No products in the cart.
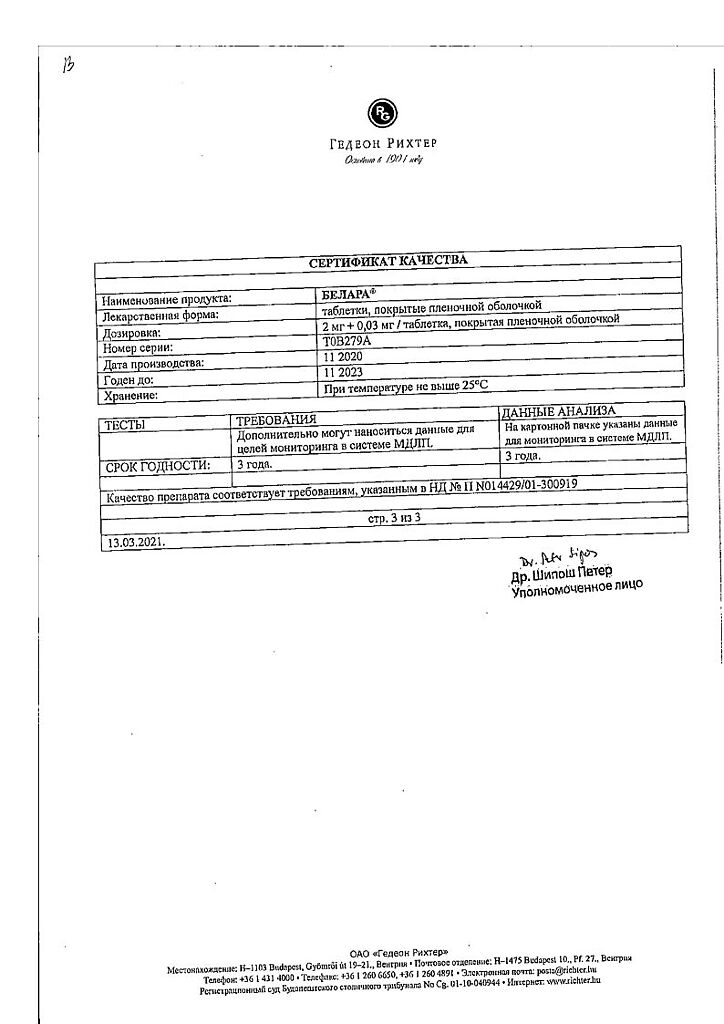
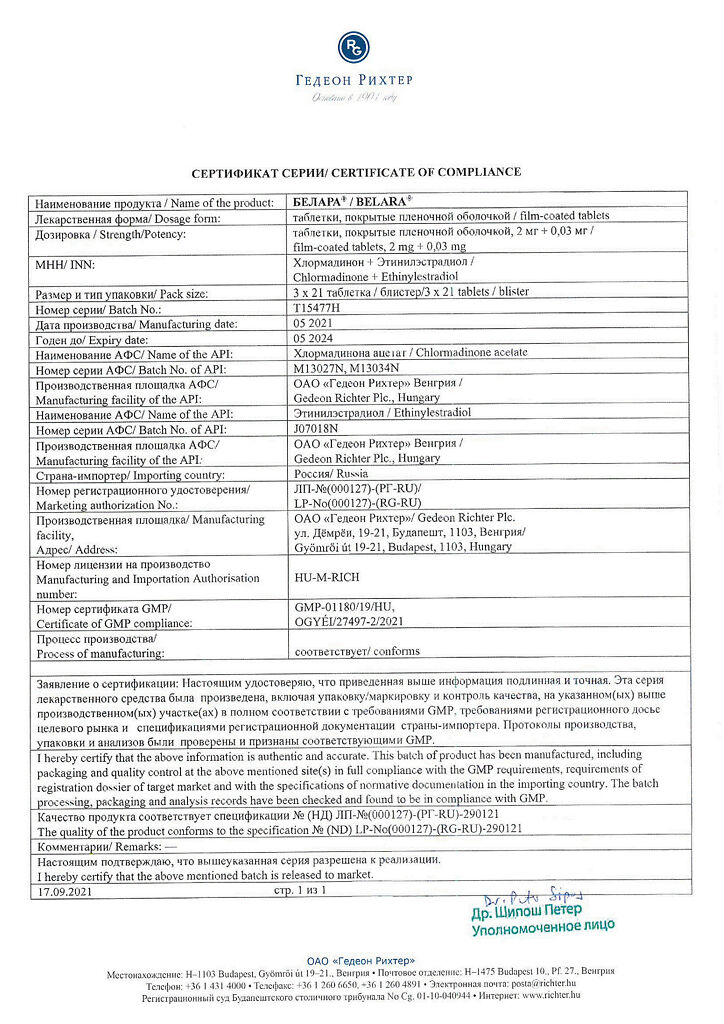
Belara, 2 mg+0.03 mg 63 pcs
€75.31 €73.29
EAN: 5997001363713
SKU: 206719
Categories: Contraceptive, Gynecology and Obstetrics, Hormonal, Medicine
Description
Pharmacodynamics:
Prolonged (more than 21 days) use of BELARA leads to decreased secretion of follicle stimulating hormone and luteinizing hormone and, consequently, suppression of ovulation, endometrial proliferation and its secretory transformation. At the same time the properties of cervical mucus change, which is accompanied by difficulty in the passage of sperm through the cervical canal and impaired sperm motility.
The component of BELARA, chlormadinone acetate, is a progestagen with anti-androgenic properties. Its action is based on the ability to replace androgens at specific receptors, eliminating and weakening the effect of endogenous and exogenous androgens. It takes 1.7 mg of chlormadinone acetate daily to completely suppress ovulation. The required dose per cycle is 25 mg.
BELARA’s other active ingredient, ethinyl estradiol, inhibits skin sweat gland secretion. It also significantly increases the production of globulin that binds sex hormones, thereby reducing the amount of free testosterone in the blood plasma.
Interacts with specialized estrogen receptors in the target organs (in the fallopian tubes, cervix, vagina, external genitalia, mammary ducts) and causes endometrial proliferation.
In addition to its reliable contraceptive properties, the positive effects of BELARA may be observed in menstrual cycle normalization, reduction of premenstrual syndrome, incidence of iron deficiency anemia, dysmenorrhea, functional ovarian cysts, ectopic pregnancy, endometrial and ovarian malignancies, certain forms of benign breast diseases and pelvic inflammatory diseases.
