No products in the cart.
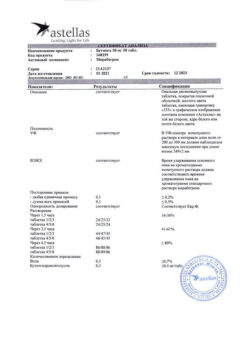
Betmiga, 50 mg 10 pcs
€22.52 €18.77
Description
A selective β3-adrenoreceptor agonist. Studies with mirabegron demonstrated relaxation of bladder smooth muscles in rats and in an isolated preparation of human tissues, as well as an increase in the concentration of cAMP in the bladder tissue in rats. Thus, mirabegron improves the reservoir function of the bladder by stimulating β3-adrenoreceptors located in its wall.
Studies have demonstrated the efficacy of mirabegron both in patients previously treated with m-cholinoblockers for the treatment of overactive bladder (UBG) and in patients without a history of prior therapy with m-cholinoblockers.
Mirabegron has also been effective in patients with UBG who have stopped treatment with m-cholinoblockers due to lack of effect.
A 12-week study in men with lower urinary tract symptoms (LUTs) and infravesical obstruction (IVO) demonstrated the safety and good tolerability of mirabegron at doses of 50 and 100 mg once daily, as well as no effect of mirabegron on cystometric parameters.
Changes in pulse rate and BP during treatment are reversible and disappear after discontinuation.
Pharmacokinetics
After oral administration mirabegron is absorbed into the bloodstream and reaches Cmax in plasma between three and four hours after administration. Studies have shown an increase in absolute bioavailability from 29% to 35% after increasing the dose from 25 to 50 mg.
The mean Cmax value and AUC value increased more than proportionally to the dose. Css is reached after 7 days of taking mirabegron once daily. The plasma Css of mirabegron is approximately 2 times greater after multiple doses of once daily.
Mirabegron is intensively distributed in the body. Vd under stable conditions (Vss) is approximately 1670 l. Mirabegron binds (approximately 71%) to plasma proteins and also exhibits moderate affinity to albumin and alpha-1 acidic glycoprotein.
Mirabegron distributes to erythrocytes. Concentrations of 14C mirabegron in erythrocytes were 2 times higher than in plasma (as shown by in vitro studies).
There are many pathways for metabolism of mirabegron in the body, including dealkylation, oxidation, (direct) glucuronidation and amide hydrolysis. After a single administration of C-mirabegron, the main circulating component is mirabegron.
Two major metabolites of mirabegron were detected in human plasma: both are glucuronides (phase II metabolites) and constitute, respectively, 16% and 11% of the total drug concentration. These metabolites have no pharmacological activity.
Despite the participation of the CYP2D6 and CYP3A4 isoenzymes in the oxidative metabolic pathway of mirabegron under in vitro conditions, under in vivo conditions the role of these isoenzymes in total elimination is small.
Total plasma clearance is approximately 57 L/h. The final T1/2 is approximately 50 hr. Renal clearance is approximately 13 l/h, which corresponds to almost 25% of the total clearance. The main mechanisms of excretion by the kidneys are active tubular secretion and glomerular filtration.
The amount of unchanged mirabegron excreted in the urine is dose-dependent and ranges from 6.0% after a daily dose of 25 mg to 12.2% after a daily dose of 100 mg. After administration of 160 mg of C-mirabegron by healthy volunteers, approximately 55% of the radiolabel was detected in the urine and 34% in the feces. The fraction of unchanged mirabegron was approximately 45% of the total isotope-labeled drug in the urine, indicating the presence of metabolites. Most of the isotope-labeled drug in feces was unchanged mirabegron.
Indications
Indications
Overactive bladder (OAB) with symptoms of urinary incontinence, frequent urination and urinary urgency.
