No products in the cart.
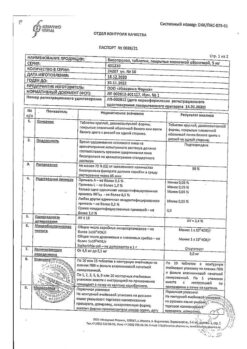
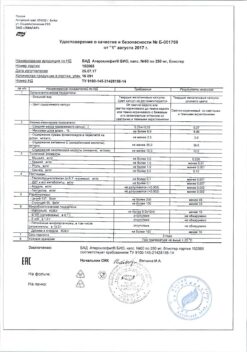
Bisoprolol, 5 mg 50 pcs.
€4.55 €4.04
Description
Pharmacotherapeutic group: selective beta1-adrenoblocker
ATX code: C07AB07
Pharmacological properties
Pharmacodynamics
A selective beta1-adrenoblocker with no sympathomimetic activity of its own, has no membrane-stabilizing action.
Bisoprolol in therapeutic doses has negligible affinity for beta2-adrenoreceptors of internal organs (pancreas, skeletal muscles, smooth muscle of peripheral arteries, bronchi and uterus) as well as for beta2-adrenoreceptors involved in metabolism regulation. Consequently, bisoprolol (unlike non-selective beta-adrenoblockers) in general does not affect the airway resistance, has a less pronounced effect on the organs containing beta2-adrenoreceptors and on carbohydrate metabolism, does not cause sodium ion retention in the body. The atherogenic effect of bisoprolol does not differ from that of propranolol. When increasing the dose above the therapeutic dose, bisoprololol loses selectivity and has beta2-adrenoblocking effect.
In therapeutic doses, bisoprololol blocks beta1-adrenoceptors of the heart, reduces catecholamine-stimulated formation of cyclic adenosine monophosphate (cAMP) from adenosine triphosphate (ATP), reduces intracellular calcium ions (Ca2+) flow, has negative chrono-, dromo-, batmo- and inotropic effects.
Bisoprolol reduces heart rate (HR) at rest and during exercise, slows atrioventricular (AV) conduction, reduces myocardial excitability. It reduces cardiac output, slightly reduces stroke volume, increases right atrial pressure and pulmonary artery congestion pressure at rest and during exercise.
Limits myocardial oxygen demand, reduces plasma renin activity. At the beginning of treatment in the first 24 hours after bisoprolol administration, total peripheral vascular resistance (TPRR) increases slightly (as a result of reciprocal increase of alpha-adrenoreceptor activity). After 1 to 3 days, OPPS returns to baseline.
In long-term therapy initially increased OPPS decreases.
The maximum hemodynamic effect is reached 3-4 hours after oral administration. When administered once daily therapeutic effect of bisoprololol is maintained for 24 hours due to 10-12 hour blood plasma elimination half-life.
Bisoprolol has the same electrophysiological effects as other beta-adrenoblockers. In electrophysiological studies, bisoprolol decreased HR, increased conduction time and refractory periods of sinoatrial and AV nodes. There was a prolongation of RR and PQ intervals as well as corrected QT interval (qtc) on ECG (within normal values).
Bisoprolol has antihypertensive, antianginal, and antiarrhythmic effects.
The mechanism of antihypertensive action of bisoprolol is not fully understood. Antihypertensive effect may be due to the decrease of the minute blood volume, sympathetic stimulation of peripheral vessels, decrease of plasma renin and renin-angiotensin system activity (important for patients with initial renin hypersecretion), restoration of aortic arch baroreceptors sensitivity in response to blood pressure (BP) decrease and the effect on the central nervous system (CNS). In arterial hypertension the effect comes in 2-5 days, the maximum BP decrease is usually reached in 2 weeks after the treatment start.
The antianginal effect is caused by decrease of myocardial oxygen demand as a result of HR shortening, slight decrease of contractility, prolongation of diastole, improvement of myocardial perfusion. When administered once in patients with coronary heart disease (CHD) without signs of chronic heart failure (CHF), bisoprolol decreases HR, cardiac stroke volume and, consequently, decreases ejection fraction and myocardial oxygen demand.
The antiarrhythmic effect is caused by the elimination of arrhythmogenic factors (tachycardia, increased activity of the sympathetic nervous system, increased content of CAMF, arterial hypertension), decrease of spontaneous excitation rate of sinus and ectopic pacemakers and delay of AV conduction (mainly in antegrade and, to a lesser degree, in retrograde direction through AV node) and through additional pathways.