Pharmacokinetics
Chlormadinone acetate and ethinylestradiol are quickly and completely absorbed when the drug is taken orally. The maximum concentration of ethinylestradiol is reached after 1.5 hours. The maximum concentration of chlormadinone acetate is reached in 1-2 hours.
The elimination half-life of chloradinone acetate is approximately 34-39 h, of ethinylestradiol 12-14 h. Chlormadinone acetate metabolites are excreted by the kidneys and through the intestine in the ratio of 2:3.
The elimination half-life of ethinylestradiol is approximately 12-14 h.
The metabolites of ethinylestradiol are water-soluble sulfate or glucuron conjugation derivatives.
Ethinylestradiol metabolites are excreted by the kidneys and through the intestine at a ratio of 4:6.
Indications
Indications
Oral contraception.
Pharmacological effect
Pharmacological effect
Pharmacodynamics:
Long-term (more than 21 days) use of the drug BELARA leads to a decrease in the secretion of follicle-stimulating hormone and luteinizing hormone, and, consequently, suppression of ovulation, endometrial proliferation and its secretory transformation. At the same time, the properties of the mucus of the cervical canal change, which is accompanied by difficulty in the passage of sperm through the cervical canal and a violation of their motility.
Chlormadinone acetate, which is part of BELARA, is a progestogen with antiandrogenic properties. Its action is based on the ability to replace androgens on specific receptors, eliminating and weakening the effect of endogenous and exogenous androgens. To completely suppress ovulation, 1.7 mg of chlormadinone acetate is required daily. The required dose per cycle is 25 mg.
