and bradycardia, were dose-dependent and related to the drug’s mechanism of action.
List of adverse reactions
The frequency of adverse reactions that were noted in clinical studies is given in the following gradation: very often (³ 1/10); often (³ 1/100,< 1/10); uncommon (³ 1/1000, < 1/100); rare (³ 1/10000, < 1/1000); very rare (< 1/10000); frequency unknown (frequency cannot be estimated from available data).
Nervous system disorders:
often: headache, especially in the first month of therapy, dizziness, possibly associated with bradycardia;
Uncommon: syncope, possibly associated with bradycardia.
Visual disorders:
very common: changes in light perception (phosphenes) were noted in 14.5% of patients and were described as a transient change in brightness in a limited area of the visual field. As a rule, such phenomena were provoked by a sharp change in lighting intensity. Phosphenes may also occur, which may have the appearance of a halo, disintegration of the visual image into separate parts (stroboscopic and kaleidoscopic effects), or appear in the form of bright color flashes or multiple images (retinal persistence). Basically, photopsia appeared in the first two months of treatment, but subsequently it could occur again. The severity of photopsia was usually mild or moderate. The appearance of photopsia stopped while therapy was continued (in 77.5% of cases) or after its completion. In less than 1% of patients, the appearance of photopsia was the reason for changing their lifestyle or refusing treatment;
often: blurred vision;
uncommon: diplopia, visual impairment.
Hearing and labyrinth disorders:
uncommon: vertigo.
Cardiac disorders:
often: bradycardia in 3.3% of patients, especially in the first 2-3 months of therapy; in > 0.5% of patients, severe bradycardia developed with a heart rate of no more than 40 beats/min, AV block of the first degree (prolongation of the PQ interval on the ECG), ventricular extrasystole, uncontrolled changes in blood pressure, atrial fibrillation was observed in 5.3% of patients receiving ivabradine, compared with 3.8% of patients receiving placebo. According to an analysis of pooled data from clinical studies with a follow-up period of at least 3 months, the occurrence of atrial fibrillation was observed in 4.86% of patients taking ivabradine, compared with 4.08% in control groups;
infrequently: palpitations, supraventricular estrusystole;
very rarely: AV block II and III degrees, sick sinus syndrome.
Vascular disorders:
often: marked decrease in blood pressure, possibly associated with bradycardia.
Disorders of the respiratory system, chest and mediastinal organs:
uncommon: shortness of breath.
Gastrointestinal disorders:
uncommon: nausea, constipation, diarrhea, abdominal pain.
Disorders of the skin and subcutaneous tissues:
uncommon: skin rash, angioedema;
rarely: erythema, itching, urticaria.
Musculoskeletal and connective tissue disorders:
uncommon: muscle spasms.
General disorders and disorders at the injection site:
uncommon: asthenia, increased fatigue, possibly associated with bradycardia;
rarely: malaise, possibly associated with bradycardia.
Laboratory and instrumental data:
uncommon: hyperuricemia, eosinophilia, increased plasma creatinine concentration, prolongation of the QT interval on the ECG.
Interaction
Interaction
Pharmacodynamic interaction
Concomitant use is not recommended
Drugs that prolong the QT interval:
· antiarrhythmic drugs that prolong the QT interval (for example, quinidine, disopyramide, bepridil, sotalol, ibutilide, amiodarone);
· Drugs that prolong the QT interval that are not antiarrhythmic drugs (for example, pimozide, ziprasidone, sertindole, mefloquine, halofantrine, pentamidine, cisapride, erythromycin for intravenous administration).
The simultaneous use of ivabradine and drugs that prolong the QT interval is not recommended, since a decrease in heart rate may cause additional prolongation of the QT interval. If concomitant use is necessary, careful ECG monitoring is required.
Concomitant use requiring caution
Potassium-sparing diuretics (thiazide and loop diuretics)
Hypokalemia may increase the risk of developing arrhythmia. Since the use of ivabradine can cause bradycardia, the combination of hypokalemia and bradycardia is a predisposing factor for the development of severe arrhythmia, especially in patients with long QT syndrome, both congenital and caused by the use of drugs.