In clinical trials in patients with stable CHF of III-IV functional class according to NYHA classification (left ventricular ejection fraction < 35%) bisoprolol administration resulted in decrease of total mortality, sudden death and reduction of number of decompensation episodes of CHF requiring hospitalization. There was also a decrease in functional class of CHF by NYHA classification.
Pharmacokinetics
Intake. Bisoprolol is almost completely (> 90%) absorbed from the gastrointestinal tract. Its bioavailability due to insignificant metabolism during “primary passage” through the liver (at about 10-15%) is about 85-90% after oral administration. Food intake has no effect on the bioavailability of bisoprolol. Bisoprolol exhibits linear kinetics, with plasma concentrations proportional to the administered dose in the dose range of 5 to 20 mg. Maximum plasma concentrations are reached after 2-3 hours.
Distribution. Bisoprolol is distributed quite widely. The volume of distribution is 3.5 l/kg. Bisoprolol binding to blood plasma proteins reaches approximately 35%; bisoprolol uptake by blood cells is not observed.
Metabolism. Bisoprolol is metabolized by the oxidative pathway without subsequent conjugation. All metabolites are strongly polar and are excreted by the kidneys.
The major metabolites found in plasma and urine have no pharmacological activity. The data obtained from in vitro experiments with human liver microsomes show that bisoprolol is metabolized primarily by the CYP3A4 isoenzyme (approximately 95%) and the CYP2D6 isoenzyme plays only a minor role.
Elimination. Bisoprolol clearance is determined by a balance between its excretion through the kidneys as unchanged substance (about 50%) and its oxidation in the liver (about 50%) to metabolites, which are then also excreted by the kidneys. Total clearance of bisoprololol is 15.6±3.2 L/h, with renal clearance of 9.6±1.6 L/h. The half-life (T1/2) of bisoprololol is 10-12 hours.
Since excretion occurs equally in the kidneys and the liver, patients with impaired hepatic function or with renal failure do not require dose adjustments. The pharmacokinetics of bisoprolol are linear and independent of age.
Pharmacokinetics in special patient groups
Renal dysfunction
. In a study in patients with renal impairment (mean creatinine clearance [CK] 28 mL/min), it was shown that a decrease in CK was accompanied by an increase in Cmax, AUC (area under the concentration-time curve), and T1/2 of bisoprololol. Since clearance of bisoprololol is equally handled by the kidneys and liver, there is no significant cumulation of bisoprolol in patients with severe renal impairment.
Hepatic disorders
In patients with cirrhosis, there is high variability and significant delayed elimination compared to healthy subjects (T1/2 of bisoprololol is 8.3 to 21.7 hours). No clinically significant differences in pharmacokinetics were found between patients with normal and impaired liver function.
Chronic Heart Failure
In patients with NYHA functional class III CHF, higher plasma bisoprolol levels and increased T1/2 were noted compared to healthy volunteers. Maximal bisoprolol plasma concentration at equilibrium is 64±21 ng/ml at a daily dose of 10 mg; T1/2 is 17±5 hours. The pharmacokinetics of bisoprololol in patients with CHF and concomitant hepatic or renal impairment have not been studied.
Elderly patients
In elderly patients a slight increase in some pharmacokinetic parameters (Tl/2, AUC, Cmaõ) of bisoprolol compared to younger patients has been noted, presumably due to age-related decrease in renal clearance. However, these differences are not clinically significant and do not require bisoprololol dose adjustment.
Indications
Indications
arterial hypertension;
IHD: stable angina;
CHF.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: selective beta1-blocker
ATX code: С07АВ07
Pharmacological properties
Pharmacodynamics
A selective beta1-blocker, without its own sympathomimetic activity, does not have a membrane-stabilizing effect.
Bisoprolol in therapeutic doses has little affinity for beta2-adrenergic receptors of internal organs (pancreas, skeletal muscles, smooth muscles of peripheral arteries, bronchi and uterus), as well as for beta2-adrenergic receptors involved in the regulation of metabolism. Consequently, bisoprolol (unlike non-selective beta-blockers) generally does not affect respiratory tract resistance, has a less pronounced effect on organs containing beta2-adrenergic receptors and on carbohydrate metabolism, and does not cause sodium ion retention in the body. The severity of the atherogenic effect of bisoprolol does not differ from the effect of propranolol. When the dose is increased above the therapeutic dose, bisoprolol loses selectivity and has a beta2-adrenergic blocking effect.
