No products in the cart.
Description
Pharmacological action Pharmacological action is antitumor.
Pharmacodynamics
The mechanism of action
The mechanism of action of paclitaxel is based on its ability to stimulate the assembly of microtubules of the mitotic spindle from dimeric tubulin molecules and stabilize microtubules by inhibiting their depolymerization. This leads to the suppression of the normal dynamic reorganization of the microtubule network in the interphase of mitosis and also causes the formation of abnormal clusters of microtubules throughout the cell cycle and the appearance of multiple star-shaped clusters (asters) in the mitosis phase.
Abraxan contains nanodispersed paclitaxel stabilized by albumin with nanoparticle size of approximately 130 nm with paclitaxel in a non-crystalline (amorphous) state.
After injection the nanoparticles rapidly dissociate to form soluble paclitaxel complexes bound to albumin with an approximate size of 10 nm. Albumin is known to regulate the transendothelial transport of plasma components, and in in vitro studies it was demonstrated that the presence of albumin in Abraxane stimulates paclitaxel transport through the endothelial cell layer. It has been hypothesized that transendothelial transport is mediated by the albumin transporter gp-60 and there is increased cumulation of paclitaxel in the tumor due to the presence of an albumin-binding protein, acid secreted cysteine-rich protein (SPARC).
Pharmacokinetics
The pharmacokinetics (PK) of paclitaxel have been studied in clinical studies at 30- and 180-minute infusions of Abraxane at doses ranging from 80 to 375 mg/m2. AUC values for paclitaxel increased linearly, from 2653 to 16736 ng/h/mL over a dose range of 80 to 300 mg/m2.
In a study involving patients with advanced solid tumors, paclitaxel parameters (FC) after an IV injection of Abraxane at a dose of 260 mg/m2 for 30 minutes were compared with FC parameters after administration of solvent-based paclitaxel at a dose of 175 mg/m2 for 3 hours. Based on the uncompartmentalized analysis, paclitaxel clearance (43%) and its Vd (53%) were higher with administration of Abraxane than with solvent-based paclitaxel.
No differences in terminal T1/2 were reported. In a study of multiple IV infusions of Abraxane at a dose of 260 mg/m2 in 12 patients, intraindividual variability in paclitaxel systemic exposure (AUC) was 19% (range of values = 3.21-27.7%). No evidence of paclitaxel cumulation was recorded with multiple courses of therapy.
Distribution. After administration of Abraxane to patients with solid tumors, paclitaxel was evenly distributed in blood cells, plasma and 94% bound to plasma proteins. Binding of paclitaxel to proteins was assessed by ultrafiltration in a comparison study in the same patient. The fraction of free paclitaxel was significantly higher with Abraxane (6.2%) than with solvent-based paclitaxel (2.3%). This provided significantly higher exposure values of the unbound fraction of paclitaxel when administered with Abraxane than with solvent-based paclitaxel, even with comparable values of total exposure.
This phenomenon is probably due to the lack of paclitaxel binding to Cremophor EL micelles that is observed with solvent-based paclitaxel. According to published studies that evaluated in vitro binding of paclitaxel (at concentrations from 0.1 to 50 µg/ml) to human plasma proteins, the presence of cimetidine, ranitidine, dexamethasone or diphenhydramine had no effect on paclitaxel binding to plasma proteins.
In view of the results of a population-based analysis of FC data, the total Vd is approximately 1741 L; a large Vd indicates intense extravascular distribution and/or binding of paclitaxel to tissue proteins.
Metabolism and excretion. In in vitro studies using liver microsomes and human tissue slices have shown that paclitaxel is metabolized predominantly to form 6α-hydroxypaclitaxel and two additional metabolites present in smaller amounts (3′-n-hydroxypaclitaxel and 6α-3′-n-dihydroxypaclitaxel). The formation of these hydroxylated metabolites is catalyzed by cytochrome P450 system isoenzymes CYP2C8, CYP3A4, and both CYP2C8 and CYP3A4, respectively.
In patients with metastatic breast cancer, after an IV drip injection of Abraxane for 30 minutes at a dose of 260 mg/m2, the mean cumulative urinary excretion of unchanged active ingredient corresponded to 4% of the total drug dose administered; less than 1% of the administered dose were the urinary excreted metabolites 6α-hydroxypaclitaxel and 3′-n-hydroxypaclitaxel, indicating significant extrarenal clearance of the drug. Paclitaxel is predominantly eliminated by hepatic metabolism and excretion with bile. When administered at a therapeutic dose of 80 to 300 mg/m2, mean plasma clearance of paclitaxel ranges from 13 to 30 L/h/m2, and mean terminal T1/2 ranges from 13 to 27 h.
Particular patient groups
Hepatic impairment. The results of the clinical studies demonstrated that mild hepatic insufficiency (total bilirubin >1 to ≤1.5×VGN) had no clinically significant effect on the FC parameters of paclitaxel. In patients with moderate hepatic impairment (total bilirubin >1.5 to ≤3×VGN) and severe (total bilirubin >3 to ≤5×VGN), a 22-26% decrease in the maximum elimination rate of paclitaxel and an approximately 20% increase in the mean AUC of paclitaxel were observed.
Hepatic insufficiency had no effect on the mean Cmax value of paclitaxel. In addition, paclitaxel elimination was inversely correlated with measures of total bilirubin and directly correlated with measures of plasma albumin concentration.
