No products in the cart.
Description Pharmacotherapeutic group: Antiviral [HIV] drug Pharmacodynamics: Pharmacokinetics:
ATX: J.05.A.F.01 Zidovudine
A synthetic nucleoside analog. Inside the cell, zidovudine is sequentially phosphorylated to the active metabolite, zidovudine-5′-triphosphate. Zidovudine triphosphate inhibits HIV reverse transcriptase by interrupting DNA synthesis of the virus after inclusion in the nucleotide chain. Zidovudine triphosphate weakly inhibits cellular DNA polymerases alpha and gamma.
In combination with other antiviral drugs it increases the number of CD4+ cells.
Adults
Pharmacokinetics when taken orally are dose-independent over a dose range from 2 mg/kg every 8 hours to 10 mg/kg every 4 hours.
Absorption is rapid; ingestion with fatty foods reduces the extent and rate of absorption. Bioavailability in adults is 54-74%. Time of maximum concentration achievement in blood (ТСmах) after oral intake – 0.5-1.5 hours. Volume of distribution is 1.0-2.2 l/kg.
The binding to plasma proteins is less than 38%.
It penetrates into most tissues and body fluids. It is found in cerebrospinal fluid at concentrations of 15-64% of that in plasma. It is metabolized in the liver. The main metabolite of zidovudine is glucuronide, the area under the curve “concentration-time” (AUC) of which is 3 times greater than the AUC of zidovudine. The average half-life (T1/2) from cells is 3.3 h; from blood serum in adults is about 1 h (0.8-1.2 h). After oral administration 14% of zidovudine and 74% of its metabolite are detected in urine.
Patients with impaired renal function
In patients with severe renal impairment the maximum concentration of zidovudine in plasma is increased by 50% compared to that in patients without renal impairment. Systemic exposure of the drug (defined as the area under the “concentration-time” curve) is increased by 100%; the elimination half-life does not change significantly. In renal failure there is a significant cumulation of the main metabolite of zidovudine – glucuronide, with no signs of toxic effects. Hemodialysis and peritoneal dialysis have no effect on zidovudine elimination, while excretion of glucuronide is increased.
Patients with impaired hepatic function
In hepatic insufficiency there may be cumulation of zidovudine due to decreased glucuronidation, which requires adjustment of the drug dose.
Patients in the elderly
The pharmacokinetics of zidovudine have not been studied in patients older than 65 years.
Pharmacokinetics in children
In children over 5-6 months of age, pharmacokinetic parameters are similar to those in adults.
Pregnancy
The pharmacokinetics in pregnant women are similar to those in non-pregnant women.
The plasma concentration of zidovudine in children at birth is the same as in their mothers at delivery.
.
Indications
Indications
Treatment of HIV infection caused by HIV-1 (as part of combination antiretroviral therapy).
Prevention of perinatal transmission of HIV from an infected mother to her child, as zidovudine reduces the risk of intrauterine infection of the fetus.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Antiviral [HIV] agent
ATC: J.05.A.F.01 Zidovudine
Pharmacodynamics:
Synthetic analogue of nucleosides. Inside the cell, zidovudine is sequentially phosphorylated to the active metabolite, zidovudine-5′-triphosphate. Zidovudine triphosphate inhibits HIV reverse transcriptase by interrupting viral DNA synthesis after incorporation into the nucleotide chain. Zidovudine triphosphate weakly inhibits cellular DNA polymerases alpha and gamma.
In combination with other antiviral drugs, it increases the number of CD4+ cells.
Pharmacokinetics:
Adults
Pharmacokinetics when administered orally are dose-independent in the dose range from 2 mg/kg every 8 hours to 10 mg/kg every 4 hours.
Absorption is rapid; taking it with fatty foods reduces the degree and speed of absorption. Bioavailability in adults is 54-74%. The time to reach maximum concentration in the blood (TCmax) after oral administration is 0.5-1.5 hours. Volume of distribution is 1.0-2.2 l/kg.
Communication with plasma proteins is less than 38%.