In therapeutic doses, bisoprolol blocks beta1-adrenergic receptors of the heart, reduces catecholamine-stimulated formation of cyclic adenosine monophosphate (cAMP) from adenosine triphosphate (ATP), reduces the intracellular current of calcium ions (Ca2+), and has a negative chrono-, dromo-, bathmo- and inotropic effect.
Bisoprolol reduces heart rate (HR) at rest and during exercise, slows down atrioventricular (AV) conduction, and reduces myocardial excitability. Reduces cardiac output, slightly reduces stroke volume, increases right atrial pressure and pulmonary artery wedge pressure at rest and during exercise.
Reduces myocardial oxygen demand and reduces plasma renin activity. At the beginning of treatment in the first 24 hours after taking bisoprolol, total peripheral vascular resistance (TPVR) increases slightly (as a result of a reciprocal increase in the activity of alpha-adrenergic receptors). After 1-3 days, the OPSS returns to its original level.
With long-term therapy, the initially elevated TPR decreases.
The maximum hemodynamic effect is achieved 3-4 hours after oral administration. When used once a day, the therapeutic effect of bisoprolol lasts for 24 hours due to a 10-12 hour half-life from the blood plasma.
Bisoprolol has the same electrophysiological effects as other beta-blockers. In electrophysiological studies, bisoprolol reduced heart rate and increased conduction time and refractory periods of the sinoatrial and AV nodes. There is a prolongation of the RR and PQ intervals, as well as the corrected QT (qtc) interval on the ECG (within normal values).
Bisoprolol has antihypertensive, antianginal and antiarrhythmic effects.
The mechanism of the antihypertensive effect of bisoprolol has not been fully studied. The antihypertensive effect may be associated with a decrease in minute blood volume, sympathetic stimulation of peripheral vessels, a decrease in plasma renin and activity of the renin-angiotensin system (of great importance for patients with initial renin hypersecretion), restoration of the sensitivity of the aortic arch baroreceptors in response to a decrease in blood pressure (BP) and an effect on the central nervous system (CNS). For arterial hypertension, the effect occurs within 2-5 days; the maximum reduction in blood pressure is usually achieved 2 weeks after the start of treatment.
The antianginal effect is due to a decrease in myocardial oxygen demand as a result of a decrease in heart rate, a slight decrease in contractility, prolongation of diastole, and improved myocardial perfusion. When used once in patients with coronary heart disease (CHD) without signs of chronic heart failure (CHF), bisoprolol reduces heart rate, stroke volume and, as a result, reduces the ejection fraction and myocardial oxygen demand.
The antiarrhythmic effect is due to the elimination of arrhythmogenic factors (tachycardia, increased activity of the sympathetic nervous system, increased cAMP content, arterial hypertension), a decrease in the rate of spontaneous excitation of sinus and ectopic pacemakers and a slowdown of AV conduction (mainly in the antegrade and, to a lesser extent, in the retrograde directions through the AV node) and along additional pathways.
In clinical studies in patients with stable CHF III-IV functional class according to the NYHA classification (left ventricular ejection fraction <35%), the use of bisoprolol led to a decrease in overall mortality, sudden death and a decrease in the number of episodes of CHF decompensation requiring hospitalization. There was also a decrease in the functional class of CHF according to the NYHA classification.
Pharmacokinetics
Suction. Bisoprolol is almost completely (> 90%) absorbed from the gastrointestinal tract. Its bioavailability due to insignificant metabolism during the “first pass” through the liver (at a level of approximately 10-15%) is approximately 85-90% after oral administration. Food intake does not affect the bioavailability of bisoprolol. Bisoprolol exhibits linear kinetics, with plasma concentrations being proportional to the administered dose over a dose range of 5 to 20 mg. The maximum concentration in blood plasma is achieved after 2-3 hours.
Distribution. Bisoprolol is distributed quite widely. The volume of distribution is 3.5 l/kg. The binding to plasma proteins reaches approximately 35%; uptake of bisoprolol by blood cells is not observed.
Metabolism. Bisoprolol is metabolized via the oxidative pathway without subsequent conjugation. All metabolites have strong polarity and are excreted by the kidneys.
The main metabolites found in blood plasma and urine do not exhibit pharmacological activity. Data obtained from experiments with human liver microsomes in vitro show that bisoprolol is metabolized primarily by the CYP3A4 isoenzyme (about 95%), and the CYP2D6 isoenzyme plays only a minor role.