Pharmacokinetic/pharmacodynamic modeling showed no correlation between liver function (as measured by baseline albumin or total bilirubin concentration) and neutropenia in relation to Abraxane exposure. FC analysis was not performed in patients with total bilirubin >5×VGN or patients with metastatic pancreatic adenocarcinoma (see “Dosage and administration”).
Kidney function impairment. Mild to moderate renal impairment (creatinine Cl ≥30 to <90 ml/min) had no clinically significant effect on the maximum elimination rate and systemic exposure (AUC and Cmax) of paclitaxel. There is insufficient FC analysis data for patients with severe renal impairment and no data for patients with end-stage renal failure.
Elderly patients. A population-based FC analysis of Abraxane included data from patients aged 24 to 85 years. The results showed that age had no significant effect on the maximum elimination rate and systemic exposure (AUC and Cmax) of paclitaxel.
Pharmacokinetic/pharmacodynamic modeling using data from 125 patients with advanced solid tumors showed that patients aged >65 years may be more prone to develop neutropenia during the first cycle of therapy, although age had no effect on plasma paclitaxel exposure.
Other intrinsic factors. A population-based FC analysis of Abraxane demonstrated that gender, race (mongoloid vs. Caucasoid) and type of sólid tumors had no clinically significant effect on the systemic exposure (AUC and Cmax) of paclitaxel. The AUC of paclitaxel in patients with a body weight of 50 kg is approximately 25% lower than in patients with a body weight of 75 kg. The clinical significance of these data is unknown.
Indications
Indications
Metastatic colorectal cancer:
in combination with chemotherapy based on fluoropyrimidine derivatives.
Locally recurrent or metastatic breast cancer:
as first line therapy in combination with paclitaxel.
Advanced unresectable, metastatic or recurrent non-squamous non-small cell lung cancer:
as first-line therapy in addition to platinum-based chemotherapy.
Advanced and/or metastatic renal cell carcinoma:
as first line therapy in combination with interferon alfa-2a.
Glioblastoma (glioma grade IV according to WHO classification):
in combination with radiation therapy and temozolomide in patients with newly diagnosed glioblastoma;
in monotherapy or in combination with irinotecan in patients with glioblastoma relapse or disease progression.
Epithelial cancer of the ovary, fallopian tube and primary peritoneal cancer:
as first-line therapy in combination with carboplatin and paclitaxel for advanced (IIIB, IIIC and IV stages according to FIGO classification) epithelial cancer of the ovary, fallopian tube and primary peritoneal cancer;
in combination with carboplatin and gemcitabine for recurrent platinum-sensitive epithelial cancer of the ovary, fallopian tube and primary peritoneal cancer in patients who have not previously received therapy with bevacizumab or other VEGF inhibitors;
in combination with paclitaxel or topotecan or pegylated liposomal doxorubicin for recurrent platinum-resistant epithelial ovarian, fallopian tube and primary peritoneal cancer in patients who have previously received no more than two chemotherapy regimens.
Pharmacological effect
Pharmacological effect
Pharmacological action
Pharmacological action – antitumor.
Pharmacodynamics
Mechanism of action
The mechanism of action of paclitaxel is based on its ability to stimulate the assembly of mitotic spindle microtubules from dimeric tubulin molecules and stabilize microtubules by inhibiting their depolymerization. This leads to the suppression of the normal dynamic reorganization of the microtubular network in the interphase of mitosis, and also causes the formation of abnormal clusters of microtubules throughout the cell cycle and the appearance of multiple star-shaped clusters (asters) in the mitotic phase.
Abraxane contains nanodispersed paclitaxel, stabilized by albumin, with a nanoparticle size of approximately 130 nm, in which paclitaxel is in a non-crystalline (amorphous) state.
After intravenous administration, the nanoparticles quickly dissociate to form soluble complexes of paclitaxel bound to albumin, the approximate size of which is 10 nm. Albumin is known to regulate the processes of transendothelial transport of plasma components, and in vitro studies have demonstrated that the presence of albumin in Abraxane stimulates the transport of paclitaxel through the endothelial cell layer. It has been hypothesized that transendothelial transport is mediated by the albumin transporter gp-60 and that there is increased accumulation of paclitaxel in the tumor due to the presence of the albumin-binding protein secreted acidic protein rich in cysteine (SPARC).
Pharmacokinetics
The pharmacokinetics (PK) of paclitaxel was studied in clinical studies with 30- and 180-minute infusions of Abraxane in doses ranging from 80 to 375 mg/m2. AUC values for paclitaxel increased linearly, from 2653 to 16736 ng·h/ml over the dose range from 80 to 300 mg/m2.
In a study of patients with advanced solid tumors, PK parameters of paclitaxel after IV administration of Abraxane at a dose of 260 mg/m2 over 30 minutes were compared with PK parameters after administration of vehicle-based paclitaxel at a dose of 175 mg/m2 over 3 hours. Based on the results of the analysis without taking into account compartments, paclitaxel clearance (43%) and Vd it (53%) was higher with Abraxane than with solvent-based paclitaxel.
No differences in terminal T1/2 were recorded. In a study of repeated IV administration of Abraxane 260 mg/m2 in 12 patients, the intra-individual variability in paclitaxel systemic exposure (AUC) was 19% (range = 3.21–27.7%). There were no signs of accumulation of paclitaxel during several courses of therapy.
