No products in the cart.
Bicillin-3, 1200000 units 10 ml
€6.51 €5.79
Description
Pharmacotherapeutic group: biosynthetic penicillin antibiotic
ATX code: [J01SE30]
Pharmacokinetics
After intramuscular administration, it is slowly absorbed with release from the benzylpenicillin depot. When administered once, it persists at an average therapeutic concentration for 6-7 days. Time required to reach maximum concentration (TCmax) in plasma is 12-24 hours after injection. On the 14th day after 2.4 million units have been injected, serum concentrations are 0.12 µg/ml; on the 21st day after 1.2 million units have reached 0.06 µg/ml (1 unit = 0.6 µg). Fluid penetration is high, tissue penetration is low. Binding with plasma proteins is 40-60%. It penetrates through the placental barrier and is detected in the mother’s milk. It is metabolized insignificantly, it is excreted mainly by kidneys unchanged.
Pharmacodynamics
A combined bactericidal drug of 3 ‑salts of benzylpenicillin: dibenzyl-ethylenediamine, procaine, sodium, having a long action. It suppresses the synthesis of the cell wall of microorganisms.
It is active against Gram-positive microorganisms:
Staphylococcus spp. (non-penicillinase forming), Streptococcus spp, including Streptococcus pneumoniae, Corynebacterium diphtheriae;
Anaerobic spore-forming bacilli:
Bacillus anthracis, Clostridium spp, Actinomyces israelii;
Gram-negative microorganisms:
Neisseria gonorrhoeae, Neisseria meningitidis, Treponema spp.
Penicillinase-producing strains of Staphylococcus spp. are resistant to the drug.
Indications
Indications
Infections (in adults) caused by sensitive microorganisms: syphilis and other diseases caused by Treponema pallidum (yaws), streptococcal infections (excluding infections caused by group B streptococci) – acute tonsillitis, scarlet fever, erysipelas; prevention of rheumatism.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: biosynthetic antibiotic penicillin
ATX code: [J01CE30]
Pharmacokinetics
After intramuscular administration, it is slowly absorbed with the release of benzylpenicillin from the depot. With a single administration, it remains in an average therapeutic concentration for 6–7 days. The time required to achieve maximum concentration (TCmax) in plasma is 12–24 hours after injection. On the 14th day after administration of 2.4 million units, the concentration in the blood serum is 0.12 mcg/ml; on day 21 after administration of 1.2 million units – 0.06 mcg/ml (1 unit = 0.6 mcg). Penetration into liquids is high, into tissues – low. Bonding with plasma proteins is 40–60%. Penetrates the placental barrier and is found in mother’s milk. Metabolized slightly, excreted mainly by the kidneys unchanged.
Pharmacodynamics
A combined bactericidal preparation of 3 benzylpenicillin salts: dibenzyl-ethylenediamine, procaine, sodium, which have a long-lasting effect. Suppresses the synthesis of the cell wall of microorganisms.
Active against gram-positive microorganisms:
Staphylococcus spp. (non-penicillinase-forming), Streptococcus spp., including Streptococcus pneumoniae, Corynebacterium diphtheriae;
Anaerobic spore-forming rods:
Bacillus anthracis, Clostridium spp., Actinomyces israelii;
Gram-negative microorganisms:
Neisseria gonorrhoeae, Neisseria meningitidis, Treponema spp.
Staphylococcus spp. strains that produce penicillinase are resistant to the drug.
Special instructions
Special instructions
The drug should not be administered into tissues with reduced blood supply. Before starting therapy, a thorough history should be taken to determine possible sensitization to penicillins and/or other beta-lactam antibiotics. When treated with the drug, severe (up to the development of anaphylactic shock) and sometimes fatal allergic reactions may occur. The patient should be informed about possible allergy symptoms and the need to immediately inform the doctor about their occurrence. If allergic reactions occur, treatment with the drug should be stopped immediately and, if necessary, symptomatic therapy should be prescribed.
In 5–10% of cases, allergic reactions to penicillin can be cross-reactions with allergic reactions to cephalosporins. In this regard, if there is a history of allergic reactions to cephalosporins, the use of penicillins is contraindicated.