Another active component of BELARA, ethinyl estradiol, inhibits the secretion of skin sweat glands. It also significantly increases the production of sex hormone binding globulin, thereby reducing the amount of free testosterone in the blood plasma.
Interacts with specialized estrogen receptors in target organs (in the fallopian tubes, cervix, vagina, external genitalia, excretory ducts of the mammary glands), causes proliferation of the endometrium.
In addition to the reliable contraceptive effect, the positive effect of the drug BELARA is manifested in the normalization of the menstrual cycle, reducing the severity of premenstrual syndrome, the incidence of iron deficiency anemia, dysmenorrhea, functional ovarian cysts, ectopic pregnancy, malignant formations of the endometrium and ovaries, some forms of benign diseases of the mammary glands and inflammatory diseases of the pelvic organs.
Pharmacokinetics
When taken orally, chlormadinone acetate and ethinyl estradiol are quickly and completely absorbed. The maximum concentration of ethinyl estradiol is achieved after 1.5 hours. The maximum concentration of chlormadinone acetate is achieved after 1–2 hours.
The half-life of chlormadinone acetate is approximately 34-39 hours, ethinyl estradiol – 12-14 hours. Metabolites of chlormadinone acetate are excreted by the kidneys and through the intestines in a ratio of 2:3.
The half-life of ethinyl estradiol is approximately 12–14 hours.
Ethinyl estradiol metabolites are water-soluble derivatives of sulfate or glucuronic conjugation.
Metabolites of ethinyl estradiol are excreted by the kidneys and through the intestines in a ratio of 4:6.
Special instructions
Special instructions
Smoking increases the risk of developing severe cardiovascular side effects of COCs, the risk increases with age and depending on the number of cigarettes smoked and is more pronounced in women over 35 years of age; women over 35 years of age who smoke should use other methods of contraception.
When using COCs, the risk of developing serious diseases increases: myocardial infarction, thrombosis/thromboembolism, stroke and liver tumors.
Other risk factors such as hypertension, hyperlipidemia, obesity and diabetes mellitus clearly increase the risk of morbidity and mortality.
If one of the above diseases/risk factors is present, it is necessary to weigh the possible benefits of prescribing Belara® against the risks, and this should be discussed with the woman before she starts taking the drug. If these diseases or risk factors begin to appear or progress while taking the drug, you should consult your doctor.
Your doctor must decide whether to stop taking this drug.
Thromboembolism and other vascular diseases
It has been noted that there is a relationship between taking COCs and an increased risk of diseases caused by venous or arterial thromboembolism, for example, myocardial infarction, cerebral stroke, deep vein thrombosis or pulmonary embolism. These complications are rare.
Taking COCs leads to an increased risk of venous thromboembolism (VTE). The risk of VTE is greatest during the first year of use. This risk is less than during pregnancy, where the incidence of VTE is 60 cases per 100,000 pregnancies. VTE is fatal in 1–2% of cases. There is no data on assessing the development of the risk of VTE when taking Belara® in comparison with other COCs.
The risk of developing venous thromboembolic complications when taking COCs increases:
with age
in the presence of thromboembolism in relatives (venous thromboembolism in one of the siblings or parents at a relatively young age). If a hereditary predisposition is suspected, it is recommended that the woman be referred for consultation with a specialist before deciding to prescribe COCs.
with long-term decreased mobility
for obesity (body mass index > 30 kg/m2).
The risk of developing arterial thromboembolic complications when taking COCs increases:
with age
in smokers
for dyslipoproteinemia
for obesity (body mass index > 30 kg/m2)
for hypertension
for heart defects
for atrial fibrillation
in the presence of thromboembolism in relatives (arterial thromboembolism in one of the siblings or parents at a relatively young age). If there is chronic inflammation of the intestines (Crohn’s disease and ulcerative colitis), sickle anemia. When assessing the risk/benefit, it should be remembered that adequate treatment of the above diseases can reduce the risk of thrombosis. It is necessary to take into account the increased risk of thromboembolic complications in the postpartum period.