Distribution. After administration of the drug Abraxane to patients with solid tumors, paclitaxel was evenly distributed in blood cells, plasma and was 94% bound to plasma proteins. Protein binding of paclitaxel was assessed by ultrafiltration in a comparison study in the same patient. The proportion of free paclitaxel was significantly higher with Abraxane (6.2%) than with solvent-based paclitaxel (2.3%). This resulted in significantly higher exposures to the unbound paclitaxel fraction when administered with Abraxane than to vehicle-based paclitaxel, even with comparable total exposures.
This phenomenon is likely due to the lack of binding of paclitaxel to Cremophor EL micelles, which is observed when using solvent-based paclitaxel. According to published studies in which the binding of paclitaxel (at concentrations ranging from 0.1 to 50 mcg/ml) to human plasma proteins was assessed in vitro, the presence of cimetidine, ranitidine, dexamethasone or diphenhydramine did not affect the binding of paclitaxel to plasma proteins.
Considering the results of the population analysis of PK data, the total Vd is approximately 1741 L; a large Vd indicates extensive extravascular distribution and/or binding of paclitaxel to tissue proteins.
Metabolism and excretion. In vitro studies using liver microsomes and human tissue sections showed that paclitaxel is metabolized predominantly to 6α-hydroxypaclitaxel, as well as two additional metabolites present in smaller quantities (3′-n-hydroxypaclitaxel and 6α-3′-n-dihydroxypaclitaxel). The formation of these hydroxylated metabolites is catalyzed by the cytochrome P450 isoenzymes CYP2C8, CYP3A4, and both CYP2C8 and CYP3A4, respectively.
In patients with metastatic breast cancer after intravenous drip administration of the drug Abraxane for 30 minutes at a dose of 260 mg/m2, the average cumulative urinary excretion of unchanged active substance corresponded to 4% of the total administered dose of the drug; less than 1% of the administered dose was excreted in the urine by the metabolites 6α-hydroxypaclitaxel and 3′-n-hydroxypaclitaxel, indicating significant extrarenal clearance of the drug. Paclitaxel is primarily eliminated through hepatic metabolism and biliary excretion. When the drug is administered at a therapeutic dose of 80 to 300 mg/m2, the average plasma clearance of paclitaxel varies from 13 to 30 l/h/m2, and the average terminal T1/2 ranges from 13 to 27 hours.
Special patient groups
Liver dysfunction. The results of clinical studies demonstrated that mild liver failure (total bilirubin >1 to ≤1.5×ULN) did not have a clinically significant effect on the PK parameters of paclitaxel. In patients with moderate (total bilirubin >1.5 to ≤3×ULN) and severe hepatic impairment (total bilirubin >3 to ≤5×ULN), a decrease in the maximum rate of paclitaxel elimination by 22–26% and an increase in the mean AUC of paclitaxel by approximately 20% were observed.
Hepatic impairment did not affect the mean Cmax of paclitaxel. In addition, the elimination of paclitaxel was inversely correlated with total bilirubin and directly correlated with plasma albumin concentrations.
Pharmacokinetic/pharmacodynamic modeling showed no correlation between liver function (as measured by baseline albumin or total bilirubin concentrations) and neutropenia, taking into account Abraxane exposure. PK analysis was not performed in patients with total bilirubin >5×ULN or in patients with metastatic pancreatic adenocarcinoma (see Dosage and Administration).
Renal dysfunction. Mild to moderate renal impairment (creatinine clearance ≥30 to <90 mL/min) did not have a clinically significant effect on the maximum elimination rate and systemic exposure (AUC and Cmax) of paclitaxel. There is insufficient PK analysis data for patients with severe renal impairment and no data for patients with end-stage renal disease.
Elderly patients. The population PK analysis of Abraxane included data from patients aged 24 to 85 years. The results showed that age does not have a significant effect on the maximum elimination rate and systemic exposure (AUC and Cmax) of paclitaxel.
Pharmacokinetic/pharmacodynamic modeling using data from 125 patients with advanced solid tumors suggested that patients aged >65 years may be more susceptible to developing neutropenia during the first cycle of therapy, although age did not influence plasma paclitaxel exposure.
Other internal factors. A population PK analysis of Abraxane demonstrated that sex, race (Mongoloid versus Caucasian), and solid tumor type did not have a clinically significant effect on the systemic exposure (AUC and Cmax) of paclitaxel. The AUC of paclitaxel in patients weighing 50 kg is approximately 25% lower than in patients weighing 75 kg. The clinical significance of these data is unknown.
