No products in the cart.
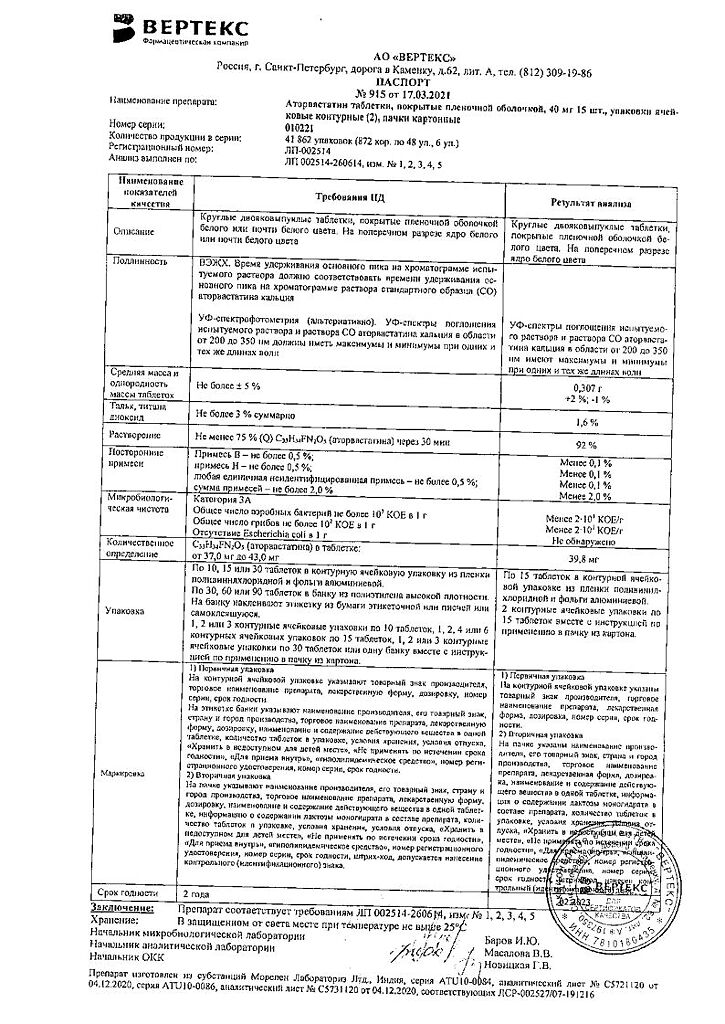
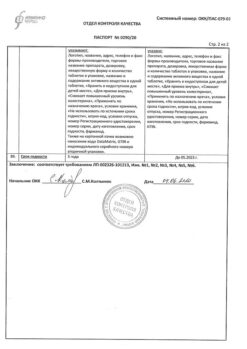
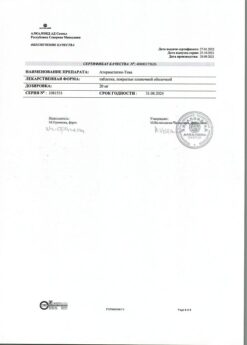
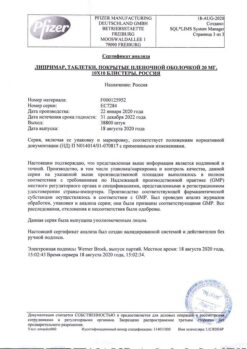
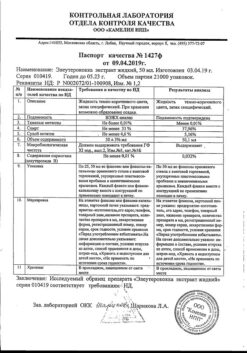
Atorvastatin-Vertex, 40 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Atorvastatin is a hypolipidemic drug of the III generation from the group of statins.
Indications
Indications
– in combination with a diet to reduce elevated levels of total cholesterol, LDL cholesterol, apolipoprotein B and TG and increase the level of HDL cholesterol in patients with primary hypercholesterolemia, heterozygous familial and non-familial hypercholesterolemia and combined (mixed) hyperlipidemia (types IIa and IIb according to Fredrickson);
– in combination with diet for the treatment of patients with elevated serum TG levels (Fredrickson type IV) and patients with dysbetalipoproteinemia (Fredrickson type III) in whom diet therapy does not provide an adequate effect;
– to reduce the levels of total cholesterol and LDL cholesterol in patients with homozygous familial hypercholesterolemia, when diet therapy and other non-pharmacological treatment methods are not effective enough.