Pharmacokinetic interaction
Isoenzyme CYP3A4
Ivabradine is metabolized in the liver using only the CYP3A4 isoenzyme and is a very weak inhibitor of this cytochrome. Does not affect the metabolism and plasma concentrations of other substrates (strong, moderate and weak inhibitors) of the CYP3A4 isoenzyme. Inhibitors and inducers of the CYP3A4 isoenzyme may interact with ivabradine and have a clinically significant effect on its metabolism and pharmacokinetic properties. Inhibitors of the CYP3A4 isoenzyme increase, and inducers of the CYP3A4 isoenzyme reduce the concentration of ivabradine in the blood plasma. An increase in the concentration of ivabradine in the blood plasma may cause a risk of developing severe bradycardia (see section “Special Instructions”).
Concomitant use is contraindicated
Concomitant use with potent inhibitors of the CYP3A4 isoenzyme, such as azole antifungals (ketoconazole, itraconazole), macrolide antibiotics (clarithromycin, oral erythromycin, josamycin, telithromycin), HIV protease inhibitors (nelfinavir, ritonavir) and nefazodone is contraindicated (see section “Contraindications”). Potent inhibitors of the CYP3A4 isoenzyme – ketoconazole (200 mg 1 time per day) or josamycin (1 g 2 times per day) increase the average concentration of ivabradine in the blood plasma by 7-8 times.
Moderate CYP3A4 inhibitors
The simultaneous use of ivabradine and diltiazem or verapamil (drugs that slow down heart rate) in healthy volunteers and patients was accompanied by an increase in AUC by 2-3 times and an additional decrease in heart rate by 5 beats/min. This use is contraindicated (see section “Contraindications”).
Concomitant use is not recommended
Grapefruit juice
When used simultaneously with grapefruit juice, there was a 2-fold increase in the concentration of ivabradine in the blood plasma. Drinking grapefruit juice is not recommended while taking ivabradine.
Concomitant use requiring caution
Moderate CYP3A4 inhibitors
Concomitant use of ivabradine with other moderate inhibitors of the CYP3A4 isoenzyme (for example, fluconazole) is possible if the resting heart rate is more than 70 beats/min. The recommended starting dose of ivabradine is 2.5 mg 2 times a day.
Heart rate control is required.
Inducers of the CYP3A4 isoenzyme
Inducers of the CYP3A4 isoenzyme (for example, rifampicin, barbiturates, phenytoin drugs containing St. John’s wort) may reduce the plasma concentration of ivabradine and its activity and require the selection of a higher dose of ivabradine. The simultaneous use of ivabradine at a dose of 10 mg 2 times a day and drugs containing St. John’s wort reduces the AUC of ivabradine by 2 times. The simultaneous use of drugs containing St. John’s wort and ivabradine is not recommended.
Simultaneous use with other drugs
There is no clinically significant effect on the pharmacodynamics and pharmacokinetics of ivabradine when used simultaneously with proton pump inhibitors (omeprazole, lansoprazole), phosphodiesterase-5 inhibitors (sildenafil), HMG-CoA reductase inhibitors (simvastatin), slow calcium channel blockers (SCBC) (amlodipine, lacidipine), digoxin and warfarin.
Ivabradine does not have a clinically significant effect on the pharmacokinetics of simvastatin, amlodipine, lacidipine, the pharmacokinetics and pharmacodynamics of digoxin, warfarin and the pharmacodynamics of acetylsalicylic acid.
The simultaneous use of ivabradine and ACE inhibitors, ARB II, beta-blockers, diuretics, aldosterone antagonists, short- and long-acting nitrates, HMG-CoA reductase inhibitors, fibrates, proton pump inhibitors, oral hypoglycemic agents, acetylsalicylic acid and other antiplatelet agents was not accompanied by a change in the safety profile of the therapy.
Overdose
Overdose
Symptoms
An overdose of Bravadin can lead to severe and prolonged bradycardia.
Treatment
Treatment of severe bradycardia is symptomatic and should be carried out in specialized hospital departments. In the case of a combination of bradycardia with impaired hemodynamic parameters, the use of beta-adrenergic agonists (isoprenaline) is necessary. If necessary, implantation of an electrical pacemaker.