Penetrates into most tissues and body fluids. Found in the cerebrospinal fluid in a concentration of 15-64% of that in plasma. Metabolized in the liver. The main metabolite of zidovudine is a glucuronide, the area under the concentration-time curve (AUC) of which is 3 times greater than the AUC of zidovudine. The average half-life (T1/2) from cells is 3.3 hours; from blood serum in adults – about 1 hour (0.8-1.2 hours). After oral administration, 14% of zidovudine and 74% of its metabolite are found in the urine.
Patients with impaired renal function
In patients with severe renal impairment, the maximum plasma concentration of zidovudine is increased by 50% compared with that in patients without renal impairment. Systemic exposure of the drug (defined as the area under the concentration-time curve) is increased by 100%; the half-life does not change significantly. In case of renal failure, a significant accumulation of the main metabolite of zidovudine, glucuronide, is observed, but no signs of toxic effects are observed. Hemodialysis and peritoneal dialysis do not affect the elimination of zidovudine, while the excretion of glucuronide is enhanced.
Patients with liver dysfunction
In case of liver failure, accumulation of zidovudine may be observed due to decreased glucuronidation, which requires dose adjustment of the drug.
Elderly patients
The pharmacokinetics of zidovudine have not been studied in patients over 65 years of age.
Pharmacokinetics in children
In children over 5-6 months of age, pharmacokinetic parameters are similar to those in adults.
Pregnancy
Pharmacokinetics in pregnant women is similar to that in non-pregnant women.
Plasma zidovudine concentrations in children at birth are the same as those in their mothers at the time of delivery.
Special instructions
Special instructions
Patients should be informed of the dangers of concomitant use of zidovudine with over-the-counter medications and that the use of zidovudine does not prevent the risk of transmitting HIV to others through sexual contact or blood transfusion. Therefore, patients should take appropriate precautions.
Emergency prevention in case of possible HIV infection
According to international recommendations, if infection is likely through the blood of an HIV-infected person (for example, through an injection needle), it is necessary to urgently (within 1-2 hours from the moment of infection) prescribe combination therapy with zidovudine and lamivudine. In case of a high risk of infection, a drug from the group of protease inhibitors should be included in the antiretroviral therapy regimen. Prophylactic treatment is recommended for 4 weeks. Despite the rapid initiation of treatment with antiretroviral drugs, the possibility of seroconversion cannot be excluded.
Symptoms that are mistaken for adverse reactions to zidovudine may be a manifestation of an underlying disease or a reaction to taking other drugs used to treat HIV infection. The relationship between the developed symptoms and the effect of zidovudine is often very difficult to establish, especially in the advanced clinical picture of HIV infection. In such cases, it is possible to reduce the dose of the drug or discontinue it.
Zidovudine does not cure HIV infection, and patients remain at risk of developing a full-blown disease with immunosuppression and the occurrence of opportunistic infections and malignancies. In HIV infection, zidovudine reduces the risk of developing opportunistic infections, but does not reduce the risk of developing lymphomas.
Adverse reactions from the hematopoietic organs
Anemia (usually observed 6 weeks after the start of zidovudine therapy, but sometimes can develop earlier), neutropenia (usually develops 4 weeks after the start of zidovudine therapy, but sometimes occurs earlier), leukopenia can occur in patients with an advanced clinical picture of HIV infection receiving zidovudine, especially in high doses (1200-1500 mg/day), with reduced bone marrow reserve before the start of therapy. While taking zidovudine in patients with an advanced clinical picture of HIV infection, it is necessary to monitor blood tests at least once every 2 weeks during the first 3 months of therapy, and then monthly. In the early stage of HIV infection (when bone marrow hematopoiesis is still within normal limits), adverse reactions from the blood rarely develop, so blood tests are performed less frequently – depending on the general condition of the patient, once every 1-3 months.
If the hemoglobin content decreases to 75-90 g/l and/or the number of neutrophils decreases to 0.75-1.0 x 109/l, the daily dose of the drug should be reduced, or zidovudine should be discontinued for 2-4 weeks until blood counts are restored. Usually the blood picture returns to normal after 2 weeks, after which zidovudine can be re-prescribed at a reduced dose. If anemia occurs, discontinuation of the drug does not always reduce the need for blood transfusions.
Radiation therapy enhances the myelosuppressive effect of zidovudine.
