No products in the cart.
Bonviva, 150 mg
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacodynamics
Ibandronic acid is a highly active nitrogen-containing bisphosphonate, an inhibitor of bone resorption and osteoclast activity. Ibandronic acid prevents bone destruction caused by blockade of glandular function, retinoids, tumors and tumor extracts in vivo. Inhibits endogenous resorption in young (fast-growing) rats, which is manifested by higher bone mass compared to intact animals.
Does not impair bone mineralization when administered at doses more than 5000 times higher than doses for the treatment of osteoporosis and does not affect the process of osteoclast pool replenishment. The selective effect of ibandronic acid on bone tissue is due to its high affinity for hydroxyapatite, which constitutes the mineral matrix of bone.
Ibandronic acid inhibits bone resorption in a dose-dependent manner and has no direct effect on bone formation. In menopausal women it decreases increased rate of bone renewal to the level of reproductive age resulting in overall progressive increase of bone mass, decrease of bone collagen breakdown (concentration of deoxypyridinoline and cross-linked C- and N-telopeptides of collagen type I) in urine and serum, fracture rate and increase of BMD.
The high activity and therapeutic range allow for flexible dosing and intermittent administration of the drug with long periods of no treatment at relatively low doses.
Effectiveness
The administration of Bonviva 150 mg once a month for one year increases mean lumbar spine, femur, femoral neck, and trochanteric spine BMD by 4.9, 3.1, 2.2, and 4.6%; Boneviva 3 mg once every 3 months for 1 year increased mean BMD of the femur, femoral neck and trochanter by 2.4, 2.3 and 3.8%, respectively.
Independent of the duration of menopause and the degree of baseline bone mass loss, Bonviva leads to significantly more pronounced BMD changes than placebo. One-year benefit, defined as an increase in BMD, was seen in 83.9% (with coated tablets) and 92.1% (intravenous injection) of patients.
Biochemical markers of bone resorption
Shell tablets, 2.5 mg. Biochemical markers of bone resorption (concentration of C-terminal procollagen peptide type I in urine (CTX) and osteocalcin in blood serum) decrease to their levels in reproductive age; the maximum decrease is observed after 3-6 months of treatment. One month after the use of the drug Bonviva 2.5 mg daily and 20 mg in the intermittent mode, a clinically significant reduction of biochemical markers of bone resorption by 50 and 78% was achieved, respectively; moreover, some decrease in these figures was observed after one week of treatment. A clinically significant reduction in biochemical markers of bone resorption (CTX concentration in urine) was observed one month after the start of treatment.
Daily use of 2.5 mg of Bonviva for prevention of postmenopausal osteoporosis (study MF4499) increased mean lumbar spinal BMD by 1.9% over baseline. Regardless of the duration of menopause and the degree of baseline loss of basic bone substance, the use of Bonviva leads to significantly more pronounced changes in lumbar vertebral BMD. Benefit of Bonviva, defined as an increase in BMD over baseline, was seen in 70% of patients.
The coated tablets are 150 mg and the solution for intravenous injection. A 28% reduction in serum concentration of CTC was observed as early as 24 hours after the first administration of 150 mg of Bonviva, the maximum reduction was 68% after 6 days. After the third and fourth doses of Bonviva 150 mg, a maximum decrease in serum CTC of 74% was observed after 6 days. After 28 days of the fourth dose, a decrease in suppression of biochemical markers of bone resorption was observed up to 56%.
A clinically significant reduction in serum CBC was obtained after 3, 6 and 12 months of therapy. After one year of therapy with Bonviva 150 mg, the reduction was 76%; compared with the baseline value, when 3 mg was used intravenously, it was 58.6%.
A CTX reduction greater than 50% from baseline was seen in 83.5% of patients who received Bonviva 150 mg once every 28 days.
Pharmacokinetics
There is no direct correlation between the effectiveness of ibandronic acid and the plasma concentration of the substance. Plasma concentrations increase dose-dependently with increasing doses of intravenous solution from 0.5 to 6 mg. Similar efficacy of ibandronic acid has been confirmed with daily and intermittent regimens, provided that the total dose administered during the treatment period is the same.