Particular caution should be exercised in the following patient groups:
– Patients with bronchial asthma, allergic skin rashes have an increased risk of hypersensitivity reactions. Such patients should remain under medical supervision for at least 30 minutes after injection. If allergic reactions occur, the drug should be discontinued; if necessary, symptomatic and/or anti-shock therapy is indicated;
– Patients with renal and/or liver failure (see also section “Method of administration and dosage”);
– Patients with concomitant dermatomycosis (possible development of paraallergic reactions).
As a general principle, patients susceptible to developing hypersensitivity reactions should, if possible, be under medical observation for at least half an hour after administration of the antibiotic, since severe immediate hypersensitivity reactions can occur even after the first administration of the drug.
During the treatment of syphilis, due to massive lysis of bacteria and the release of endotoxins, the Jarisch-Herxheimer reaction (fever, chills, other general and local symptoms) may develop.
2–12 hours after administration of the drug, headache, sweating, chills, myalgia, arthralgia, nausea, tachycardia, an increase and subsequent decrease in blood pressure may occur.
These symptoms disappear within 10–12 hours.
The patient should be informed that these reactions are common transient complications of antibiotic treatment. If a Jarisch-Herxheimer reaction occurs, appropriate symptomatic therapy should be administered to eliminate or reduce the severity of its symptoms.
In patients with diabetes mellitus, due to impaired peripheral circulation, the absorption of the drug into the systemic circulation may slow down. The drug should not be administered into tissues with impaired perfusion.
It cannot be administered subcutaneously, intravenously, endolumbarally, or into body cavities.
Renal function and peripheral blood patterns should be periodically monitored during long-term use of the drug (more than 5 days).
In case of accidental subcutaneous injection, a painful lump may occur at the injection site. The pain may be relieved by applying ice to the injection site.
With accidental intravascular administration of the drug, a transient feeling of anxiety and visual disturbances (Hoyne’s syndrome) may occur.
Symptoms usually go away within an hour. If symptoms are severe, sedatives may be required.
With the use of the drug, the development of Nicolau syndrome, acute drug-induced embolism of skin vessels, is possible. Nicolau syndrome is a rare complication that occurs during intramuscular administration of drugs, the manifestations of which include necrosis of the skin and/or underlying tissues of varying severity. With accidental intra-arterial administration of the drug, serious complications can occur, such as arterial thrombosis and tissue necrosis (gangrene). The initial manifestations of these complications may be pale “spots” on the skin of the buttock area. As a result of high pressure at the injection site, retrograde reflux of the drug into the common iliac artery, aorta or spinal arteries may occur.
In order to avoid accidental intravascular injection of the drug, it is recommended to perform aspiration before performing an intramuscular injection in order to identify a possible needle entry into the vessel.
Rubbing the buttock after the injection is not recommended.
Repeated injections into the same area of muscle tissue during long-term treatment with depot penicillins (for example, treatment of syphilis) can lead to damage to this area of tissue and a local increase in vascularization. Subsequent injections increase the likelihood of the injected substance entering the bloodstream directly by direct injection into a blood vessel due to increased pressure during administration or due to “rubbing” of the site where the drug depot was created.
For long-term treatment, it is recommended to select the site for the next injection at a considerable distance from the site of the previous injection.
When treating sexually transmitted diseases, if syphilis is suspected, dark-field microscopy should be performed before starting therapy and then serological tests should be performed within 4 months. In cases of congenital syphilis, cerebrospinal fluid (CSF) should also be examined.
If central nervous system involvement (neurosyphilis) cannot be excluded, other penicillin preparations that penetrate better into the CSF should be used.
In severe purulent-inflammatory diseases (severe pneumonia, empyema, sepsis, meningitis, peritonitis), drugs are required that create a higher concentration of benzylpenicillin in the blood plasma. Water-soluble salts of the drug should be used.
If severe, persistent diarrhea occurs, pseudomembranous colitis should be suspected (possible symptoms include watery stools with blood/mucus, tenesmus, diffuse cramping abdominal pain, fever). This condition can be life-threatening, drug therapy should be immediately discontinued, and appropriate therapy should be prescribed based on the sensitivity of the identified pathogen (for example, vancomycin 250 mg orally 4 times a day). Drugs that inhibit intestinal motility are contraindicated.
Due to the possibility of the development of fungal infections, it is advisable to use B vitamins and vitamin C when treating with benzylpenicillin. In case of suspicion of the development of a fungal infection, the use of antifungal drugs is indicated.