There is no consensus on whether there is a relationship between thrombophlebitis of the superficial veins and/or varicose veins and the etiology of venous thromboembolism.
With the development of venous or arterial thrombosis, the following symptoms may occur:
leg pain and/or swelling
sudden severe pain in the chest, with or without radiation to the left arm
sudden shortness of breath, cough for no apparent reason
sudden, severe, prolonged headache
partial or complete loss of vision, diplopia/speech impairment, or aphasia
dizziness, collapse, in some cases accompanied by a focal epileptic seizure
sudden weakness or dysesthesia (distortion of sensation) on one side or in one part of the body
movement disorders
acute pain in the abdomen.
Women taking COCs should be informed that if symptoms resembling those of thrombosis occur, they should consult their doctor. Belara® should be discontinued if a diagnosis of thrombosis is suspected or confirmed.
An increase in the frequency or severity of migraine attacks while taking COCs (which may be a harbinger of the development or symptom of cerebrovascular disease) may be a reason for their discontinuation.
Tumors
It has been noted that the use of COCs is a risk factor for the development of cervical cancer in women infected with the human papillomavirus (HPV). However, the extent to which other confounding factors (such as number of sexual partners or use of mechanical contraceptives) influence this observation remains controversial (see also Medical Examination).
There is evidence that the relative risk (RR=1.24) of developing breast cancer in women who take COCs is slightly higher. Within 10 years after stopping taking COCs, the risk level gradually decreases and returns to the age level. Because breast cancer is rare in women under 40 years of age, there is little difference between the risk of breast cancer in current and recent COC users and the overall risk of developing the disease.
There are reports of the development in rare cases of benign, and in even more rare cases of malignant liver tumors while taking COCs. In some cases, these tumors are the cause of life-threatening intra-abdominal bleeding. In case of severe abdominal pain that does not go away on its own, hepatomegaly or signs of intra-abdominal bleeding, it is necessary to take into account the possibility of a liver tumor and discontinue Belara®.
Other diseases
Many women taking oral contraceptives experience a slight increase in blood pressure; however, clinically significant increases are rare. The relationship between the prescription of oral contraceptives and the clinical manifestation of hypertension has not yet been confirmed. If a clinically significant increase in blood pressure occurs while taking Belara®, the drug should be discontinued and hypertension treated. As soon as blood pressure levels return to normal against the background of antihypertensive therapy, taking Belara® can be continued.
Women with a history of herpes during pregnancy may experience a relapse of the disease while taking COCs. Women with a history or family history of hypertriglyceridemia are at increased risk of developing pancreatitis while taking COCs. Acute or chronic liver dysfunction may require discontinuation of COCs until liver function tests normalize. Recurrence of cholestatic jaundice, which first occurred during pregnancy or previous use of sex hormones, requires discontinuation of the COC.
COCs may have effects on peripheral tissue insulin resistance or glucose tolerance.
Therefore, patients with diabetes should be under constant supervision while taking oral contraceptives.
In rare cases, chloasma may develop, especially in women who have had chloasma during pregnancy. Women at risk of developing chloasma should avoid sun exposure and ultraviolet radiation while taking oral contraceptives.
Patients with rare congenital conditions such as galactose intolerance, Lapp lactase deficiency or glucose-galactose malabsorption syndrome should not take this drug.
Medical examination
Before prescribing oral contraceptives, it is necessary to collect complete data on the health of the woman and her relatives in order to identify contraindications (see section “Contraindications”) and risk factors (see section “With caution”). The woman must undergo a medical examination.
A medical examination should be carried out annually while taking Belara®. Regular medical examination is also necessary due to the fact that diseases that are contraindications (for example, transient ischemic attacks) or risk factors (for example, venous or arterial thrombosis in relatives) may first occur while taking oral contraceptives. The medical examination should include measuring blood pressure, examining the breasts, abdomen, internal and external genitalia, taking a smear from the cervix and conducting appropriate laboratory tests.