Excretion. The clearance of bisoprolol is determined by the balance between its excretion through the kidneys in the form of unchanged substance (about 50%) and oxidation in the liver (about 50%) to metabolites, which are then also excreted by the kidneys. The total clearance of bisoprolol is 15.6±3.2 l/h, with renal clearance being 9.6±1.6 l/h. The half-life (T1/2) of bisoprolol is 10-12 hours.
Since excretion occurs equally in the kidneys and liver, no dosage adjustment is required in patients with impaired liver function or renal failure. The pharmacokinetics of bisoprolol is linear and does not depend on age.
Pharmacokinetics in special groups of patients
Renal dysfunction
In a study in patients with renal failure (average creatinine clearance [CC] 28 ml/min), it was shown that a decrease in creatinine clearance is accompanied by an increase in Cmax, AUC (area under the concentration-time curve) and T1/2 of bisoprolol. Since bisoprolol is cleared equally by the kidneys and liver, there is no significant accumulation of bisoprolol in patients with severe renal failure.
Liver dysfunction
In patients with liver cirrhosis, there is high variability and a significant slowdown in elimination compared to healthy people (T1/2 of bisoprolol ranges from 8.3 to 21.7 hours). Clinically significant differences in pharmacokinetics between patients with normal and impaired liver function were not identified.
Chronic heart failure
In patients with CHF functional class III according to the NYHA classification, higher levels of bisoprolol in the blood plasma and increased T1/2 were noted compared to healthy volunteers. The maximum concentration of bisoprolol in blood plasma at steady state is 64±21 ng/ml at a daily dose of 10 mg; T1/2 is 17±5 hours. The pharmacokinetics of bisoprolol in patients with CHF and concomitant liver or kidney dysfunction have not been studied.
Elderly patients
In elderly patients, there is a slight increase in some pharmacokinetic parameters (Tl/2, AUC, Cmax) of bisoprolol compared to young patients, presumably due to an age-related decrease in renal clearance. However, these differences are not clinically significant and do not require dose adjustment of bisoprolol.
Special instructions
Special instructions
Termination of therapy and “withdrawal syndrome”
You should not abruptly interrupt treatment with bisoprolol or change the recommended dose without first consulting your doctor, as this may lead to a temporary deterioration in heart function. Treatment should not be interrupted suddenly, especially in patients with coronary artery disease (increased severity of angina attacks, the development of myocardial infarction and the occurrence of ventricular arrhythmias in patients with coronary artery disease with sudden cessation of beta-blockers have been noted). If discontinuation of treatment is necessary, the dose of bisoprolol should be reduced gradually. In case of significant worsening of angina or development of acute coronary syndrome, bisoprolol should be temporarily resumed.
Diseases for which it is necessary to use the drug with caution Bisoprolol should be used with caution in the following cases: severe forms of COPD and mild forms of bronchial asthma; diabetes mellitus with significant fluctuations in blood glucose concentrations: bisoprolol may mask symptoms of hypoglycemia (a marked decrease in blood glucose concentrations), such as tachycardia, palpitations or increased sweating; strict diet; carrying out desensitizing therapy; AV block of the first degree; vasospastic angina (Prinzmetal’s angina); mild to moderate peripheral arterial circulatory disorders (increased symptoms may occur at the beginning of therapy); psoriasis (including history).
Diseases of the cardiovascular system
Beta blockers should not be used for decompensated CHF until the patient’s condition has stabilized.
At the initial stages of using bisoprolol, patients need constant monitoring.
Beta blockers may cause bradycardia. If the heart rate at rest decreases to less than 50-55 beats/min, the dose should be reduced or discontinued taking bisoprolol.
Like other beta blockers, bisoprolol may cause a prolongation of the PQ interval on the ECG. Bisoprolol should be used with caution in patients with first degree AV block.
Non-selective beta-blockers may increase the frequency and duration of anginal attacks in patients with vasospastic angina (Prinzmetal’s angina) due to alpha-receptor-mediated coronary artery vasoconstriction. Cardioselective beta1-blockers (including bisoprolol) should be used with caution in vasospastic angina.
To date, there is insufficient data regarding the use of bisoprolol in patients with CHF in combination with type 1 diabetes mellitus, severe renal and/or liver dysfunction, restrictive cardiomyopathy, congenital heart defects or heart valve disease with severe hemodynamic disturbances. Also, sufficient data have not yet been obtained regarding patients with CHF with myocardial infarction within the last 3 months.