It must be taken into account that using the drug in insufficient doses or stopping treatment too early often leads to the emergence of resistant strains of pathogens. The possibility of the emergence of resistant strains of pathogens should be taken into account during long-term treatment. In case of secondary infections (superinfections), appropriate measures should be taken.
Impact on the results of diagnostic laboratory tests
– Patients receiving benzylpenicillin have a positive direct Coombs test. After discontinuation of penicillin, the direct antiglobulin test may remain positive for 6–8 weeks.
– Determination of urine proteins using precipitate methods (sulfosalicylic acid, trichloroacetic acid), the Folin-Ciocalteu method or the biuret method may lead to false-positive results. Thus, protein in urine must be determined by other methods.
– Determination of amino acids in urine using the ninhydrin method may also lead to false-positive results.
– Penicillins bind to albumin. During electrophoresis, erroneous bisalbuminemia may be observed when determining albumin content.
– During benzylpenicillin therapy, non-enzymatic determination of glucose and urobilinogen in urine may lead to false-positive results.
– During treatment with benzylpenicillin, increased values of 17-ketosteroids (using the Zimmermann reaction) in the urine may be observed.
– Use the drug with caution in patients with impaired renal excretory function, since there is a risk of hyponatremia. When using the drug, it is recommended to monitor renal function.
The sodium content in a single dose of the drug for a dosage of 600,000 units is 7.73 mg or 0.336 mmol, for a dosage of 1,200,000 units is 15.46 mg or 0.672 mmol.
Impact on the ability to drive vehicles and machinery
During the treatment period, care should be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Benzathine benzylpenicillin, Benzylpenicillin procaine, Benzylpenicillin
Composition
Composition
For 1 bottle:
Active ingredients:
Benzathine benzylpenicillin – 400,000 units,
benzylpenicillin sodium (benzylpenicillin sodium salt) – 400,000 units,
benzylpenicillin procaine (benzylpenicillin novocaine salt) – 400,000 units.
Pregnancy
Pregnancy
Use during pregnancy is possible only when the expected benefit to the mother outweighs the potential risk to the fetus.
If it is necessary to use the drug during lactation, the issue of stopping breastfeeding should be decided.
Contraindications
Contraindications
Hypersensitivity to drugs of the penicillin group and other beta-lactam antibiotics, to procaine, children under 18 years of age.
With caution
Pregnancy, breastfeeding, renal failure, allergic diseases, including bronchial asthma, hay fever (including history), pseudomembranous colitis.
Side Effects
Side Effects
Infections and infestations
With long-term therapy, superinfection with resistant microorganisms and fungi occurs.
Blood and lymphatic system disorders: hemolytic anemia, anemia, thrombocytopenia, leukopenia, hypocoagulation.
Immune system disorders: anaphylactic shock, Jarisch-Herxheimer reaction, anaphylactoid reactions (asthmatic attack, purpura, gastrointestinal symptoms).
Mental disorders: Hoyne’s syndrome (acute penicillin psychotic syndrome).
Nervous system disorders: neuropathy.
Gastrointestinal disorders: stomatitis, glossitis, diarrhea, vomiting, pseudomembranous colitis.
Disorders of the liver and biliary tract: hepatitis, cholestasis.
Disorders of the skin and subcutaneous tissue: urticaria, angioedema, exudative erythema multiforme, exfoliative dermatitis; in patients with concomitant ringworm, paraallergic reactions may develop (due to the similarity of penicillin antigens and dermatophyte metabolites), Stevens-Johnson syndrome, Lyell’s syndrome.
Muscular, skeletal and connective tissue disorders: arthralgia, joint pain.
Renal and urinary tract disorders: nephropathy, interstitial nephritis.
General disorders and reactions at the injection site: fever, pain at the injection site, infiltrates at the injection site, Nicolau syndrome (acute drug-induced embolism of skin vessels).
Laboratory and instrumental data: positive direct Coombs test, moderate transient increase in the activity of serum transaminases.
Interaction
Interaction
Concomitant use is not recommended
Since penicillin derivatives act only on dividing microbial cells, the drug should not be combined with bacteriostatic antibacterial drugs (for example, macrolides, chloramphenicol, lincosamides, tetracyclines). Combinations with other antibacterial drugs are possible only if a synergistic, or at least additive effect of the drug combination can be expected.