A woman should be warned that the prescription of oral contraceptives, including Belara®, does not protect her from infection with HIV infection (AIDS) or other sexually transmitted diseases.
Lack of efficiency
Missing a pill (see section “Dosage and Administration”, “Skipping a drug”), nausea or symptoms of digestive disorders, including diarrhea, prolonged concomitant use of certain medications (see section “Use in case of diarrhea, vomiting”, “Interaction with other drugs”) or, in very rare cases, metabolic disorders may reduce the effectiveness of contraception.
Effect on the menstrual cycle
Bleeding or “breakthrough” spotting (intermenstrual)
All oral contraceptives may cause irregular vaginal bleeding (breakthrough bleeding/spotting), especially during the first few cycles of taking the drug. Therefore, a medical examination for irregular cycles should be carried out only after an adaptation period, which usually lasts for 3 cycles. If, while taking Belar®, the appearance of extraordinary bleeding continues or appears for the first time in a woman with a regular cycle, it is necessary to conduct an examination to exclude pregnancy or organic pathology; After excluding pregnancy and organic pathology, you can continue taking Belara® or switch to taking another drug.
Bleeding that occurs between cycles may be a sign of insufficient contraceptive effectiveness.
Absence of menstrual-like bleeding (withdrawal bleeding)
Withdrawal bleeding usually occurs 21 days after taking the drug. Sometimes, especially in the first few months of taking the drug, withdrawal bleeding may be absent. However, this is not evidence of insufficient contraceptive effect. If bleeding does not occur after taking the drug for one cycle, provided that no doses of the film-coated tablet were missed, the period after completion of the drug did not exceed 7 days, other drugs were not taken at the same time, there was no nausea or diarrhea, fertilization is unlikely to have occurred, and pregnancy or organic pathology is taking Belara®. After excluding pregnancy and organic pathology, taking Belara® can be continued.
If, when taking Belara®, the instructions were not followed before the first absence of withdrawal bleeding, or withdrawal bleeding was absent for two consecutive cycles, it is necessary to exclude the presence of pregnancy to decide whether to continue taking the drug.
While taking Belara, you should not take herbal remedies containing St. John’s wort (Hypericum perforatum).
Laboratory indicators
While taking COCs, changes in some laboratory parameters may occur, including the functional activity of the liver, adrenal glands and thyroid gland, the level of associated proteins in the plasma (for example, SHBG (SHBG), lipoproteins), indicators of carbohydrate metabolism, coagulation and fibrinolysis.
The nature and extent of changes are determined in part by the nature and dose of hormones taken.
INFLUENCE ON THE ABILITY TO DRIVE A VEHICLE OR WORK WITH PRECISION INSTRUMENTS
No effect.