Special instructions
Special instructions
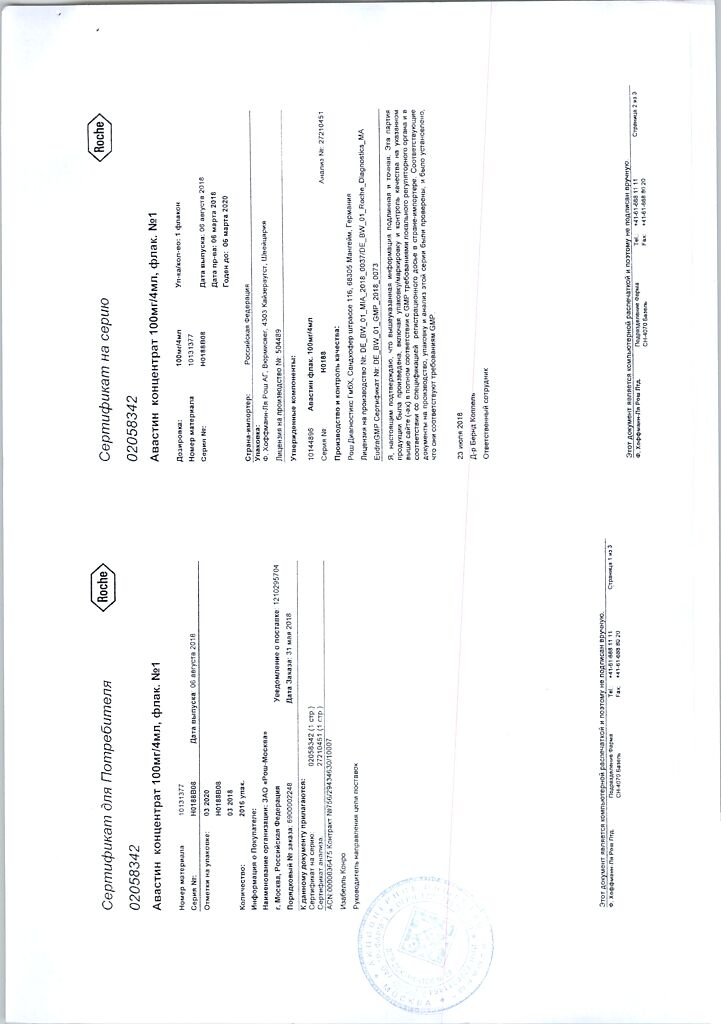
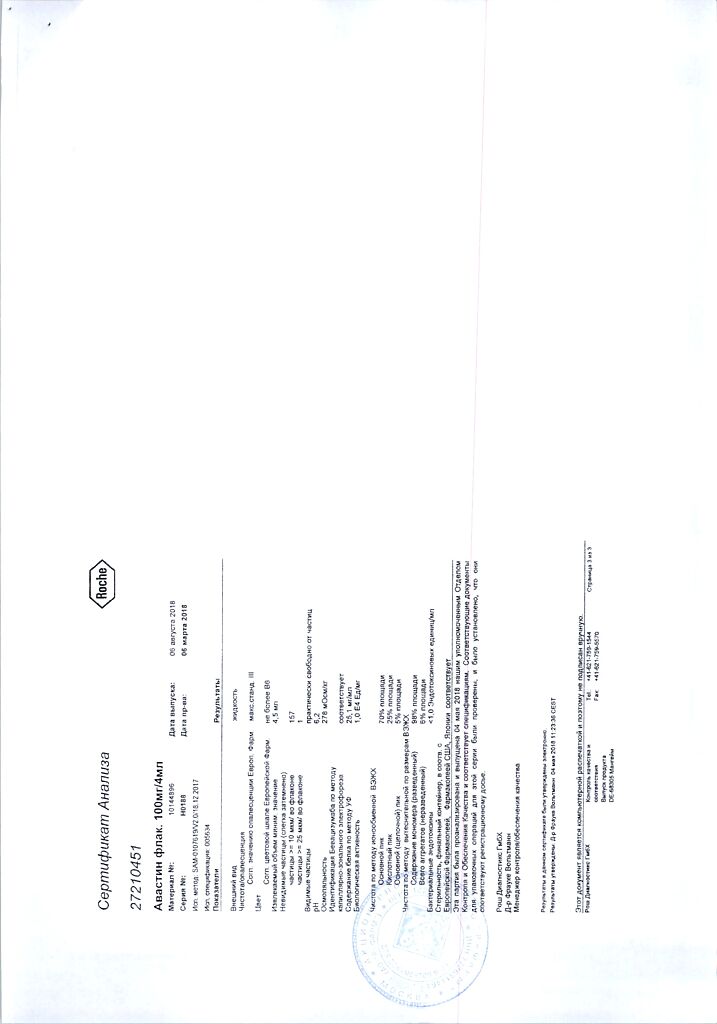
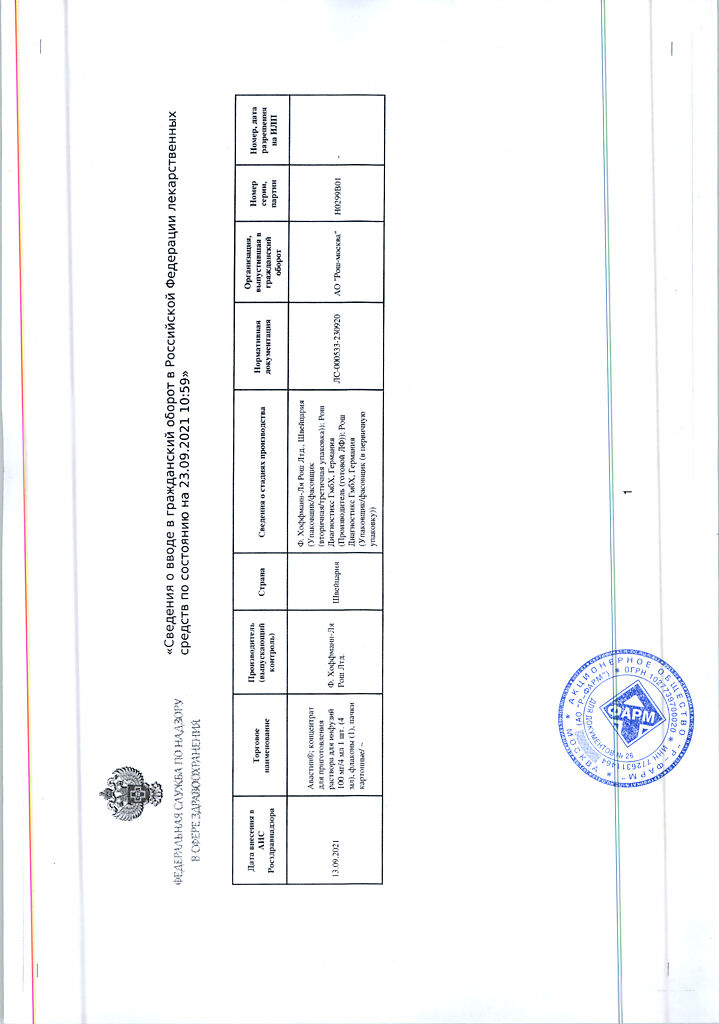
The patient’s medical records should indicate the trade name of the drug (Avastin®). Replacing the drug with any other biological drug requires agreement with the attending physician. The information presented in this description applies only to Avastin®.