Respiratory system
Despite the fact that selective beta1-blockers have a lesser effect on the function of the respiratory system than non-selective beta-blockers, patients with COPD and mild forms of bronchial asthma should be prescribed bisoprolol with extreme caution and only if the possible benefits of its use outweigh the potential risks. For bronchial asthma or COPD, simultaneous use of bronchodilators is indicated. In patients with bronchial asthma, there may be an increase in airway resistance, which requires a higher dose of beta2-agonists.
In patients with COPD, bisoprolol prescribed in combination therapy for the treatment of heart failure should be started at the lowest possible dose, and patients should be carefully monitored for the appearance of new symptoms (eg, shortness of breath, exercise intolerance, cough).
Major surgery and general anesthesia
If surgical interventions are necessary, the anesthesiologist should be warned that the patient is taking beta-blockers (risk of drug interactions with the development of severe bradyarrhythmias, reduction of reflex tachycardia and arterial hypotension). It is recommended not to stop taking bisoprolol in the perioperative period unless clearly necessary (since blockade of beta-adrenergic receptors reduces the risk of arrhythmias and myocardial ischemia during induction of anesthesia and tracheal intubation). If it is necessary to interrupt treatment with bisoprolol before surgery, the drug should be discontinued at least 48 hours before surgery.
Pheochromocytoma
In patients with pheochromocytoma, bisoprolol can only be prescribed while using alpha-blockers.
Thyrotoxicosis
With hyperthyroidism, beta-blockers (including bisoprolol) can mask tachycardia and reduce the severity of symptoms of thyrotoxicosis. Abrupt withdrawal of the drug can cause exacerbation of symptoms of the disease and the development of thyrotoxic crisis.
Hypersensitivity reactions
Beta blockers, including bisoprolol, may increase sensitivity to allergens and the severity of anaphylactic/hypersensitivity reactions due to decreased adrenergic compensatory regulation by beta blockers. The use of usual therapeutic doses of epinephrine (adrenaline) while taking beta-blockers does not always lead to achieving the desired clinical effect. Caution should be exercised when prescribing bisoprolol to patients with a history of severe hypersensitivity reactions or undergoing desensitization.
Psoriasis
When deciding on the use of bisoprolol in patients with psoriasis, the expected benefits of the drug should be carefully weighed against the possible risk of exacerbation of psoriasis.
Contact lenses
Patients who use contact lenses should take into account that the use of beta-blockers may reduce the production of tear fluid.
Effect on the ability to drive vehicles and machinery According to the study results, in patients with coronary artery disease, bisoprolol does not affect the ability to drive vehicles. However, due to individual reactions, the ability to drive a car or operate technically complex mechanisms may be impaired. Particular attention should be paid to this at the beginning of treatment and after changing the dose of bisoprolol.
Active ingredient
Active ingredient
Bisoprolol
Composition
Composition
Active ingredient: bisoprolol fumarate 5 mg;
excipients: microcrystalline cellulose (MCC-102), corn starch, croscarmellose sodium, magnesium stearate, colloidal silicon dioxide; shell composition: Opadry II yellow 85F220023 (polyvinyl alcohol, macrogol, titanium dioxide (E 171), talc, yellow iron oxide dye (E 172), black iron oxide dye (E 172));
Pregnancy
Pregnancy
Pregnancy
The pharmacological effects of bisoprolol can have an adverse effect on the course of pregnancy and the body of the fetus/newborn. In general, beta blockers reduce blood flow to the placenta, which may lead to fetal growth restriction, intrauterine fetal death, or premature birth. The fetus and newborn may develop adverse effects (eg, hypoglycemia and bradycardia). If treatment with beta-blockers is necessary, preference should be given to selective beta1-blockers.
During pregnancy, bisoprolol should be used only if absolutely necessary, if the expected benefit to the mother outweighs the possible risk of side effects in the fetus and/or newborn. Blood flow in the placenta and uterus should be monitored, as well as the growth and development of the unborn child. In the event of adverse events related to pregnancy and/or the fetus, it is recommended to use alternative methods of therapy.
The newborn should be carefully examined after birth. In the first three days of life, the newborn may experience symptoms of bradycardia and hypoglycemia.