Lactic acidosis and severe hepatomegaly with steatosis
These complications can be fatal both with zidovudine monotherapy and with zidovudine used as part of combination antiretroviral therapy.
The risk of developing these complications is higher in female patients. Signs of the development of these complications may be general weakness, sudden unexplained weight loss, anorexia, symptoms from the digestive system (nausea, vomiting, abdominal pain), symptoms from the respiratory system (rapid breathing or shortness of breath). If clinical or laboratory signs of lactic acidosis or liver toxicity occur, zidovudine should be discontinued.
Redistribution of subcutaneous fat tissue
In some patients, combination antiretroviral therapy may be accompanied by redistribution/accumulation of subcutaneous fat, incl. a decrease in the amount of adipose tissue in the face and extremities, an increase in visceral fat, enlargement of the mammary glands and fat deposition along the back of the neck and back (“buffalo hump”), as well as an increase in serum lipid concentrations and blood glucose concentrations.
Although all drugs in the protease inhibitor and nucleoside reverse transcriptase inhibitor classes may cause one or more of the above adverse reactions associated with the common syndrome often referred to as lipodystrophy, accumulating evidence suggests that there are differences among individual members of these drug classes in the ability to cause these adverse reactions.
In addition, lipodystrophy syndrome has a multifactorial etiology; for example, stage of HIV infection, advanced age, and duration of antiretroviral therapy play an important, possibly potentiating, role in the development of this complication. The long-term consequences of these adverse reactions have not yet been established. Clinical evaluation of patients should include examination for signs of redistribution of adipose tissue. Serum lipid and glucose concentrations should also be monitored. Lipid imbalances must be corrected according to clinical indications.
Myopathy
It should be borne in mind that the development of symptoms of myopathy (myalgia, weakness, increased activity of creatine phosphokinase) in HIV-infected patients may be associated with the underlying disease. When using zidovudine in doses of 500 mg or 600 mg per day, drug-related myopathy is rare. In case of development of myopathy caused by taking zidovudine, the drug should be discontinued.
Immune reconstitution syndrome
In HIV-infected patients with severe immunodeficiency, during the initiation of antiretroviral therapy, an exacerbation of the inflammatory process against the background of an asymptomatic or indolent opportunistic infection is possible, which can cause a serious deterioration of the condition or aggravation of symptoms. Typically, such reactions were observed in the first weeks or months after the start of antiretroviral therapy. The most significant examples are cytomegalovirus retinitis, generalized and/or focal mycobacterial infection and Pneumocystis pneumonia. Any symptoms of inflammation must be immediately identified and treatment initiated promptly. Autoimmune diseases (such as Graves’ disease, polymyositis and Guillain-Barre syndrome) have been observed in the setting of immune reconstitution, but the timing of initial manifestations varies and the disease may occur many months after the start of therapy and have an atypical course.
Patients infected simultaneously with HIV and hepatitis C virus (HCV)
In vitro studies have shown that ribavirin can reduce the phosphorylation of pyrimidine nucleoside analogues, incl. zidovudine. Although no clear evidence of the pharmacokinetic and pharmacodynamic interaction of ribavirin and zidovudine in patients with co-infection (HIV-1/HCV) was found. Exacerbation of ribavirin-induced anemia has been reported in HIV-infected patients receiving concomitant zidovudine therapy. The mechanism for the development of this effect is currently unknown. Therefore, the simultaneous use of ribavirin and zidovudine is not recommended. The antiretroviral regimen should be replaced with an alternative that does not contain zidovudine, especially if there is a history of zidovudine-associated anemia.
Cases of liver failure (sometimes fatal) have been reported in patients infected with HIV-1 with concomitant hepatitis C receiving combination antiretroviral therapy for HIV-1 and interferon alfa with or without ribavirin. When zidovudine and interferon alfa are used concomitantly with or without ribavirin, patients should be closely monitored for signs of toxicity, particularly liver failure, neutropenia, and anemia. If clinical manifestations of toxicity increase, especially liver failure (> 6 points on the Child-Pugh scale), the dose should be reduced or discontinued interferon alfa, ribavirin, or both drugs. If myelosuppression develops, the possibility of interrupting or discontinuing zidovudine therapy should be considered.