Treatment with Avastin® should only be carried out under the supervision of a physician experienced in the use of anticancer therapy.
Patients receiving Avastin® are at increased risk of developing gastrointestinal and gallbladder perforations. Severe cases of gastrointestinal perforation were observed, incl. and fatal (in 0.2-1% of all patients receiving Avastin®). The clinical presentation of gastrointestinal perforations varied in severity and ranged from signs of free gas on abdominal radiography that resolved without treatment to perforations with abdominal abscess and death.
In some cases, there was underlying intraperitoneal inflammation due to gastric ulceration, tumor necrosis, diverticulitis, or chemotherapy-associated colitis. The relationship between the development of intraperitoneal inflammation and gastrointestinal perforation and treatment with Avastin® has not been established. If gastrointestinal perforation develops, treatment with Avastin should be discontinued.
Serious cases of fistula formation, including fatal cases, have been reported during treatment with Avastin®. Gastrointestinal fistulas most often occurred in patients with metastatic colorectal cancer and ovarian cancer (up to 2% of patients), less often in other tumor locations. Infrequently (≥0.1-<1%) cases of fistula formation in other locations (bronchopleural, urogenital, biliary) were recorded. The formation of fistulas is most often observed in the first 6 months of therapy with Avastin®, but can occur both after 1 week and 1 year or later after the start of therapy.
If a tracheoesophageal fistula or a fistula of any location of grade 4 severity occurs, Avastin® therapy should be discontinued. There is limited information about the continued use of Avastin® in patients with fistulas of other locations. If an internal fistula that does not penetrate the gastrointestinal tract occurs, discontinuation of Avastin® should be considered.
Patients receiving Avastin® are at increased risk of bleeding, especially bleeding from the tumor. Avastin should be discontinued if NCI-CTC grade 3 or 4 bleeding occurs. The overall incidence of grade 3-5 bleeding when using Avastin® for all indications is 0.4-6.5%. Most often, bleeding from the tumor or minor bleeding from the mucous membrane and skin (for example, nosebleeds) was observed. Most often, nosebleeds of grade 1 severity according to the NCI-CTC classification were observed, lasting less than 5 minutes, resolved without medical intervention and did not require a change in the dosage regimen of Avastin®. The frequency of minor bleeding from the mucous membrane and skin depends on the dose of the drug. Minor gum bleeding or vaginal bleeding occurred less frequently.
Heavy or massive pulmonary bleeding/hemoptysis was observed mainly in non-small cell lung cancer. Taking antirheumatic/anti-inflammatory drugs, anticoagulants, previous radiation therapy, atherosclerosis, central location of the tumor, cavity formation before or during treatment are possible risk factors for the development of pulmonary hemorrhage/hemoptysis, while only for squamous cell lung cancer a statistically significant association with the development of bleeding was established.
Patients who have recently had bleeding/hemoptysis (more than 2.5 ml of blood) should not receive Avastin®.
Patients with colorectal cancer may experience gastrointestinal bleeding associated with the tumor, incl. rectal bleeding and melena.
Bleeding was rarely observed, incl. intracranial hemorrhages, in patients with metastatic lesions of the central nervous system or with glioblastoma.
It is necessary to monitor symptoms of intracranial hemorrhage, and if they occur, discontinue treatment with Avastin®.
In patients with congenital bleeding diathesis, acquired coagulopathy, or receiving full-dose anticoagulants for thromboembolism, caution should be exercised before prescribing Avastin due to the lack of information on the safety profile of the drug in such patients. There was no increase in the incidence of grade 3 or higher bleeding in patients receiving Avastin® and warfarin.
Isolated cases and case series of serious ocular adverse events (including infectious endophthalmitis and other inflammatory diseases) have been reported following unapproved intravitreal administration of Avastin®. Some of these events have resulted in varying degrees of loss of visual acuity, including permanent blindness. Avastin® is not intended for intravitreal administration.
An increased incidence of arterial hypertension of all degrees of severity (up to 42.1%) was observed in patients receiving Avastin®. For all indications, the frequency of arterial hypertension of 3-4 severity according to the NCI-CTC classification was 0.4%-17.9%; Grade 4 severity (hypertensive crisis) was observed in 1% of patients.
Clinical safety data suggest that the incidence of elevations in blood pressure is likely dose dependent on bevacizumab.
Avastin® can be prescribed only to patients with pre-compensated arterial hypertension with further blood pressure control. There is no information on the effect of Avastin® in patients with uncontrolled hypertension at the time of initiation of therapy. In patients with arterial hypertension requiring drug therapy, it is recommended to temporarily discontinue Avastin® therapy until blood pressure normalizes.