To avoid unwanted pharmaceutical interactions, the drug should not be administered in the same syringe with other medications.
Combinations to use with caution
When used simultaneously with non-steroidal anti-inflammatory drugs (indomethacin, phenylbutazone, salicylates), probenecid, allopurinol, the possibility of competitive inhibition of drug excretion from the body should be taken into account.
The use of probenecid leads to inhibition of the tubular secretion of benzylpenicillin, resulting in an increase in the concentration of the drug in the blood serum and its half-life.
In addition, probenecid inhibits the transport of penicillin from the cerebrospinal fluid, so simultaneous administration of probenecid further reduces the penetration of benzylpenicillin into brain tissue.
Concomitant use with oral anticoagulants may enhance their properties (as vitamin K antagonists) and increase the risk of bleeding. Frequent monitoring of the international normalized ratio (INR) is recommended, and the dose of the vitamin K antagonist should be adjusted both during and after the end of treatment with the drug.
When used together with digoxin, the risk of developing bradycardia increases significantly.
Reduces the excretion of methotrexate, which may result in increased toxicity.
Overdose
Overdose
At very high doses, penicillins can cause the development of encephalopathy (impaired consciousness, movement disorders, convulsions). If an overdose is suspected, monitoring the patient’s condition and symptomatic therapy is required.
Storage conditions
Storage conditions
In a dry place at a temperature of 8 to 15 °C.
Shelf life
Shelf life
3 years.
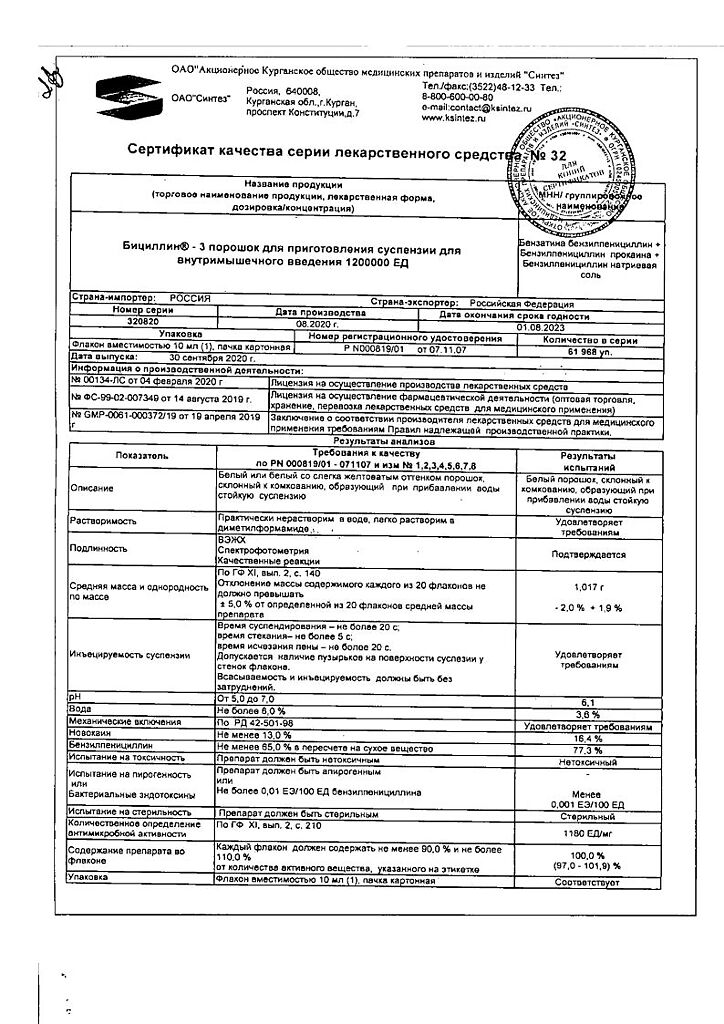
Manufacturer
Manufacturer
Sintez, Russia
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | In a dry place at a temperature of 8 to 15 ° C. |
| Manufacturer | Sintez OAO, Russia |
| Medication form | Powder for preparation of solution |
| Brand | Sintez OAO |
Related products
Buy Bicillin-3, 1200000 units 10 ml with delivery to USA, UK, Europe and over 120 other countries.