Impact on the ability to drive vehicles. Wed and fur.:
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions. If undesirable effects such as dizziness, drowsiness, lethargy, or convulsions occur, you should refrain from performing these activities.
Active ingredient
Active ingredient
Zidovudine
Composition
Composition
1 tablet contains:
Active ingredient:
Zidovudine 100 mg,
Excipients:
Each film-coated tablet contains:
Core: sodium carboxymethyl starch (Primogel) – 5.0 mg, pregelatinized starch – 5.0 mg, colloidal silicon dioxide (Aerosil brand A-300) – 0.4 mg, magnesium stearate – 0.6 mg, microcrystalline cellulose – 86.0 mg.
Film coating: Ready water-soluble film coating – 3.0 mg. (Shell composition: hydroxypropyl methylcellulose (hypromellose) – 25.0%, copolyvidone – 22.5%, polyethylene glycol 6000 (Macrogol 6000) – 9.5%, glyceryl caprylocaprate – 3.0%, polydextrose – 15.0%, titanium dioxide – 25.0%).
Contraindications
Contraindications
Hypersensitivity to zidovudine or any other component of the drug; neutropenia/leukopenia (neutrophil count below 0.75 x 109/l); anemia (hemoglobin below 75 g/l); simultaneous use with stavudine, doxorubicin, and other drugs that reduce the antiviral activity of zidovudine; childhood (with body weight less than 30 kg).
With caution:
Suppression of bone marrow hematopoiesis, deficiency of cyanocobalamin or folic acid, liver failure, old age, obesity, hepatomegaly, hepatitis or any risk factors for liver disease, neutropenia/leukopenia (neutrophil count 0.75-1.0 x 109/l); anemia (hemoglobin 75-90 g/l).
Side Effects
Side Effects
Adverse reactions that occur during treatment with zidovudine are the same in children and adults.
To assess the frequency of occurrence of adverse reactions, the following gradations were used: very often (>1/10), often (>1/100, 1/1000, 1/10000, <1/1000), very rarely (<1/10000).
From the hematopoietic organs: often – anemia (which may require blood transfusions), neutropenia, leukopenia, infrequently – thrombocytopenia, pancytopenia with bone marrow hypoplasia, rarely – erythrocyte aplasia, very rarely – aplastic anemia.
From the gastrointestinal tract: very often – nausea, often – vomiting, pain in the upper abdomen, diarrhea, infrequently – flatulence, rarely – dyspepsia, taste perversion, pigmentation of the oral mucosa, pancreatitis, anorexia.
From the hepatobiliary system: often – hyperbilirubinemia, increased activity of liver enzymes, rarely – severe hepatomegaly with steatosis.
From the nervous system: very often – headache, often – dizziness, rarely – paresthesia, insomnia, drowsiness, decreased mental performance, convulsions, anxiety, depression.
From the respiratory system: infrequently – shortness of breath, rarely – cough.
From the cardiovascular system: cardiomyopathy.
From the urinary system: rarely – frequent urination.
From the endocrine system and metabolism: often – hyperlactatemia, rarely – lactic acidosis, gynecomastia.
From the musculoskeletal system: often – myalgia, infrequently – myopathy.
From the skin: infrequently – skin rash, itching; rarely – pigmentation of nails and skin, increased sweating, urticaria.
Other: often – malaise, infrequently – fever, asthenia, generalized pain syndrome, rarely – flu-like syndrome, chills, chest pain, redistribution/accumulation of subcutaneous fat.
Adverse reactions that occur when using zidovudine to prevent the transmission of HIV infection from mother to fetus.
Pregnant women tolerate zidovudine well at recommended doses. In children, a decrease in hemoglobin levels is observed, which, however, does not require blood transfusions. Anemia disappears 6 weeks after completion of zidovudine therapy.
Interaction
Interaction
Zidovudine is used as part of combination antiretroviral therapy together with other nucleoside reverse transcriptase inhibitors and drugs from other groups (protease inhibitors, non-nucleoside reverse transcriptase inhibitors). The list of interactions listed below should not be considered exhaustive, but they are typical for drugs that require careful use with zidovudine.