Pharmacological effect
Pharmacological effect
Atorvastatin is a third-generation lipid-lowering drug from the group of statins.
Special instructions
Special instructions
Before starting Atorvastatin therapy, the patient must be prescribed a standard cholesterol-lowering diet, which he must follow during the entire treatment period.
The use of HMG-CoA reductase inhibitors to reduce blood lipid levels can lead to changes in biochemical parameters reflecting liver function. Liver function should be monitored before starting therapy, 6 weeks, 12 weeks after starting Atorvastatin and after each dose increase, and periodically, for example, every 6 months.
An increase in the activity of liver enzymes in the blood serum may be observed during therapy with Atorvastatin. Patients who experience elevated enzyme levels should be monitored until enzyme levels return to normal. If alanine aminotransferase (ALT) or aspartic aminotransferase (AST) values are more than 3 times the upper acceptable limit, it is recommended to reduce the dose of Atorvastatin or discontinue treatment.
Atorvastatin should be used with caution in patients who abuse alcohol and/or have liver disease. Active liver disease or persistent increases in aminotransferase activity of unknown origin are contraindications to the use of Atorvastatin. Treatment with Atorvastatin may cause myopathy.
The diagnosis of myopathy (muscle pain and weakness in combination with an increase in creatine phosphokinase (CPK) activity more than 10 times the upper limit of normal) should be considered in patients with widespread myalgia, muscle soreness or weakness, and/or a marked increase in CPK activity.
Patients should be warned that they should immediately tell their doctor if they experience unexplained muscle pain or weakness if they are accompanied by malaise or fever. Atorvastatin therapy should be discontinued in the event of a marked increase in CPK activity or in the presence of confirmed or suspected myopathy.
The risk of myopathy during treatment with other drugs in this class was increased with concomitant use of cyclosporine, fibrates, erythromycin, niacin, or azole antifungals. Many of these drugs inhibit cytochrome P450 3A4-mediated metabolism and/or drug transport.
Atorvastatin is biotransformed by CYP 3A4. When prescribing Atorvastatin in combination with fibrates, erythromycin, immunosuppressive agents, azole antifungals or nicotinic acid in lipid-lowering doses, the expected benefits and risks of treatment should be carefully weighed and patients should be regularly monitored for muscle pain or weakness, especially during the first months of treatment and during periods of increasing dosage of any drug.
In such situations, periodic determination of CPK activity can be recommended, although such monitoring does not prevent the development of severe myopathy.
When using Atorvastatin, as well as other drugs of this class, cases of rhabdomyolysis with acute renal failure caused by myoglobinuria have been described. Atorvastatin therapy should be temporarily discontinued or completely discontinued if signs of possible myopathy appear or if there is a risk factor for the development of renal failure due to rhabdomyolysis (for example, severe acute infection, hypotension, major surgery, trauma, severe metabolic, endocrine and electrolyte disturbances, and uncontrolled seizures).
Before starting therapy with Atorvastatin, an attempt should be made to control hypercholesterolemia through adequate diet therapy, increased physical activity, weight loss in obese patients, and treatment of other conditions. Patients should be warned to seek immediate medical attention if they experience unexplained muscle pain or weakness, especially if accompanied by malaise or fever.
Active ingredient
Active ingredient
Atorvastatin
Composition
Composition
Active ingredient:
atorvastatin calcium trihydrate;
Excipients:
calcium carbonate;
MCC;
StarCap1500 (corn starch and pregelatinized starch);
colloidal silicon dioxide (Aerosil);
talc; magnesium stearate;
Opadry II (series 85) (polyvinyl alcohol, macrogol, talc, titanium dioxide, iron oxide yellow, iron oxide red).
Contraindications
Contraindications
– active liver diseases;
– increased activity of liver enzymes of unknown origin (more than 3 times compared to ULN);
– liver failure (classes A and B on the Child-Pugh scale);
– pregnancy;
– lactation period;
– age under 18 years (efficacy and safety have not been established);
– hypersensitivity to the components of the drug.
The drug should be used with caution in patients with chronic alcoholism, a history of liver disease, severe electrolyte imbalance, endocrine and metabolic disorders, arterial hypotension, severe acute infections (sepsis), uncontrolled epilepsy, extensive surgical interventions, trauma, and skeletal muscle diseases.