Absorption
After oral administration ibandronic acid is rapidly absorbed in the upper gastrointestinal tract. Plasma concentrations increase dose-dependently with increasing doses up to 50 mg and significantly more with further increasing doses. Time of reaching Cmax (TCmax) is 0.5-2 hours (median – 1 hour) after an empty stomach, absolute bioavailability – 0.6%. Absorption is impaired when taking the drug with food or drinks (except pure water). Simultaneous intake of food or drinks (except pure water) reduces bioavailability of ibandronic acid by 90%. When taking ibandronic acid 60 min before a meal there is no significant decrease in bioavailability. Intake of food or liquid less than 60 min after ibandronic acid reduces its bioavailability and the induced increase in bone mineral density (BMD).
Distribution
After entering the systemic bloodstream, ibandronic acid is rapidly bound in the bone tissue or excreted in the urine. 40-50% of the drug circulating in the blood penetrates well into bone tissue and accumulates there. Apparent final volume of distribution is 90 l. Blood plasma protein binding is 85% when administered orally and 85-87% when administered intravenously.
Metabolism
There is no evidence that ibandronic acid is metabolized. Ibandronate does not inhibit the 1A2, 2A6, 2C9, 2C19, 2D6, 2E1 and 3A4 enzymes of the cytochrome P450 system.
40-50% of the absorbed in the bloodstream dose taken orally or injected intravenously is bound in the bone, and the rest is excreted unchanged by the kidneys.
The unabsorbed drug is excreted unchanged in the feces.
The terminal T1/2 for 2.5 mg tablets is 10-60 hours; for 150 mg tablets and intravenous solution it is 10-72 hours. The blood concentration of the drug decreases rapidly and is 10% of the maximum after 8 hours after oral administration and 3 hours after intravenous administration.
The total clearance of ibandronic acid is 84-160 ml/min. Renal clearance (60 ml/min in healthy menopausal women) is 50-60% of total clearance and depends on creatinine clearance. The difference between total and renal clearance reflects bone uptake of the substance.
Pharmacokinetics in Special Patient Groups
The pharmacokinetics of ibandronic acid is independent of gender.
There are no clinically significant interracial differences in the distribution of ibandronic acid in persons of Southern European and Asian race. There is insufficient data regarding the Negro race.
Patients with impaired renal function. In patients with impaired renal function, the renal clearance of ibandronic acid is linearly related to creatinine clearance (creatinine Cl). No dose adjustment is required in patients with mild to moderate renal dysfunction (creatinine Cl ≥30 ml/min).
In patients with severe renal impairment (creatinine Cl
Patients with impaired liver function. There are no data on the pharmacokinetics of ibandronic acid in patients with hepatic impairment. The liver does not play a significant role in the clearance of ibandronic acid, which is not metabolized but excreted through the kidneys and by capture in the bone tissue. Therefore, no dose adjustment is required for patients with impaired liver function.
Since when administered orally in therapeutic concentrations ibandronic acid weakly binds to plasma proteins (85%), it is likely that hypoproteinemia in severe liver disease does not lead to clinically significant increase in blood concentrations of free substance.
Elderly age. The studied pharmacokinetic parameters are independent of age. Possible decreased renal function in elderly patients should be considered.
Children. There are no data on the use of Bonviva in persons younger than 18 years of age.
Indications
Indications
Postmenopausal osteoporosis to prevent fractures.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Ibandronic acid is a highly active nitrogen-containing bisphosphonate, an inhibitor of bone resorption and osteoclast activity. Ibandronic acid prevents bone destruction caused by gonadal blockade, retinoids, tumors and tumor extracts in vivo. Inhibits endogenous resorption in young (fast-growing) rats, which is manifested by higher bone mass compared to intact animals.
Does not interfere with bone mineralization when administered in doses more than 5000 times higher than doses for the treatment of osteoporosis and does not affect the process of replenishment of the osteoclast pool. The selective effect of ibandronic acid on bone tissue is due to its high affinity for hydroxyapatite, which constitutes the mineral matrix of bone.
Ibandronic acid inhibits bone resorption in a dose-dependent manner and does not have a direct effect on bone formation. In menopausal women, it reduces the increased rate of bone tissue turnover to the level of reproductive age, which leads to an overall progressive increase in bone mass, a decrease in the breakdown of bone collagen (the concentration of deoxypyridinoline and cross-linked C- and N-telopeptides of type I collagen) in urine and blood serum, the incidence of fractures and an increase in BMD.
High activity and therapeutic range provide the possibility of a flexible dosing regimen and intermittent administration of the drug with a long period without treatment in relatively low doses.
Efficiency
Taking Bonviva 150 mg once a month for a year increases the average BMD of the lumbar vertebrae, hip, femoral neck and trochanter by 4.9, 3.1, 2.2 and 4.6%; IV administration of Bonviva 3 mg once every 3 months for 1 year increases the average BMD of the femur, femoral neck and trochanter by 2.4, 2.3 and 3.8%, respectively.