Breastfeeding period
According to preclinical studies, bisoprolol and/or its metabolites penetrate into the milk of lactating rats. There is no data on the excretion of bisoprolol into breast milk. Therefore, taking bisoprolol is not recommended for women during breastfeeding. If taking bisoprolol during lactation is necessary, breastfeeding should be discontinued.
Contraindications
Contraindications
hypersensitivity to bisoprolol or to any of the excipients;
acute heart failure;
CHF in the stage of decompensation, requiring intravenous administration of inotropic drugs;
cardiogenic shock;
severe arterial hypotension (systolic blood pressure less than 100 mm Hg);
severe bradycardia (heart rate less than 60 beats/min) before the start of therapy;
AV block II and III degrees in patients without a pacemaker;
sick sinus syndrome;
sinoatrial block;
severe forms of bronchial asthma;
severe peripheral arterial circulation disorders or Raynaud’s syndrome;
pheochromocytoma (without simultaneous use of alpha-blockers);
metabolic acidosis;
age under 18 years (efficacy and safety have not been established).
With caution
AV block of the first degree; vasospastic angina (Prinzmetal’s angina); thyrotoxicosis; type I diabetes mellitus and diabetes mellitus with significant fluctuations in blood glucose concentrations; severe renal failure (creatinine clearance less than 20 ml/min); severe liver dysfunction; psoriasis; restrictive cardiomyopathy; congenital heart defects or heart valve disease with severe hemodynamic disturbances; CHF with myocardial infarction within the last 3 months; mild to moderate peripheral arterial circulation disorders; severe forms of chronic obstructive pulmonary disease (COPD); mild forms of bronchial asthma; bronchospasm (history); allergic reactions (history); carrying out desensitizing therapy; extensive surgical interventions and general anesthesia; strict diet; pregnancy and breastfeeding period.
Side Effects
Side Effects
The frequency of side effects is classified according to the recommendations of the World Health Organization: very common (≥ 1/10), common (≥ 1/100 to
<1/10), uncommon (≥1/1000 to <1/100), rare (≥1/10000 to <1/1000), very rare (<1/10000), frequency unknown (cannot be estimated from available data).
Mental disorders: infrequently – sleep disturbance, depression; rarely – hallucinations, nightmares.
Nervous system disorders: often – dizziness, headache (in patients with arterial hypertension or angina pectoris, these symptoms especially often appear at the beginning of the course of treatment. Usually these phenomena are mild and usually disappear within 1-2 weeks after the start of treatment); rarely – loss of consciousness.
Visual disturbances: rarely – decreased tear production (should be taken into account when wearing contact lenses); very rarely – conjunctivitis.
Hearing disorders and labyrinthine disorders: rarely – hearing impairment. Cardiac disorders: very often – bradycardia (in patients with CHF); often – worsening symptoms of CHF (in patients with CHF); uncommon – AV disorder
conductivity, worsening symptoms of CHF (in patients with hypertension or angina), bradycardia (in patients with hypertension or angina).
Vascular disorders: often – a feeling of coldness or numbness in the extremities, arterial hypotension, especially in patients with heart failure; infrequently – orthostatic hypotension.
Disorders of the respiratory system, chest and mediastinal organs: infrequently – bronchospasm in patients with bronchial asthma or a history of obstructive airway diseases; rarely – allergic rhinitis.
Gastrointestinal disorders: often – nausea, vomiting, diarrhea, constipation.
Disorders of the liver and biliary tract: rarely – hepatitis.
Disorders of the skin and subcutaneous tissues: rarely – hypersensitivity reactions (such as itching, skin hyperemia, skin rash); very rare: alopecia. Beta blockers may cause exacerbation or worsening of psoriasis, or cause psoriasis-like rashes.
Musculoskeletal and connective tissue disorders: uncommon – muscle weakness, cramps.
Disorders of the genital organs and mammary gland: rarely – impaired potency.
General disorders and disorders at the injection site: often – asthenia (in patients with CHF), increased fatigue; uncommon – asthenia (in patients with hypertension or angina pectoris).
Laboratory and instrumental data: rarely – increased activity
“liver” transaminases: aspartate aminotransferase (AST), alanine aminotransferase (ALT) in the blood, increased concentration of triglycerides in the blood.
Interaction
Interaction
Not recommended combinations
Treatment of CHF
Class I antiarrhythmic drugs
Class I antiarrhythmic drugs (for example, quinidine, disopyramide, lidocaine, phenytoin, flecainide, propafenone), when used simultaneously with bisoprolol, can reduce AV conduction and reduce cardiac contractility.