In most cases, normalization of blood pressure is achieved with the help of standard antihypertensive drugs (ACE inhibitors, diuretics and slow calcium channel blockers), selected individually for each patient. Discontinuation of Avastin® therapy or hospitalization was rarely required.
Very rare cases of hypertensive encephalopathy have been observed, some with fatal outcome. The risk of hypertension associated with Avastin therapy does not correlate with baseline patient characteristics, concomitant disease, or concomitant therapy.
Therapy with Avastin® should be discontinued if blood pressure does not normalize, hypertensive crisis or hypertensive encephalopathy develops.
During therapy with Avastin®, isolated cases of posterior reversible encephalopathy syndrome have been reported, manifested by an epileptic seizure, headache, mental disorders, visual impairment, damage to the visual centers of the cerebral cortex, with or without arterial hypertension and other symptoms. The diagnosis can be confirmed using brain imaging techniques (preferably MRI). If posterior reversible encephalopathy syndrome develops, symptomatic therapy should be prescribed, blood pressure should be carefully monitored, and Avastin should be discontinued. Resolution or improvement of symptoms usually occurs within a few days, but neurological complications have been observed in some patients. The safety of repeated administration of Avastin in these patients has not been established.
When treated with Avastin® in combination with chemotherapy, the incidence of arterial thromboembolism, including stroke, transient ischemic attack and myocardial infarction and other arterial thromboembolism events, was higher than when prescribing chemotherapy alone. The overall incidence of arterial thromboembolism was 3.8%. If arterial thromboembolism occurs, treatment with Avastin® should be discontinued. A history of arterial thromboembolism or age over 65 years are associated with an increased risk of arterial thromboembolism during treatment with Avastin®. Caution must be exercised when treating such patients.
During treatment with Avastin® there is an increased risk of developing venous thromboembolism (PE, deep vein thrombosis, thrombophlebitis). The overall incidence of venous thromboembolism (deep vein thrombosis and pulmonary embolism) varies from 2.8% to 17.3%.
Treatment with Avastin® should be discontinued if a life-threatening event (grade 4 severity) of venous thromboembolism, including PE, occurs, and if the severity of venous thromboembolism is ≤3, the patient’s condition should be carefully monitored.
Chronic heart failure (CHF) occurred with the use of Avastin® for all indications, but mainly in metastatic breast cancer. Both asymptomatic decreases in left ventricular ejection fraction and CHF requiring therapy or hospitalization were observed.
CHF of grade 3 or higher was observed in 3.5% of patients receiving Avastin®. In patients receiving Avastin® in combination with anthracycline drugs, the incidence of CHF grade 3 or higher did not differ from the available data in the treatment of metastatic breast cancer. Most patients experienced improvement in symptoms and/or left ventricular ejection fraction with appropriate treatment.
There are no data on the risk of developing CHF in patients with a history of CHF II-IV according to the NYHA classification.
In most cases, CHF occurred in patients with metastatic breast cancer who received anthracycline therapy, a history of radiation therapy to the chest area, or with other risk factors for the development of CHF.
Caution should be exercised when prescribing Avastin® to patients with a history of clinically significant cardiovascular disease, such as coronary heart disease or CHF.
In patients who had not previously received anthracycline therapy, there was no increase in the incidence of CHF of any severity when using Avastin® and anthracycline drugs compared to monotherapy with anthracycline drugs. CHF grade 3 or higher occurred slightly more often in the group receiving Avastin® in combination with chemotherapy compared with chemotherapy alone, which is consistent with other data obtained in patients with metastatic breast cancer and not receiving concomitant anthracycline therapy.
In patients with diffuse large B-cell lymphoma, when treated with bevacizumab and doxorubicin at a cumulative dose of more than 300 mg/m2, an increase in the number of new cases of CHF was observed. When comparing rituximab/cyclophosphamide/doxorubicin/vincristine/prednisolone (R-CHOP) + bevacizumab and R-CHOP, the number of new cases did not differ, but was higher than previously observed with doxorubicin therapy. The incidence of CHF was higher in the R-CHOP+ bevacizumab group.
Avastin® may adversely affect wound healing. Treatment with bevacizumab should be started at least 28 days after major surgery or when the surgical wound is completely healed. If complications associated with wound healing develop during treatment, Avastin® should be temporarily discontinued until the wound is completely healed. Avastin® should also be temporarily discontinued in the event of elective surgery.
Rare cases of necrotizing fasciitis (including fatal cases) have been reported in patients treated with Avastin®. This complication, as a rule, developed against the background of impaired wound healing, gastrointestinal perforation or fistula formation. If necrotizing fasciitis is detected, Avastin® should be discontinued and appropriate treatment initiated immediately.
Proteinuria was observed in 0.7-38% of patients receiving Avastin®. The severity of proteinuria ranged from transient asymptomatic detection of traces of protein in the urine and, in 1.4% of patients, to nephrotic syndrome (grade 4 proteinuria). Grade 3 proteinuria was reported in 8.1% of patients receiving Avastin® for various indications. Proteinuria was not associated with renal dysfunction and rarely required discontinuation of Avastin® therapy. The risk of developing proteinuria is increased in patients with a history of arterial hypertension. It is possible that grade 1 proteinuria depends on the dose of Avastin®.
If grade 4 proteinuria develops, Avastin® should be discontinued. A urine test for proteinuria is recommended before and during treatment with Avastin®.
In most cases with proteinuria ≥2 g/day, Avastin therapy was temporarily suspended until proteinuria decreased to <2 g/day.