Regardless of the duration of menopause and the degree of initial bone loss, Bonviva resulted in a significantly greater change in BMD than placebo. The effect of treatment within a year, defined as an increase in BMD, is observed in 83.9% (when taking film-coated tablets) and 92.1% (when administered intravenously) of patients.
Biochemical markers of bone resorption
Film-coated tablets, 2.5 mg. Biochemical markers of bone resorption (urinary concentrations of type I procollagen C-terminal peptide (CTX) and serum osteocalcin) decline to their levels during reproductive age; the maximum reduction is observed after 3-6 months of treatment. Just one month after starting the use of Bonviva 2.5 mg daily and 20 mg intermittently, a clinically significant reduction in biochemical markers of bone resorption was achieved by 50 and 78%, respectively; Moreover, a slight decrease in these indicators was noted after a week of treatment. A clinically significant decrease in biochemical markers of bone resorption (urinary CTX concentrations) is observed one month after the start of treatment.
Bonviva 2.5 mg daily for the prevention of postmenopausal osteoporosis (study MF4499) increased mean lumbar spine BMD by 1.9% compared with baseline. Regardless of the duration of menopause and the degree of initial loss of basic bone tissue, the use of Bonviva leads to a significantly more pronounced change in BMD of the lumbar vertebrae. When using Bonviva, the treatment effect, defined as an increase in BMD compared to the baseline, is observed in 70% of patients.
Film-coated tablets, 150 mg and solution for intravenous administration. A 28% decrease in serum CTX concentration was noted within 24 hours after the first dose of 150 mg Bonviva, with a maximum decrease of 68% after 6 days. After the third and fourth doses of Bonviva 150 mg, the maximum decrease in serum CTX by 74% was observed after 6 days. 28 days after taking the fourth dose, a decrease in the suppression of biochemical markers of bone resorption was noted to 56%.
Clinically significant reductions in serum CTX were obtained after 3, 6 and 12 months of therapy. After a year of therapy with Bonviva 150 mg, the reduction was 76%; compared with the initial value, when using 3 mg intravenously – 58.6%.
A decrease in CTX of more than 50% compared to the initial value was observed in 83.5% of patients receiving Bonviva 150 mg once every 28 days.
Pharmacokinetics
There was no direct relationship between the effectiveness of ibandronic acid and the concentration of the substance in the blood plasma. The concentration in blood plasma increases in a dose-dependent manner as the dose of the solution for intravenous administration increases from 0.5 to 6 mg. Similar effectiveness of ibandronic acid was confirmed with daily and intermittent use, provided that the total dose administered during the treatment period was the same.
Suction
After oral administration, ibandronic acid is rapidly absorbed from the upper gastrointestinal tract. Plasma concentrations increase dose-dependently when the dose is increased to 50 mg and significantly more when the dose is further increased. Time to reach Cmax (TCmax) – 0.5–2 hours (median – 1 hour) after administration on an empty stomach, absolute bioavailability – 0.6%. Absorption is impaired when taking the drug with food or drinks (except pure water). Concomitant consumption of food or drinks (except pure water) reduces the bioavailability of ibandronic acid by 90%. When taking ibandronic acid 60 minutes before meals, no significant decrease in bioavailability is observed. Ingestion of food or liquid less than 60 minutes after ibandronic acid reduces its bioavailability and the resulting increase in bone mineral density (BMD).
Distribution
After entering the systemic circulation, ibandronic acid quickly binds to bone tissue or is excreted in the urine. 40–50% of the amount of the drug circulating in the blood penetrates well into bone tissue and accumulates in it. Apparent final volume of distribution 90 l. Communication with blood plasma proteins when administered orally is 85% and 85–87% when administered intravenously.
Metabolism
There is no evidence that ibandronic acid is metabolized. Ibandronate does not inhibit enzymes 1A2, 2A6, 2C9, 2C19, 2D6, 2E1 and 3A4 of the cytochrome P450 system.
Removal
40–50% of an orally or intravenously administered dose absorbed into the bloodstream is bound in the bones, and the rest is excreted unchanged by the kidneys.
The unabsorbed drug is excreted unchanged in the feces.
Terminal T1/2 for 2.5 mg tablets is 10–60 hours; for tablets 150 mg and solution for intravenous administration – 10–72 hours. The concentration of the drug in the blood decreases quickly and is 10% of the maximum 8 hours after oral administration and 3 hours after intravenous administration.