Pharmacological effect
Pharmacological effect
Selective agonist of β3-adrenergic receptors. Studies with mirabegron have demonstrated relaxation of bladder smooth muscle in rats and in isolated human tissue, as well as an increase in cAMP concentrations in bladder tissue in rats. Thus, mirabegron improves the reservoir function of the bladder by stimulating β3-adrenergic receptors located in its wall.
Studies have demonstrated the effectiveness of mirabegron both in patients who have previously received anticholinergic drugs for the treatment of overactive bladder (OAB), and in patients without a history of previous anticholinergic therapy.
Mirabegron was also effective in patients with OAB who discontinued treatment with anticholinergic drugs due to lack of effect.
A 12-week study in men with lower urinary tract symptoms (LUTS) and bladder outlet obstruction (IVO) demonstrated the safety and good tolerability of mirabegron in doses of 50 and 100 mg once a day, as well as the absence of mirabegron’s effect on cystometric parameters.
Changes in heart rate and blood pressure during treatment are reversible and disappear after treatment is discontinued.
Pharmacokinetics
Following oral administration, mirabegron is absorbed into the bloodstream and reaches Cmax in plasma between three and four hours after administration. Studies have shown an increase in absolute bioavailability from 29% to 35% after increasing the dose from 25 to 50 mg.
In this case, the average Cmax value and AUC value increased more than proportionally to the dose. Css is achieved after 7 days of taking mirabegron once a day. After repeated use once a day, the Css of mirabegron in the blood plasma are approximately 2 times higher than those after a single dose of the drug.
Mirabegron is intensively distributed in the body. Vd in stable conditions (Vss) is approximately 1670 l. Mirabegron is approximately 71% protein bound in plasma and also exhibits moderate affinity for albumin and alpha-1 acid glycoprotein.
Mirabegron is distributed to red blood cells. Concentrations of 14C-mirabegron in erythrocytes were 2 times higher than in plasma (as shown by in vitro studies).
There are many ways mirabegron is metabolized in the body, incl. dealkylation, oxidation, (direct) glucuronidation and amide hydrolysis. After a single administration of C-mirabegron, the main circulating component is mirabegron.
Two main metabolites of mirabegron were found in human plasma: both are glucuronides (phase II metabolites) and constitute, respectively, 16% and 11% of the total drug concentration. These metabolites do not have pharmacological activity.
Despite the participation of the CYP2D6 and CYP3A4 isoenzymes in the oxidative pathway of mirabegron metabolism in vitro, in in vivo conditions the role of these isoenzymes in the overall elimination is small.
The total plasma clearance is about 57 l/h. The final T1/2 is approximately 50 hours. Renal clearance is approximately 13 l/h, which corresponds to almost 25% of the total clearance. The main mechanisms of excretion by the kidneys are active tubular secretion and glomerular filtration.
The amount of unchanged mirabegron excreted in the urine is dose-dependent and varies from 6.0% after taking the drug at a daily dose of 25 mg to 12.2% after taking a daily dose of 100 mg. After administration of 160 mg of C-mirabegron to healthy volunteers, approximately 55% of the radiolabel was detected in urine and 34% in feces. The unchanged mirabegron fraction accounted for approximately 45% of the total isotopically labeled drug in urine, indicating the presence of metabolites. Most of the isotopically labeled drug in the feces was represented by unchanged mirabegron.
Special instructions
Special instructions
Mirabegron at therapeutic doses did not demonstrate clinically significant prolongation of the QT interval in the studies performed.
However, since patients taking drugs that may cause QT prolongation did not participate in these studies with mirabegron, the effect on these patients is not known. This category of patients should take mirabegron with caution.
Mirabegron should be used with caution in combination with drugs that have a narrow therapeutic index and drugs that are significantly metabolized by CYP2D6, such as thioridazine, drugs for the treatment of class 1 C arrhythmias (for example, flecainide, propafenone) and tricyclic antidepressants (for example, imipramine, desipramine).