Side Effects
Side Effects
In controlled clinical trials (n=2502), less than 2% of patients discontinued treatment due to side effects caused by atorvastatin. The most common adverse effects associated with atorvastatin were constipation, flatulence, dyspepsia and abdominal pain.
From the nervous system and sensory organs: ≥2% – headache, asthenic syndrome, insomnia, dizziness;
From the cardiovascular system: ≥2% – chest pain; blood pressure, phlebitis, arrhythmia, angina pectoris, anemia, lymphadenopathy, thrombocytopenia.
From the respiratory system: ≥2% – sinusitis, pharyngitis, bronchitis, rhinitis;
From the gastrointestinal tract: ≥2% – abdominal pain, constipation or diarrhea, dyspepsia, flatulence, nausea;
From the musculoskeletal system: ≥2% – arthralgia, myalgia, arthritis;
From the genitourinary system: ≥2% – urogenital infections, peripheral edema;
From the skin: Allergic reactions: ≥2% – skin rash;
Other: ≥2% – infections, accidental trauma, influenza-like syndrome, back pain; ALP, increased ALT or AST, exacerbation of gout.
Side effects noted in post-marketing studies with atorvastatin therapy: anaphylaxis, angioedema, bullous rash (including erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis), rhabdomyolysis, tendon rupture.
Interaction
Interaction
The risk of developing myopathy during treatment with statins increases when used in combination with cyclosporine, fibrates, erythromycin, nicotinic acid in lipid-lowering doses, strong CYP3A4 inhibitors (including clarithromycin, HIV protease inhibitors, itraconazole).
When using atorvastatin in combination with inhibitors of the CYP3A4 isoenzyme (for example, cyclosporine, macrolide antibiotics – erythromycin and clarithromycin; itraconazole, HIV protease inhibitors), plasma concentrations of atorvastatin may increase (atorvastatin is metabolized with the participation of CYP3A4); Particular caution should be exercised when using atorvastatin in combination with the above-mentioned drugs (see “Special Instructions”).
With the combined use of atorvastatin at a dose of 40 mg and itraconazole at a dose of 200 mg 1 time per day, an increase in the AUC of atorvastatin by 3 times was detected compared to the AUC with monotherapy. The simultaneous use of atorvastatin with protease inhibitors (lopinavir/ritonavir, ritonavir/saquinavir) was accompanied by an increase in the concentration of atorvastatin in the blood plasma.
With simultaneous use of atorvastatin at a dose of 40 mg and the combination of lopinavir + ritonavir (at a dose of 400/100 mg 2 times a day), an increase in the AUC of atorvastatin by 5.9 times was detected compared to the AUC with monotherapy. When atorvastatin was used at a dose of 40 mg with the combination of ritonavir + saquinavir (at a dose of 400/400 mg 2 times a day), its AUC increased by 3.9 times.
Antacids reduce the concentration of atorvastatin by 35% (the effect on LDL cholesterol does not change). With repeated administration of digoxin and atorvastatin, digoxin Css increases by approximately 20% (patients need to be monitored).
When atorvastatin is used together with oral contraceptives, the AUC of norethindrone and ethinyl estradiol increases by approximately 30 and 20% (this effect should be taken into account when choosing an oral contraceptive for a woman receiving atorvastatin).
When taken concomitantly with erythromycin (CYP3A4 inhibitor), the plasma concentration of atorvastatin increases by approximately 40%.
The lipid-lowering effect of the combination of atorvastatin with colestipol is superior to that of each drug separately.
Concomitant use with drugs that reduce the concentration or activity of endogenous steroid hormones (including ketoconazole, spironolactone, cimetidine) increases the risk of reducing the production of endogenous steroid hormones (caution should be exercised).
When atorvastatin was administered concomitantly with a suspension containing magnesium aluminum hydroxide, atorvastatin plasma concentrations were reduced by approximately 35%, but the degree of reduction in LDL/cholesterol levels did not change.
Overdose
Overdose
Treatment: there is no specific antidote; symptomatic therapy is carried out.
Hemodialysis is ineffective.
Storage conditions
Storage conditions
Store in a dry place, protected from light, out of reach of children, at a temperature of 15 C to 30 C.
Shelf life
Shelf life
2 years.
Manufacturer
Manufacturer
Vertex, Russia
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | Store in a dry place protected from light, out of the reach of children, at a temperature of 15 C to 30 C. |
| Manufacturer | Vertex, Russia |
| Medication form | pills |
| Brand | Vertex |
Other forms…
Related products
Buy Atorvastatin-Vertex, 40 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.