The total clearance of ibandronic acid is 84–160 ml/min. Renal clearance (60 ml/min in healthy menopausal women) accounts for 50–60% of the total clearance and depends on creatinine clearance. The difference between total and renal clearance reflects the uptake of the substance into bone tissue.
Pharmacokinetics in special groups of patients
The pharmacokinetics of ibandronic acid does not depend on gender.
There were no clinically significant interracial differences in the distribution of ibandronic acid in individuals of the Southern European and Asian races. There is not enough data regarding the Negroid race.
Patients with impaired renal function. In patients with impaired renal function, the renal clearance of ibandronic acid is linearly dependent on creatinine clearance (Cl creatinine). For patients with mild or moderate renal impairment (creatinine Cl ≥30 ml/min), no dose adjustment is required.
In patients with severe renal impairment (Cl creatinine
Patients with impaired liver function. There are no data on the pharmacokinetics of ibandronic acid in patients with impaired liver function. The liver does not play a significant role in the clearance of ibandronic acid, which is not metabolized but is excreted through the kidneys and by uptake into bone tissue. Therefore, for patients with impaired liver function, no dose adjustment is required.
Since, when taken orally in therapeutic concentrations, ibandronic acid weakly binds to plasma proteins (85%), it is likely that hypoproteinemia in severe liver diseases does not lead to a clinically significant increase in the concentration of the free substance in the blood.
Old age. The studied pharmacokinetic parameters do not depend on age. The possible decrease in renal function in elderly patients should be taken into account.
Children. There are no data on the use of Bonviva in persons under 18 years of age.
Special instructions
Special instructions
Risk factors for the development of postmenopausal osteoporosis and fractures are a family history, previous bone fractures, early menopause, active bone metabolism, low BMD (at least 1.0 SD less than the average BMD at reproductive age), frail physique, as well as women belonging to the Southern European and Asian race, smoking. These factors are of great importance when deciding whether to prescribe Bonviva film-coated tablets 2.5 mg for the prevention of osteoporosis.
Osteoporosis can be confirmed by detecting low BMD (T index
Before using Bonviva, hypocalcemia and other disorders of bone metabolism and electrolyte balance should be corrected. Patients should consume adequate amounts of calcium and vitamin D.
If the patient does not receive enough calcium and vitamin D from food, then they should be additionally taken in the form of nutritional supplements.
When taken orally, the side effects of the drug are usually mild or moderate. A transient flu-like syndrome is observed after taking the first dose and resolves independently without adjustment of therapy. There was no increase in the incidence of upper gastrointestinal adverse effects in patients with gastrointestinal diseases (including peptic ulcer without bleeding or hospitalization, dyspepsia or reflux disease).
The use of oral bisphosphonates is often accompanied by difficulty swallowing, esophagitis and the formation of ulcers of the esophagus and stomach, so special attention must be paid to following the recommendations for taking the drug (sitting or standing position for 60 minutes after administration).
If signs and symptoms of possible damage to the esophagus appear (the appearance or worsening of swallowing difficulties, pain when swallowing, chest pain, heartburn), you should stop taking Bonviva and consult a doctor.
Post-marketing experience with Bonviva is limited.
Serum creatinine should be determined before each injection.
Osteonecrosis of the jaw has been reported when bisphosphonates were prescribed. Most cases have been reported in patients with cancer during dental procedures, with a few cases in patients with postmenopausal osteoporosis or other diseases. Risk factors for the development of osteonecrosis of the jaw include an established diagnosis of cancer, concomitant therapy (chemotherapy, radiation therapy, corticosteroids) and other disorders (anemia, coagulopathy, infection, gum disease). Most cases were observed with intravenous bisphosphonates, but isolated cases were observed in those receiving oral drugs.
Dental surgery during bisphosphonate therapy can increase the manifestations of osteonecrosis of the jaw. It is unknown whether discontinuation of bisphosphonates reduces the risk of osteonecrosis. The decision to conduct treatment must be made for each patient individually after assessing the risk/benefit ratio.
Active ingredient
Active ingredient
Ibandronic acid
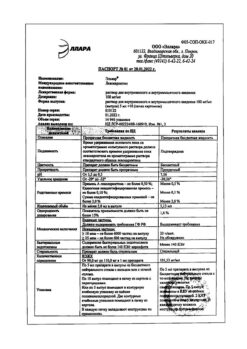
Composition
Composition
1 film-coated tablet contains:
active ingredient:
ibandronic acid 150 mg (as sodium ibandronate monohydrate)
excipients:
lactose monohydrate,
povidone (K 25),
microcrystalline cellulose,
crospovidone,
stearic acid,
anhydrous colloidal silicon dioxide.