All indications for the use of bisporolol:
Verapamil and diltiazem
Non-dihydropyridine slow calcium channel blockers (SCBCs), such as verapamil and, to a lesser extent, diltiazem, when used simultaneously with bisoprolol, can lead to a decrease in myocardial contractility and impaired AV conduction, cardiac arrest and heart failure. In particular, intravenous administration of verapamil to patients taking beta-blockers can lead to severe arterial hypotension and AV block.
Centrally acting antihypertensives
The simultaneous use of bisoprolol with centrally acting antihypertensive drugs (such as clonidine, methyldopa, moxonidine, rilmenidine) can lead to a worsening of heart failure due to a decrease in central sympathetic tone (decreased heart rate, decreased cardiac output, peripheral vasodilation).
Abrupt withdrawal of centrally acting antihypertensive drugs, especially before discontinuation of beta-blockers, may increase the risk of developing rebound hypertension (withdrawal syndrome). In patients taking bisoprolol and clonidine concomitantly, if it is necessary to discontinue therapy, bisoprolol should be discontinued several days before stopping clonidine. If clonidine is to be replaced with bisoprolol, a beta-blocker should be prescribed a few days after clonidine is discontinued.
Methyldopa increases the risk of developing or worsening bradycardia, AV block, cardiac arrest, and heart failure.
Fingolimod
Fingolimod may enhance the negative chronotropic effect of beta-blockers and lead to severe bradycardia. Concomitant use of fingolimod and bisoprolol is not recommended. If it is necessary to use these drugs simultaneously, careful monitoring of the patient’s condition is required. It is recommended that combination therapy be initiated in a hospital setting and appropriate monitoring be carried out (long-term heart rate monitoring is indicated, at least until the morning of the next day after the first simultaneous administration of fingolimod and a beta-blocker).
Combinations requiring special care
Treatment of arterial hypertension and stable angina:
Class I antiarrhythmic drugs
Class I antiarrhythmic drugs (for example, quinidine, disopyramide, lidocaine, phenytoin, flecainide, propafenone), when used simultaneously with bisoprolol, can slow AV conduction and reduce cardiac contractility.
All indications for the use of bisoprolol:
Class III antiarrhythmic drugs
Class III antiarrhythmic drugs (eg, amiodarone) may worsen AV conduction disturbances. Amiodarone and other antiarrhythmic drugs increase the risk of developing or worsening bradycardia, cardiac arrest, and heart failure.
Blockers of “slow” calcium channels (SCBC) – dihydropyridine derivatives CMCC – dihydropyridine derivatives (for example, nifedipine, felodipine, amlodipine), when used simultaneously with bisoprolol, may increase the risk of developing arterial hypotension. In patients with CHF, the risk of further deterioration of cardiac contractile function cannot be excluded. Nifedipine can lead to a significant decrease in blood pressure.
Drugs that lower blood pressure
Antihypertensive drugs (diuretics, clonidine, etc.), as well as other drugs with a possible antihypertensive effect (for example, tricyclic antidepressants, barbiturates, phenothiazines) can enhance the antihypertensive effect of bisoprolol and lead to an excessive decrease in blood pressure.
Beta-blockers for local use
The effect of topical beta-blockers (for example, eye drops for the treatment of glaucoma) may enhance the systemic effects of bisoprolol (lowering blood pressure, lowering heart rate).
Cholinomimetics
Cholinomimetics (parasympathomimetics), when used simultaneously with bisoprolol, may increase AV conduction disturbances and increase the risk of developing bradycardia.
Hypoglycemic drugs
The hypoglycemic effect of insulin or oral hypoglycemic agents may be enhanced. Signs of hypoglycemia – in particular tachycardia – may be masked or suppressed. Such interactions are more likely when using non-selective beta-blockers.
Means for general anesthesia
Inhalational anesthetics may increase the risk of cardiodepressive effects. There is a decrease in reflex tachycardia, an increase in the risk of bradyarrhythmias and severe arterial hypotension.
Cardiac glycosides
Cardiac glycosides, when used simultaneously with bisoprolol, can lead to an increase in impulse conduction time, and thus to the development of bradycardia.
Cardiac glycosides increase the risk of AV block, cardiac arrest and heart failure.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs may reduce the antihypertensive effect of bisoprolol (via sodium retention and blockade of renal prostaglandin synthesis).
Sympathomimetics
Concomitant use of bisoprolol with beta-agonists (such as isoprenaline or dobutamine) may lead to a decrease in the effect of both drugs.