Active ingredient
Active ingredient
Chlormadinone, Ethinylestradiol
Composition
Composition
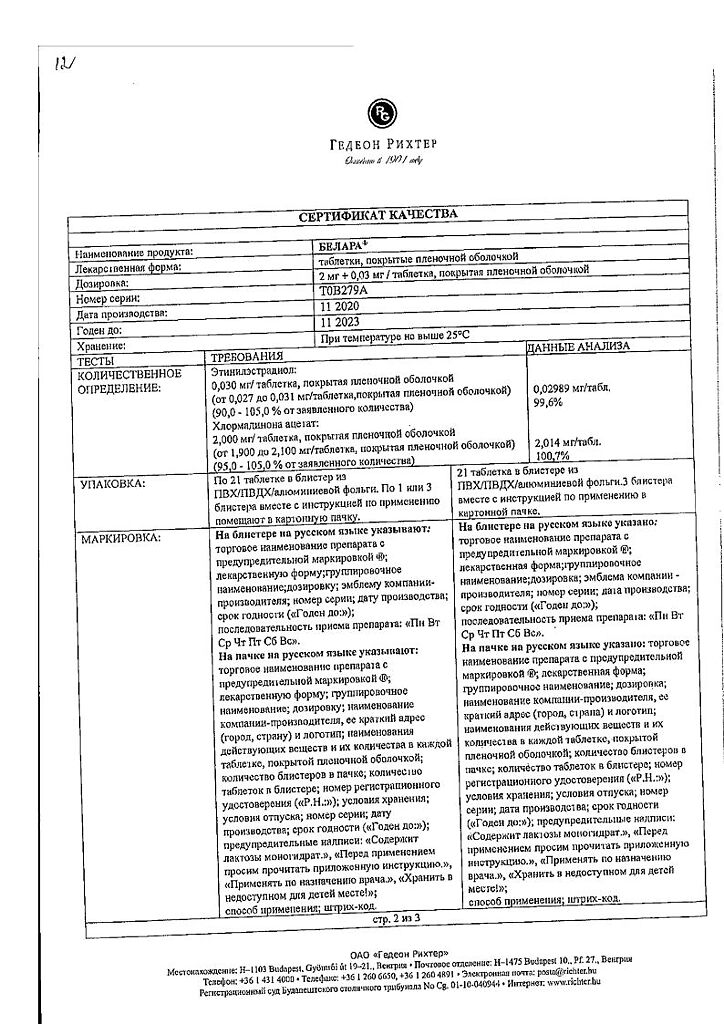
One film-coated tablet contains
active ingredients:
chlormadinone acetate 2 mg and ethinyl estradiol 0.03 mg;
excipients:
povidone K 30 – 4.5 mg,
corn starch – 9.0 mg,
lactose monohydrate – 68.97 mg,
magnesium stearate – 0.5 mg
film shell:
hypromellose 6 mPa.s – 1.115 mg,
lactose monohydrate – 0.575 mg,
macrogol 6000 – 0.279 mg,
propylene glycol – 0.093 mg,
talc – 0.371 mg,
titanium dioxide dye, E 171 – 0.557 mg,
red iron oxide dye (III), E 172 – 0.01 mg.
Pregnancy
Pregnancy
Pregnancy: the use of Belara during pregnancy is contraindicated. Before you start using Belara, you must rule out pregnancy.
If pregnancy occurs while taking Belara, the drug should be stopped immediately. Currently available data do not contain information about the development of teratogenic or embryotoxic effects in women who accidentally took during pregnancy drugs containing estrogens and progesterones in the same combination as in Belara.
Lactation period: it is not recommended to use Belara during breastfeeding, since the drug reduces the amount of milk produced and changes its composition. Small amounts of the hormones included in the contraceptive and/or their metabolites are excreted in breast milk and may affect the nursing baby.
Contraindications
Contraindications
Combined oral contraception (COC) is contraindicated in the following cases. Taking Belara should be stopped immediately if at least one of the following symptoms appears:
the presence of thrombosis (venous and arterial) currently or in history (for example, deep vein thrombosis, pulmonary embolism, myocardial infarction, stroke);
also the presence of the first signs of thrombosis, thrombophlebitis or symptoms of embolism (for example, transient ischemic attacks, angina pectoris);
planned surgical intervention (at least 4 weeks before it) and a period of immobilization, for example, after injury (including after applying plaster casts);
diabetes mellitus with vascular complications;
diabetes mellitus that is not adequately controlled;
uncontrolled hypertension or a significant increase in blood pressure (over 140/90 mmHg, see section “Special instructions”);
hereditary or acquired predisposition to the development of venous or arterial thrombosis, such as increased resistance of the body to activated C protein (APC resistance);
antithrombin III deficiency, C protein deficiency, S protein deficiency, hyperhomocysteinemia and antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant);
hepatitis, jaundice, liver dysfunction (until liver test results normalize);
generalized itching, cholestasis, especially during previous pregnancy or estrogen therapy;
Dubin-Johnson syndrome, Rotor syndrome; conditions/diseases accompanied by impaired bile outflow;
current or history of liver tumors;
severe pain in the epigastrium, enlarged liver or. symptoms of intra-abdominal bleeding (see section “Side effects”);
first manifestation or relapse of porphyria (all three forms, especially acquired porphyria);
the presence of hormone-dependent malignant diseases, including a history (for example, of the breast or uterus) or suspicion of them;
severe disorders of lipid metabolism;
pancreatitis currently or in history, in combination with severe forms of hypertriglyceridemia;
first attacks of migraine pain or frequent severe headaches;
migraine in combination with local neurological symptoms (associated migraine);
acute sensory disturbances, such as visual or hearing impairment;
movement disorders (especially paresis);
worsening of the course of epilepsy;
severe depression;
otosclerosis during previous pregnancies;
amenorrhea of unknown etiology;
endometrial hyperplasia;
bleeding from the vagina of unknown etiology;
hypersensitivity to the components of the drug;
pregnancy or suspicion of it;
breastfeeding period;
smoking over the age of 35 (see section “Special instructions”).