Clinical pharmacology
Clinical pharmacology
Pharmacodynamics
Ivabradine is a drug that slows the heart rate, the mechanism of action of which is the selective and specific inhibition of If channels of the sinus node, which control spontaneous diastolic depolarization in the sinus node and regulate heart rate (HR). Ivabradine has a selective effect on the sinus node, without affecting the timing of impulses along the intra-atrial, atrioventricular and intraventricular pathways, as well as on myocardial contractility and ventricular repolarization.
Ivabradine can also interact with the Ih channels of the retina, similar to the If channels of the heart, which are involved in causing temporary changes in the visual perception system by changing the reaction of the retina to bright light stimuli.
Under provoking circumstances (for example, a rapid change in brightness in the visual field), partial inhibition of Ih channels by ivabradine causes the phenomenon of changes in light perception (photopsia). Photopsia is characterized by a transient change in brightness in a limited area of the visual field (see section “Side effects”).
The main pharmacological feature of ivabradine is the ability to dose-dependently reduce heart rate. Analysis of the dependence of the magnitude of the decrease in heart rate on the dose of ivabradine was carried out with a gradual increase in the dose to 20 mg 2 times a day and revealed a tendency to achieve a “plateau” effect (no increase in the therapeutic effect with a further increase in the dose), which reduces the risk of developing severe bradycardia (heart rate less than 40 beats/min) (see section “Side effects”).
When ivabradine is prescribed in recommended doses, the degree of heart rate decrease depends on its initial value and is approximately 10-15 beats/min at rest and during physical activity. As a result, the work of the heart decreases and the myocardium’s need for oxygen decreases.
Ivabradine does not affect intracardiac conduction, myocardial contractility (does not cause a negative inotropic effect) and the process of repolarization of the ventricles of the heart.
In clinical electrophysiological studies, ivabradine had no effect on the timing of impulses along the atrioventricular or intraventricular pathways, as well as on the corrected QT interval (QTc).
In studies involving patients with left ventricular dysfunction (left ventricular ejection fraction [LVEF] 30-45%), ivabradine was shown to have no effect on myocardial contractility.
It was found that ivabradine at a dose of 5 mg 2 times a day improved the performance of stress tests after 3-4 weeks of therapy. Efficacy was also confirmed for a dose of 7.5 mg 2 times a day. In particular, an additional effect was established when the dose was increased from 5 to 7.5 mg 2 times a day. The antianginal and anti-ischemic activity of ivabradine was also confirmed in patients aged 65 years and older. The effectiveness of ivabradine when used in doses of 5 mg and 7.5 mg 2 times a day was accompanied by a decrease in the incidence of angina attacks by approximately 70%. The use of ivabradine 2 times a day provided constant therapeutic effectiveness for 24 hours.
In studies of the clinical effectiveness of the drug, the effects of ivabradine were fully maintained throughout the 3 and 4 month treatment periods. During treatment, there were no signs of the development of tolerance (decreased effectiveness), and after cessation of treatment, no withdrawal syndrome was observed. The antianginal and antiischemic effects of ivabradine were associated with a dose-dependent decrease in heart rate, as well as a significant decrease in work product (heart rate x systolic blood pressure [BP]), both at rest and during exercise. The effect on blood pressure and total peripheral vascular resistance (TPVR) was minor and clinically insignificant.
A sustained decrease in heart rate was observed in patients taking ivabradine for at least 1 year. No effect on carbohydrate metabolism and lipid profile was observed.
In patients with diabetes mellitus, the efficacy and safety of ivabradine were similar to those in the general patient population.
The use of ivabradine showed an improvement in the functional class XCH according to the NYHA classification.
Patients with a heart rate of 80 beats/min showed a decrease in heart rate by an average of 15 beats/min.
In a randomized, placebo-controlled trial of 97 patients, specific ophthalmologic tests assessing the function of the cone-rod system and ascending visual pathway (eg, electroretinogram, static and kinetic perimetry, color vision testing, and visual acuity testing) in patients with chronic stable angina treated with ivabradine for more than 3 years revealed no retinal toxicity.
Pharmacokinetics
Ivabradine is an S-enantiomer that has not demonstrated biological conversion in in vivo studies. The N-desmethylated derivative of ivabradine is the main active metabolite.