An increased incidence of severe neutropenia, febrile neutropenia, or infections with severe neutropenia (including fatal cases) was observed when Avastin was used in combination with myelotoxic chemotherapy regimens.
Patients may be at increased risk of developing infusion/hypersensitivity reactions. There is evidence of a higher incidence of anaphylactic and anaphylactoid-type reactions in patients receiving Avastin in combination with chemotherapy compared to patients receiving chemotherapy alone.
Close monitoring of the patient is recommended during and after administration of Avastin®. If an infusion reaction occurs, the infusion must be interrupted and appropriate medical measures taken. Systematic premedication cannot guarantee the absence of infusion reactions/hypersensitivity reactions.
Cases of osteonecrosis of the jaw have been reported in cancer patients receiving Avastin®. Most of these patients had received IV bisphosphonates previously or as concomitant therapy; osteonecrosis of the jaw is an identified risk with bisphosphonates. Caution should be exercised when using Avastin® and IV bisphosphonates simultaneously or sequentially. Invasive dental procedures are also an identified risk factor. Before starting treatment with Avastin®, a dental examination and appropriate preventive dental measures should be performed. If possible, invasive dental procedures should be avoided in patients who have previously received or are currently receiving IV bisphosphonates.
Patients over 65 years of age: When prescribing Avastin® to patients over 65 years of age, there is an increased risk of arterial thromboembolism (including stroke, transient ischemic attack, myocardial infarction), grade 3-4 leukopenia and thrombocytopenia, as well as neutropenia (all degrees of severity), diarrhea, nausea, headache and fatigue compared to patients ≤65 years of age. years. There was no increase in the incidence of other adverse reactions associated with the use of Avastin® (gastrointestinal perforation, complications associated with wound healing, arterial hypertension, proteinuria, CHF and bleeding) in patients over 65 years of age compared to patients ≤65 years of age.
Disposal of unused or expired medication must be carried out in accordance with the requirements of the medical institution.
Impact on the ability to drive vehicles and other mechanisms that require increased concentration
Studies have not been conducted to study the effect of the drug on the ability to drive vehicles or operate machinery. Patients who experience adverse events such as syncope, drowsiness or blurred vision should refrain from driving vehicles or machinery.
Active ingredient
Active ingredient
Bevacizumab
Composition
Composition
Active ingredient:
bevacizumab 100 mg.
Excipients:
α,α-trehalose dihydrate – 240 mg,
sodium dihydrogen phosphate monohydrate – 23.2 mg,
sodium hydrogen phosphate anhydrous – 4.8 mg,
polysorbate 20 – 1.6 mg,
water for d/i – up to 4 ml.
Pregnancy
Pregnancy
The drug is contraindicated for use during pregnancy and breastfeeding.
Men and women of childbearing potential must use reliable contraception during treatment with Avastin® and for at least 6 months after treatment.
Avastin® may impair fertility in women. In most patients, fertility was restored after discontinuation of Avastin® therapy. The long-term effects of Avastin® therapy on fertility are unknown.
Breastfeeding is not recommended during treatment with Avastin® and for at least 6 months after the end of treatment with Avastin.
Contraindications
Contraindications
Hypersensitivity to bevacizumab or any other component of the drug, drugs based on Chinese hamster ovary cells or other recombinant human or close to human antibodies;
renal and liver failure (efficacy and safety of use have not been established);
pregnancy;
breastfeeding period;
children under 18 years of age (efficacy and safety have not been established).
With caution: the drug should be prescribed if there is a history of arterial thromboembolism; diabetes mellitus; patients over 65 years of age; with congenital hemorrhagic diathesis and acquired coagulopathy; taking anticoagulants for the treatment of thromboembolism before starting treatment with Avastin®; clinically significant cardiovascular disease (history of coronary artery disease or chronic heart failure); arterial hypertension; venous thromboembolism; wound healing; bleeding/hemoptysis; history of gastrointestinal perforation; posterior reversible encephalopathy syndrome; neutropenia; proteinuria.
Side Effects
Side Effects
The most serious adverse reactions: gastrointestinal perforation, hemorrhage, including pulmonary hemorrhage/hemoptysis (more common in patients with non-small cell lung cancer), arterial thromboembolism.
In patients receiving Avastin®, the most common symptoms observed were: increased blood pressure, weakness or asthenia, diarrhea and abdominal pain.
The increase in blood pressure and the development of proteinuria is likely to be dose-dependent.
Below are the National Cancer Institute-CTC grades of adverse reactions that occurred in patients receiving Avastin® in combination with various chemotherapy regimens for all indications.
The following criteria are used to describe the frequency of adverse reactions:
very often (≥10%);
often (≥1%-<10%);
uncommon (≥0.1%-<1%);
rarely (≥0.01% - <0.1%);
very rare (<0.01%).
Adverse reactions are classified into a specific category according to the highest frequency of occurrence. Within one frequency category, adverse reactions are presented in order of decreasing severity. Some of the listed adverse reactions are often observed during chemotherapy (for example, hand-foot syndrome during therapy with capecitabine and peripheral sensory neuropathy during therapy with paclitaxel or oxaliplatin); however, aggravation of the condition cannot be ruled out during therapy with Avastin®. When using Avastin® in combination with pegylated liposomal doxorubicin, there may be an increased risk of developing hand-foot syndrome.
From the hematopoietic system: very often – febrile neutropenia, leukopenia, neutropenia, thrombocytopenia; often – anemia.
From the nervous system: very often – peripheral sensory neuropathy, dysgeusia, headache, dysarthria; often – stroke, syncope, drowsiness.