WITH CAUTION
The use of an estrogen/progestogen combination may have a negative effect on the course of certain diseases/conditions.
Special medical supervision is required in the following cases: epilepsy, multiple sclerosis; convulsive syndrome (tetany); migraine; bronchial asthma; heart or kidney failure; chorea; uncomplicated diabetes mellitus; diabetes mellitus (see also section “Contraindications”); liver diseases (see also section “Contraindications”); lipid metabolism disorders, dyslipoproteinemia (see also section “Contraindications”); autoimmune diseases (including systemic lupus erythematosus); obesity; arterial hypertension (see also section “Contraindications”); endometriosis; varicose veins; phlebitis (see also section “Contraindications”); blood coagulation disorder; mastopathy; uterine fibroids; herpes during pregnancy; depression (see also section “Contraindications”); chronic inflammatory bowel diseases (Crohn’s disease, ulcerative colitis).
Side Effects
Side Effects
Adverse reactions from the following organs and systems may occur:
Immune system.
Uncommon: hypersensitivity to the components of the drug, including allergic reactions from the skin.
Metabolism.
Uncommon: changes in blood lipids including hypertriglyceridemia.
Rarely: increased appetite.
Psycho-emotional sphere.
Common: depression, nervousness, irritability.
Uncommon: decreased libido.
Nervous system.
Common: dizziness, migraine (and/or worsening).
Organs of vision.
Common: visual disturbances.
Rarely: conjunctivitis, contact lens intolerance.
Hearing organs and vestibular apparatus.
Rare: sudden hearing loss, tinnitus.
Cardiovascular system.
Often: increased blood pressure.
Rarely: hypertension, hypotension, cardiovascular collapse, varicose veins, venous thrombosis.
Digestive system.
Very Common: Nausea.
Common: vomiting.
Uncommon: abdominal pain, flatulence, diarrhea.
Skin and subcutaneous tissue.
Common: acne.
Uncommon: pigmentation disorders, chloasma, hair loss, dry skin, hyperhidrosis.
Rarely: urticaria, eczema, erythema, skin itching, increased psoriasis, hypertrichosis.
Very rare: erythema nodosum.
Musculoskeletal system.
Often: feeling of heaviness.
Uncommon: back pain, muscle disorders.
Reproductive system and mammary glands.
Very Common: increased mucous discharge from the vagina, dysmenorrhea, amenorrhea.
Often: pain in the lower abdomen.
Uncommon: galactorrhea, breast fibroadenoma, vaginal candidiasis.
Rarely: breast enlargement, vulvovaginitis, menorrhagia, premenstrual syndrome.
General disorders.
Common: fatigue, swelling, weight gain.
When using combined oral contraceptives (COCs), including those containing 0.03 mg ethinyl estradiol and 2 mg chlormadinone acetate, the following undesirable effects were also observed:
– increased risk of venous and arterial thromboembolism (for example, venous thrombosis, pulmonary embolism, stroke, myocardial infarction). The risk may be increased by additional factors, see section “Special instructions”.