Mirabegron should also be taken with caution when co-administered with drugs that are metabolized by the CYP2D6 isoenzyme and the dose of which must be individually determined.
During post-marketing surveillance of the use of mirabegron in patients with bladder outlet obstruction (VFO) and in patients already taking anticholinergic drugs for the treatment of OAB, cases of urinary retention were observed. A controlled clinical safety study in patients with IFO did not find an increase in urinary retention in patients receiving mirabegron; however, mirabegron should be used with caution in patients with clinically significant IFO.
Mirabegron should also be used with caution in patients already taking anticholinergic drugs for the treatment of OAB.
Mirabegron may increase blood pressure. It is recommended to measure blood pressure before starting treatment and periodically during treatment with mirabegron, especially in patients with arterial hypertension.
Active ingredient
Active ingredient
Mirabegron
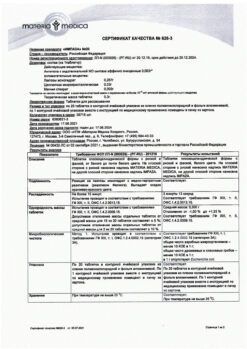
Composition
Composition
1 tab.:
– mirabegron 25 mg, 50 mg
excipients:
macrogoal 2000000,
macrogol 8000,
hydroxypropylcellulose,
butylated hydroxytoluene,
purified water
magnesium stearate
tablet shell composition:
Opadry 03F43159 (hypromellose 2910 6 mPa-s, macrogol 8000, iron oxide yellow (E172), iron oxide red (E172)), Opadry 03F42192 (hypromellose 2910 6 mPa-s, macrogol 8000, iron oxide yellow (E172)).
Pregnancy
Pregnancy
Pregnancy
There is limited data on the use of mirabegron in pregnant women. Animal studies have shown reproductive toxicity. Mirabegron is not recommended during pregnancy or in women of childbearing age who are not using contraception.
Breastfeeding period
In rodents, mirabegron is excreted in breast milk; therefore, in humans there is also a risk of the drug passing into breast milk. There are no studies examining the effect of mirabegron on breast milk production, the excretion of mirabegron in breast milk and the effect on the child. Mirabegron should not be used in women during breastfeeding.
Fertility
Animal studies have not shown any effect of mirabegron on fertility at non-lethal doses.
It has not been established whether mirabegron affects fertility in humans.
Contraindications
Contraindications
End-stage renal failure (eGFR < 15 ml/min/1.73 m2 or patients for whom hemodialysis is indicated); severe renal failure (eGFR 15-29 ml/min/1.73 m2) with simultaneous use of strong inhibitors of the CYP3A isoenzyme; severe stage of liver failure (class C on the Child-Pugh scale); severe uncontrolled hypertension, defined as systolic blood pressure ≥180 mm Hg. and/or diastolic blood pressure ≥110 mmHg; moderate stage of liver failure (class B on the Child-Pugh scale) with simultaneous use of strong inhibitors of the CYP3A isoenzyme; children's age (lack of data on effectiveness and safety); pregnancy and breastfeeding; hypersensitivity to the active substance.
Side Effects
Side Effects
Infections and infestations: often – urinary tract infection; uncommon – vaginal infection, cystitis.
From the organ of vision: rarely – swelling of the eyelids.
From the cardiovascular system: often – tachycardia; uncommon – rapid heartbeat, atrial fibrillation, increased blood pressure
From the digestive system: often – nausea; infrequently – dyspepsia, gastritis, increased activity of GGT, AST, ALT; rarely – swelling of the lips.
From the skin and subcutaneous tissue: uncommon – urticaria, rash, macular rash, papular rash, itching; rarely – leukocystoclastic vasculitis, purpura, angioedema.
From the musculoskeletal system: infrequently – swelling of the joints.