Concomitant use of bisoprolol with beta- and alpha-adrenergic agonists (such as epinephrine [adrenaline]) may enhance the vasoconstrictor effects resulting from alpha-adrenergic receptor stimulation and lead to the development of hypertension or worsening intermittent claudication. Such interactions are more likely when using non-selective beta-blockers.
Cases of the development of severe arterial hypertension have been described with the simultaneous use of beta-blockers with alpha-agonists, including drugs for topical use (for example, decongestants in the form of nasal drops).
Combinations to consider Mefloquine
Mefloquine, when used concomitantly with bisoprolol, may increase the risk of bradycardia.
Monoamine oxidase inhibitors (MAO)
MAO inhibitors (except MAO B inhibitors) may enhance the antihypertensive effect of beta-blockers. Concomitant use may also lead to the development of a hypertensive crisis. The break in treatment between the discontinuation of MAO inhibitors and the prescription of bisoprolol should be at least 14 days. Ergot alkaloids
Non-hydrogenated ergot alkaloids increase the risk of developing peripheral circulatory disorders when taking beta-blockers. Ergotamine increases the risk of developing peripheral circulatory disorders.
Pharmacokinetic interactions
Rifampicin increases metabolic clearance and shortens T1/2 of bisoprolol. Usually no dose adjustment is required.
Caution should be exercised when using bisoprolol simultaneously with inducers of liver microsomal oxidation isoenzymes.
It is possible to increase the concentration of bisoprolol in the blood plasma when used simultaneously with inhibitors of the CYP3A4 isoenzyme and reduce it when used simultaneously with inducers of CYP3A4. Bisoprolol may increase the plasma concentration of drugs metabolized by the isoenzyme CYP3A4 and possibly CYP2D6.
Pharmacokinetic studies did not reveal interactions of bisoprolol with thiazide diuretics, digoxin and cimetidine. Bisoprolol does not affect prothrombin time in patients receiving a stable dose of warfarin.
Overdose
Overdose
Symptoms: arrhythmia, ventricular extrasystole, severe bradycardia, AV block, marked decrease in blood pressure, acute heart failure, hypoglycemia, acrocyanosis, difficulty breathing, bronchospasm, dizziness, fainting, convulsions.
Sensitivity to a single high dose of bisoprolol varies widely among individual patients and patients with CHF are likely to be highly sensitive.
Treatment: if an overdose occurs, first of all you need to stop taking the drug, perform gastric lavage, prescribe adsorbents, and carry out symptomatic therapy.
For severe bradycardia, intravenous administration of atropine. If the effect is insufficient, a drug with a positive chronotropic effect can be administered with caution. Sometimes a temporary pacemaker may be needed.
With a pronounced decrease in blood pressure, intravenous administration of plasma-substituting solutions and vasopressors. Intravenous glucagon may be effective.
For hypoglycemia, intravenous dextrose (glucose) may be indicated. For AV block: Patients should be closely monitored and treated with beta-agonists such as epinephrine. If necessary, install a pacemaker.
In case of exacerbation of CHF, intravenous administration of diuretics, drugs with a positive inotropic effect, as well as vasodilators.
For bronchospasm, prescribe bronchodilators, including beta2-adrenergic agonists and/or aminophylline.
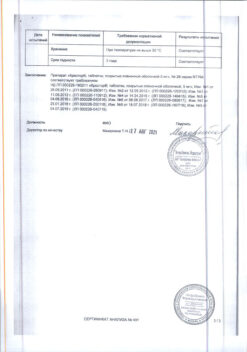
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25 ° C. Keep out of the reach of children.
Shelf life
Shelf life
2 years. Do not use after expiration date.
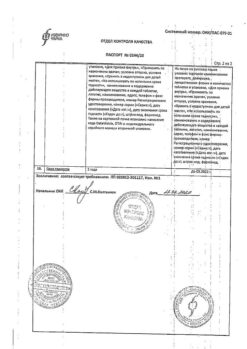
Manufacturer
Manufacturer
Rapharma JSC, Russia
Additional information
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store in a light-protected place at a temperature not exceeding 25 °С. Keep out of reach of children. |
| Manufacturer | Rapharma AO, Russia |
| Medication form | pills |
| Brand | Rapharma AO |
Other forms…
Related products
Buy Bisoprolol, 5 mg 50 pcs. with delivery to USA, UK, Europe and over 120 other countries.