Lamivudine: There is a moderate increase in maximum blood concentration (28%) for zidovudine when administered together with lamivudine, however, the overall exposure (AUC) is not affected. Zidovudine has no effect on the pharmacokinetics of lamivudine.
Phenytoin: Zidovudine reduces the concentration of phenytoin in the blood, which requires monitoring the concentration of phenytoin in the blood when administered simultaneously with zidovudine.
Probenicide: reduces glucuronidation and increases the mean half-life and AUC of zidovudine. Renal excretion of glucuronide and zidovudine itself is reduced in the presence of probenecid.
Atovaquone: Zidovudine does not affect the pharmacokinetic parameters of atovaquone. Atovachone slows down the glucuronidation of zidovudine (the AUC of zidovudine at steady state increases by 33%, maximum glucuronide concentrations decrease by 19%). The safety profile of zidovudine administered at doses of 500 or 600 mg per day is unlikely to change when coadministered with atovaquone for three weeks.
If longer-term concomitant use of these drugs is necessary, careful monitoring of the patient’s clinical condition is recommended.
Clarithromycin: reduces the absorption of zidovudine. The break between doses of drugs should be at least 2 hours.
Valproic acid, fluconazole, methadone: reduce the clearance of zidovudine, resulting in increased systemic exposure.
Ribavirin: The nucleoside analogue ribavirin is an antagonist of zidovudine. The simultaneous use of zidovudine and ribavirin should be avoided.
Rifampicin: Combination of zidovudine with rifampicin resulted in a 48% ± 34% reduction in the AUC for zidovudine, however, the clinical significance of this change is unknown.
Stavudine: Zidovudine can inhibit intracellular phosphorylation of stavudine.
Stavudine should not be used simultaneously with zidovudine.
Others: Drugs such as paracetamol, acetylsalicylic acid, codeine, methadone, morphine, indomethacin, ketoprofen, naproxen, oxazepam, lorazepam, cimetidine, clofibrate, dapsone, isoprinosine may interfere with the metabolism of zidovudine through competitive inhibition of glucuronidation or direct inhibition of microsomal metabolism in the liver. The possibility of using these drugs in combination with zidovudine, especially for long-term therapy, should be approached with caution. The combination of zidovudine, especially in emergency treatment, with potentially nephrotoxic and myelotoxic drugs (for example, pentamidine, dapsone, pyrimethamine, co-trimoxazole, amphotericin, flucytosine, ganciclovir, interferon, vincristine, vinblastine, doxorubicin) increases the risk of adverse reactions to zidovudine. It is necessary to monitor kidney function and blood counts and reduce the dose of drugs if necessary.
Overdose
Overdose
Symptoms: fatigue, headache, vomiting, abnormal hematological parameters.
Treatment: symptomatic. Hemodialysis and peritoneal dialysis are not very effective in removing zidovudine from the body, but they accelerate the elimination of its metabolite, glucuronide.
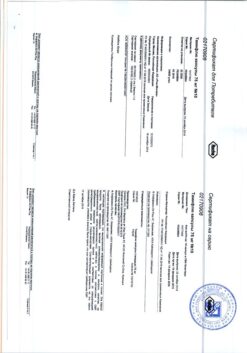
Storage conditions
Storage conditions
Store in the original manufacturer’s packaging at a temperature not exceeding 25 °C. Keep out of the reach of children.
Shelf life
Shelf life
2 years. Do not use after the expiration date indicated on the package.
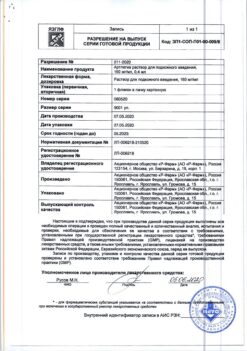
Manufacturer
Manufacturer
Pharmasintez JSC, Russia
Additional information
| Shelf life | 2 years. Do not use after the expiry date printed on the package. |
|---|---|
| Conditions of storage | Store in the original package of the manufacturer at the temperature not more than 25 °С. Keep out of reach of children. |
| Manufacturer | Pharmasintez JSC, Russia |
| Medication form | pills |
| Brand | Pharmasintez JSC |
Related products
Buy Azimitem, 100 mg 100 pcs with delivery to USA, UK, Europe and over 120 other countries.