Pregnancy
Pregnancy
Pregnancy. During preclinical studies, no evidence of direct embryotoxic or teratogenic effects was found; at a dose of the drug exceeding the human dose by at least 35 times, no adverse effect on the development of offspring in F1 rats was detected.
The adverse effects of ibandronic acid in reproductive toxicity studies in animals were the same as for all bisphosphonates: decreased embryo production, disruption of labor, increased incidence of visceral abnormalities (stenosis of the ureteropelvic segment).
There is no experience of clinical use of Bonviva in pregnant women.
Breastfeeding period. Excreted in milk in animals. After 24 hours, the concentration of ibandronic acid in blood plasma and milk is the same and corresponds to 5% of the maximum.
It is unknown whether ibandronic acid is excreted in breast milk in women.
Contraindications
Contraindications
hypersensitivity to ibandronic acid or other components of the drug;
hypocalcemia (hypocalcemia should be eliminated before starting Bonviva, as with all bisphosphonates used to treat osteoporosis).
With caution: severe renal impairment (Cl creatinine).
Side Effects
Side Effects
From the gastrointestinal tract: dyspepsia, diarrhea, gastritis.
From the musculoskeletal system: arthralgia, myalgia.
From the nervous system: headache, dizziness.
Body as a whole: influenza-like syndrome.
From the skin and its appendages: rash.
Hypersensitivity reactions: angioedema, urticaria.
Very rarely, osteonecrosis of the jaw has been observed when ibandronic acid was prescribed.
From the gastrointestinal tract: esophagitis, ulcer or stricture of the esophagus, duodenitis.
From the gastrointestinal tract: nausea, vomiting, abdominal pain, dysphagia, flatulence, gastroesophageal reflux.
From the musculoskeletal system: muscle stiffness, muscle spasm.
Interaction
Interaction
Products containing calcium and other polyvalent cations (for example aluminum, magnesium, iron), incl. Milk and solid foods may interfere with the absorption of the drug and should be consumed no earlier than 60 minutes after oral administration of Bonviva.
Calcium supplements, antacids and medications containing polyvalent cations (eg aluminum, magnesium, iron) may interfere with the absorption of ibandronic acid and should therefore be taken no earlier than 60 minutes after taking Bonviva.
Bisphosphonates and NSAIDs can cause irritation of the gastrointestinal mucosa. Particular caution should be exercised when using NSAIDs concomitantly with Bonviva. When aspirin or NSAIDs were used concomitantly with Bonviva for 1 year, the incidence of upper gastrointestinal side effects was similar.
Ranitidine intravenously increases the bioavailability of ibandronic acid by 20%. No dosage adjustment of ibandronic acid is required when used concomitantly with H2-histamine receptor blockers or other drugs that increase gastric pH.
Ibandronic acid does not affect the activity of the main isoenzymes of the cytochrome P450 system. At therapeutic concentrations, ibandronic acid weakly binds to plasma proteins, and therefore it is unlikely that it will displace other drugs from protein binding sites. Ibandronic acid is excreted only through the kidneys and does not undergo any biotransformation. It appears that the elimination pathway of ibandronic acid does not involve any of the transport systems involved in the elimination of other drugs.
Overdose
Overdose
Symptoms: dyspepsia, heartburn, esophagitis, gastritis, ulcers, hypocalcemia, hypophosphatemia
Treatment: no specific information available. Milk or antacids are used to bind Bonviva. Due to the risk of esophageal irritation, vomiting should not be induced and the patient should remain in an upright standing position.
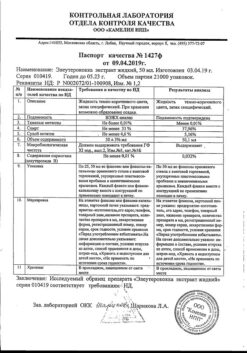
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C
Shelf life
Shelf life
2 years.
Manufacturer
Manufacturer
F.Hoffmann-La Roche Ltd, Switzerland
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | F. Hoffmann-La Roche Ltd, Switzerland |
| Medication form | pills |
| Brand | F. Hoffmann-La Roche Ltd |
Related products
Buy Bonviva, 150 mg with delivery to USA, UK, Europe and over 120 other countries.