– increased risk of biliary tract disease,
– in rare cases, an increased risk of developing benign liver tumors (and even more rarely, malignant liver tumors) and isolated cases can lead to life-threatening intra-abdominal bleeding (see also “Special Instructions”),
– exacerbation of chronic inflammatory bowel diseases (Crohn’s disease, ulcerative colitis).
Interaction
Interaction
The interaction of ethinyl estradiol, the estrogenic component of BELARA®, with other drugs may cause an increase or decrease in the concentration of ethinyl estradiol in the blood serum. If long-term treatment with these medications is necessary, you should switch to non-hormonal contraception.
A decrease in the concentration of ethinyl estradiol in the blood serum may lead to increased episodes of breakthrough bleeding, cycle disruption and a decrease in the contraceptive effectiveness of BELARA®. Increasing serum concentrations of ethinyl estradiol may increase the frequency and severity of side effects.
The following medicinal products/active substances may decrease the serum concentration of ethinyl estradiol:
– all drugs that increase gastrointestinal motility (for example, metoclopramide) or interfere with adsorption (for example, activated carbon);
– active substances that induce liver microsomal enzymes, such as rifampicin, rifabutin, barbiturates, antiepileptic drugs (for example, carbamazepine, oxcarbazepine, phenytoin and topiramate) anticonvulsant felbamate, phenylbutazone, griseofulvin, barbexaclone, primidone, modafinil, some protease inhibitors (for example, ritonavir) and St. John’s wort preparations;
– some antibiotics (for example, ampicillin, tetracycline, rifampicin) – due to a decrease in the enterohepatic circulation of estrogen.
When using such drugs/active substances simultaneously with BELARA® tablets, it is necessary to use additional barrier methods of contraception, both during treatment and for 7 days after it. When taking active substances that reduce the concentration of ethinyl estradiol in the blood serum due to the induction of hepatic microsomal enzymes, additional barrier methods (condom, spermicides) should be used within 28 days after the end of treatment.
The following medicinal products/active substances may increase the serum concentration of ethinyl estradiol:
– active substances that suppress the sulfation of ethinyl estradiol in the intestinal wall, for example, ascorbic acid or paracetamol;
— atorvastatin;
– substances that inhibit the activity of liver microsomal enzymes, such as antifungal imidazoles (for example, fluconazole), indinavir or troleandomycin.
Ethinyl estradiol may affect the metabolism of other substances:
– suppress the activity of hepatic microsomal enzymes and, accordingly, increase the concentration in the blood serum of such active substances as diazepam (and other benzodiazepines, the metabolism of which is carried out through hydroxylation), cyclosporine, theophylline and prednisolone;
– induce glucuronidation in the liver and, accordingly, reduce the concentration in the blood serum of, for example, clofibrate, paracetamol, morphine and lorazepam.
The need for insulin and oral antidiabetic agents may change due to the drug’s effects on glucose tolerance.
Overdose
Overdose
In case of an overdose of the drug, no severe toxic reactions are observed. If you accidentally take a large number of tablets, you may develop nausea, vomiting, spotting/bleeding from the vagina.
There is no specific antidote. Treatment is symptomatic. In rare cases, monitoring of water and electrolyte metabolism and liver function is necessary.
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C
Shelf life
Shelf life
3 years
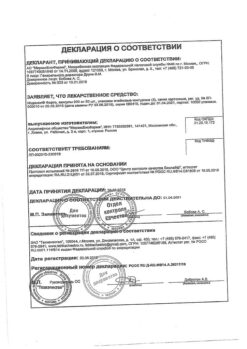
Manufacturer
Manufacturer
Gedeon Richter, Hungary
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Gedeon Richter, Hungary |
| Medication form | pills |
| Brand | Gedeon Richter |
Other forms…
Related products
Gynecology and Obstetrics
Gynecology and Obstetrics
Prepidil, intracervical gel 0.5 mg/3 g syringes with catheter
Buy Belara, 2 mg+0.03 mg 63 pcs with delivery to USA, UK, Europe and over 120 other countries.