Absorption and bioavailability
Ivabradine is rapidly and almost completely absorbed from the gastrointestinal tract after oral administration on an empty stomach, reaching maximum plasma concentrations (Cmax) in approximately 1 hour. Absolute bioavailability is about 40% and is due to the “first pass” effect through the liver.
Mealing increases the absorption time of ivabradine by approximately 1 hour and increases plasma concentrations from 20 to 30%. It is recommended to take the tablets with food to reduce concentration variability.
Distribution
Ivabradine binds to plasma proteins by approximately 70%; the volume of distribution in patients at steady state is about 100 liters. Cmax of ivabradine in blood plasma after long-term oral administration of a dose of 5 mg 2 times a day is 22 ng/ml (coefficient of variation (CV) = 29%). The average equilibrium concentration in blood plasma is 10 ng/ml (CV = 38%).
Metabolism
Ivabradine is largely metabolized in the liver and intestines by oxidation via the CYP3A4 isoenzyme. The main active metabolite is the N-desmethylated derivative (S18982) with a concentration of about 40% relative to the concentration of the parent substance. Metabolism of this active metabolite also occurs with the participation of the CYP3A4 isoenzyme. Ivabradine has a low affinity for the CYP3A4 isoenzyme and does not demonstrate clinically significant induction or inhibition of the CYP3A4 isoenzyme, therefore, changes in the metabolism or concentration of CYP3A4 substrates in the blood plasma under the influence of ivabradine are unlikely. On the contrary, potent inhibitors and inducers of the cytochrome P450 system can significantly affect the concentration of ivabradine in blood plasma.
Withdrawal
The half-life (T½) of ivabradine averages 2 hours (70-75% relative to the area under the concentration-time curve (AUC) in blood plasma), the effective T½ is 11 hours. Total clearance is about 400 ml/min, renal clearance is about 70 ml/min. Excretion of metabolites occurs to the same extent through the intestines and kidneys. About 4% of the dose taken orally is excreted unchanged by the kidneys.
Linearity/nonlinearity
The pharmacokinetics of ivabradine is linear in the dose range of 0.5-24 mg.
Special patient groups
Elderly and senile patients
Pharmacokinetic parameters (AUC and Cmax) do not differ significantly in elderly patients (≥ 65 years), geriatric patients (≥ 75 years) and the general patient population.
Impaired kidney function
Changes in the kinetics of ivabradine in patients with renal failure (creatinine clearance [CC] 15-60 ml/min) are minimal, since only about 20% of ivabradine and its active metabolite S 18982 are excreted by the kidneys.
Liver dysfunction
In patients with mild hepatic impairment (up to 7 points on the Child-Pugh scale), the AUC of ivabradine and its metabolite is 20% greater than in patients with normal liver function. Data on the use of ivabradine in patients with moderate liver failure (7-9 points on the Child-Pugh scale) are limited and do not allow us to draw a conclusion about the pharmacokinetics of ivabradine in this group of patients, and in patients with severe liver failure (more than 9 points on the Child-Pugh scale) are not available.
Relationship between pharmacokinetic and pharmacodynamic properties
The decrease in heart rate is directly proportional to the increase in plasma concentrations of ivabradine and the active metabolite S 18982 when taken in doses of 15-20 mg 2 times a day. At higher doses of the drug, the decrease in heart rate is not proportional to the concentration of ivabradine in the blood plasma and is characterized by a tendency to achieve a “plateau” effect. High plasma concentrations of ivabradine, which can be achieved with simultaneous use of ivabradine with strong inhibitors of the CYP3A4 isoenzyme, can lead to a pronounced decrease in heart rate, but this risk is reduced when used simultaneously with moderate inhibitors of the CYP3A4 isoenzyme.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C, in the original packaging.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use the drug after the expiration date.
Manufacturer
Manufacturer
KRKA-RUS, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 ° C, in the original package. Store out of the reach of children. |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | pills |
| Brand | KRKA dd Novo mesto |
Other forms…
Related products
Buy Bravadin, 5 mg 56 pcs. with delivery to USA, UK, Europe and over 120 other countries.