From the organ of vision: very often – blurred vision, increased lacrimation.
From the cardiovascular system: very often – increased blood pressure; often – chronic heart failure, supraventricular tachycardia, arterial thromboembolism, deep vein thrombosis, bleeding (including pulmonary, intracranial, from the mucous membrane and skin, gastrointestinal tract and tumors).
From the respiratory system: very often – shortness of breath, nosebleeds, rhinitis; often – pulmonary embolism (PE), hypoxia.
From the digestive system: very often – anorexia, diarrhea, nausea, vomiting, constipation, stomatitis, rectal bleeding; often – gastrointestinal perforation, intestinal obstruction (including obstructive), abdominal pain, gastrointestinal disorders.
From the reproductive system: very often – ovarian failure (amenorrhea lasting 3 months or more (FSH concentration ≥30 mIU/ml with a negative pregnancy test with determination of beta human chorionic gonadotropin in serum)).
From the skin and subcutaneous tissues: very often – exfoliative dermatitis, dry skin, change in skin color; often – hand-foot syndrome.
From the musculoskeletal system: very often – arthralgia; often – muscle weakness, myalgia.
From the urinary system: very often – proteinuria; often – urinary tract infection.
Local reactions: very often – pain, incl. at the site of drug administration.
Other: very often – asthenia, increased fatigue, pyrexia, inflammation of the mucous membranes of various localizations; often – lethargy, lethargy, sepsis, abscess, secondary infections, dehydration.
Laboratory parameters: hyperglycemia, hypokalemia, hyponatremia, increased prothrombin time, increased MHO.
Post-marketing surveillance
From the nervous system: rarely – posterior reversible encephalopathy syndrome; very rarely – hypertensive encephalopathy.
From the cardiovascular system: the frequency of occurrence is unknown – thrombotic microangiopathy of the kidneys, clinically manifested by proteinuria.
From the respiratory system: often – dysphonia; frequency of occurrence is unknown – perforation of the nasal septum, pulmonary hypertension.
From the gastrointestinal tract: frequency of occurrence is unknown – gastrointestinal ulcer.
From the liver and biliary tract: the frequency of occurrence is unknown – perforation of the gallbladder.
Allergic and infusion reactions: frequency of occurrence unknown – hypersensitivity reactions, infusion reactions with the following possible simultaneous manifestations: shortness of breath/difficulty breathing, flushing/redness/rash, decreased or increased blood pressure, decreased oxygen saturation, chest pain, chills and nausea/vomiting.
From the musculoskeletal system: osteonecrosis of the jaw (mainly in patients receiving concomitant therapy with bisphosphonates or who have previously received bisphosphonate therapy).
Other: rarely – necrotizing fasciitis, usually due to impaired wound healing, gastrointestinal perforation or fistula formation.
Interaction
Interaction
Effect of anticancer drugs on the pharmacokinetics of Avastin®
There was no clinically significant effect on the pharmacokinetics of Avastin® when used in combination with chemotherapy. There were no statistically or clinically significant differences in the clearance of Avastin® between patients receiving monotherapy and patients receiving Avastin® in combination with interferon alfa-2a or other chemotherapy drugs (IFL, FU/LV, carboplatin/paclitaxel, capecitabine, doxorubicin or cisplatin/gemcitabine).
Effect of Avastin® on the pharmacokinetics of other anticancer drugs
Avastin® does not have a significant effect on the pharmacokinetics of irinotecan and its active metabolite (SN38), capecitabine and its metabolites, as well as oxaliplatin (determined by free and total platinum levels), interferon alfa-2a, and cisplatin.
There are no reliable data on the effect of Avastin® on the pharmacokinetics of gemcitabine.
Combination of Avastin® and sunitinib When using Avastin® (10 mg/kg once every 2 weeks) in combination with sunitinib (50 mg daily), cases of microangiopathic hemolytic anemia (MAHA) have been reported in patients with metastatic renal cell carcinoma.
MAHA belongs to a subgroup of hemolytic anemias that may present with red blood cell fragmentation, anemia, and thrombocytopenia. Some patients additionally experience neurological disorders, increased creatinine concentrations, and arterial hypertension, including hypertensive crisis. These symptoms were reversible after discontinuation of bevacizumab and sunitinib therapy.
Radiation therapy
When Avastin® is used in combination with radiation therapy and chemotherapy (temozolomide) in patients with newly diagnosed glioblastoma, the safety profile of the drug remains unchanged.
The safety and effectiveness of Avastin® in combination with radiation therapy for other indications has not been established.
Pharmaceutical interactions
Avastin® is pharmaceutically incompatible with dextrose solutions.
Overdose
Overdose
Symptoms: When bevacizumab was prescribed at a maximum dose of 20 mg/kg IV every 2 weeks, severe headache (migraine) was reported in several patients. In case of overdose, the listed dose-dependent side effects may increase.
Treatment: there is no specific antidote. Treatment is symptomatic.
Storage conditions
Storage conditions
In a place protected from light, at a temperature of 2–8 °C (do not freeze)
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
F.Hoffmann-La Roche Ltd, Switzerland
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In the dark place at 2-8 °C (do not freeze) |
| Manufacturer | Roche Diagnostics GmbH, Germany |
| Medication form | concentrate for preparation of infusion solution |
| Brand | Roche Diagnostics GmbH |
Related products
Buy Avastin, 100 mg/4 ml with delivery to USA, UK, Europe and over 120 other countries.