From the reproductive system: infrequently – vulvovaginal itching
*Detected during post-marketing use
Interaction
Interaction
Mirabegron is a moderate, time-dependent inhibitor of CYP2D6 and a weak inhibitor of CYP3A. At high concentrations, mirabegron inhibited the transport of drugs carried out by P-glycoprotein.
Clinically significant interactions between mirabegron and drugs that inhibit, activate or are a substrate of one of the CYP isoenzymes or transporters are not expected, with the exception of the inhibitory effect of mirabegron on the metabolism of CYP2D6 isoenzyme substrates.
Mirabegron concentration (AUC) increased 1.8-fold under the influence of the strong CYP3A/P-gp inhibitor ketoconazole in healthy volunteers. Dose adjustment of mirabegron is not required when taken together with inhibitors of the CYP3A or P-gp isoenzyme.
However, in patients suffering from mild to moderate renal impairment (eGFR 30-89 ml/min/1.73 m2) or mild hepatic impairment (Child-Pugh class A) taking strong CYP3A inhibitors such as itraconazole, ketoconazole, ritonavir and clarithromycin, the recommended daily dose of mirabegron is 25 mg, regardless of dose food.
Substances that induce CYP3A or P-gp isoenzymes reduce the plasma concentration of mirabegron.
In healthy volunteers, mirabegron moderately inhibits the CYP2D6 isoenzyme, the activity of which is restored 15 days after discontinuation of mirabegron.
Daily dosing of mirabegron resulted in a 90% increase in Cmax and 229% increase in AUC for a single dose of metoprolol.
Daily dosing of mirabegron resulted in a 79% increase in Cmax and 241% increase in AUC for a single dose of desipramine. Mirabegron should be used with caution in combination with drugs that have a narrow therapeutic index and drugs that are significantly metabolized by the CYP2D6 isoenzyme, for example, thioridazine, drugs for the treatment of class I C arrhythmias (for example, flecainide, propafenone) and tricyclic antidepressants (for example, imipramine, desipramine).
Mirabegron should also be taken with caution when taken together with drugs that are metabolized by the CYP2D6 isoenzyme and the dose of which must be individually determined.
Mirabegron is a weak inhibitor of the P-gp protein. Mirabegron increased Cmax and AUC by 29% and 27%, respectively, when administered with digoxin to healthy volunteers.
For patients starting to take mirabegron and digoxin at the same time, digoxin should be taken at the lowest dose. In this case, it is necessary to monitor the concentrations of digoxin in the blood plasma and select a further effective dose of digoxin based on the results of control tests.
The potential for P-gp inhibition by mirabegron should be taken into account when administering mirabegron with drugs transported by P-gp proteins, such as dabigatran.
The increased effect of mirabegron when taken together with other drugs is expressed in an increase in heart rate.
Overdose
Overdose
Symptoms:
Doses up to 400 mg have been used in single doses of mirabegron to healthy volunteers. When using this dose level, adverse events were recorded in the form of rapid heartbeat (in 1 out of 6 volunteers) and an increase in heart rate of more than 100 beats/min (in 3 out of 6 volunteers).
With repeated (over 10 days) use of the drug in daily doses of up to 300 mg, an increase in heart rate and an increase in systolic blood pressure were recorded in healthy volunteers.
Treatment:
symptomatic and supportive therapy. Monitoring of pulse rate, blood pressure and ECG is necessary.
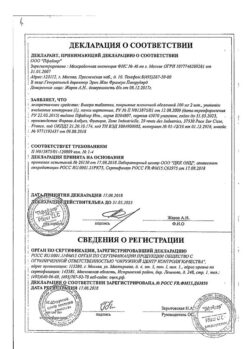
Manufacturer
Manufacturer
Avara Pharmaceutical Technologies Inc., USA
Additional information
| Manufacturer | Avara Pharmaceutical Technologies Inc, USA |
|---|---|
| Medication form | slow-release tablets |
| Brand | Avara Pharmaceutical Technologies Inc |
Other forms…
Related products
Buy Betmiga, 50 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.