No products in the cart.
Atorvastatin-Vertex, 10 mg 90 pcs
€16.65 €13.87
Description
Atorvastatin is a selective competitive inhibitor of HMG-CoA reductase, a key enzyme converting 3-hydroxy-3-methylglutaryl-CoA to mevalonate, a precursor of steroids, including cholesterol; a synthetic hypolipidemic drug.
. In patients with homozygous and heterozygous familial hypercholesterolemia, nonfamilial forms of hypercholesterolemia and mixed dyslipidemia, atorvastatin reduces plasma concentrations of total cholesterol (CH) low-density lipoprotein cholesterol (LDL-C) and apolipoprotein B (apo-B), as well as the concentration of very low density lipoproteins (VLDL-C) and triglycerides (TG), causes unstable increase in concentration of high density lipoprotein cholesterol (HDL-C).
Atorvastatin reduces plasma cholesterol and lipoprotein concentrations by inhibiting HMG-CoA reductase and cholesterol synthesis in the liver and, by increasing the number of “hepatic” LDL receptors on the cell surface, leads to increased capture and catabolism of Hs-LDL.
Atorvastatin decreases formation of LDL-C and LDL particle number, causes marked and persistent increase of LDL receptor activity in combination with favorable qualitative changes of LDL particles and decreases concentration of LDL-C in patients with homozygous hereditary familial hypercholesterolemia resistant to therapy with other hypolipidemic agents.
Atorvastatin at doses of 10 to 80 mg reduces total cholesterol concentration by 30-46%, LDL-C by 41-61%, apo-B by 34-50% and TG by 14-33%. Results of therapy are similar in patients with heterozygous familial hypercholesterolemia, nonfamilial forms of hypercholesterolemia and mixed hyperlipidemia, including patients with type 2 diabetes.
In patients with isolated hypertriglyceridemia, atorvastatin decreases the concentration of total cholesterol, chs-LDL, chs-LONP, apo-B and TG and increases the concentration of HDL-C. In patients with dysbetalipoproteinemia it reduces the concentration of intermediate density lipoprotein cholesterol (X-LDL).
In patients with hyperlipoproteinemia of type IIa and IIb according to Fredrickson classification the mean value of increase of HDL-C concentration during treatment with atorvastatin (10-80 mg) in comparison with baseline is 5.1-8.7% and it is not dose dependent. There is a significant dose-dependent decrease in the values of ratios: total cholesterol/Cs-LDL and Chs-LDL/Cs-LDL by 29-44% and 37-55%, respectively.
Atorvastatin at a dose of 80 mg significantly reduced the risk of ischemic complications and mortality by 16% after a 16-week course, and the risk of rehospitalization for angina with signs of myocardial ischemia by 26%. In patients with different baseline concentrations of CHD (with myocardial infarction without Q-wave and unstable angina, men and women, in patients younger and older than 65 years) atorvastatin causes reduction of risk of coronary complications and mortality.
Decrease in plasma concentration of Chs-LDL better correlates with the dose of atorvastatin than with its plasma concentration. The dose is adjusted taking into account the therapeutic effect (see section “Dosage and administration”).
Therapeutic effect is achieved 2 weeks after the start of therapy, reaches a maximum after 4 weeks and lasts for the duration of therapy.
Indications
Indications
primary hypercholesterolemia (heterozygous familial and non-familial hypercholesterolemia (Fredrickson type IIa);
combined (mixed) hyperlipidemia (Fredrickson types IIa and IIb);
dysbetalipoproteinemia (Fredrickson type III) (as an addition to the diet);
familial endogenous hypertriglyceridemia (Fredrickson type IV), resistant to diet;
homozygous familial hypercholesterolemia with insufficient effectiveness of diet therapy and other non-pharmacological treatments;
primary prevention of cardiovascular complications in patients without clinical signs of coronary artery disease (coronary heart disease), but with several risk factors for its development – age over 55 years, nicotine addiction, arterial hypertension, diabetes mellitus, genetic predisposition, incl. against the background of dyslipidemia;
secondary prevention of cardiovascular complications in patients with coronary artery disease with the aim of reducing the total mortality rate, myocardial infarction, stroke, re-hospitalization for angina pectoris and the need for revascularization.
Pharmacological effect
Pharmacological effect
Atorvastatin is a selective competitive inhibitor of HMG-CoA reductase, a key enzyme that converts 3-hydroxy-3-methylglutaryl-CoA into mevalonate, a precursor of steroids, including cholesterol; synthetic lipid-lowering agent.
In patients with homozygous and heterozygous familial hypercholesterolemia, non-familial forms of hypercholesterolemia and mixed dyslipidemia, atorvastatin reduces the plasma concentrations of total cholesterol (C), low-density lipoprotein cholesterol (LDL-C) and apolipoprotein B (apo-B), as well as the concentration of very low-density lipoproteins (VLDL-C) and triglycerides (TG), causes an unstable increase in the concentration of high-density lipoprotein cholesterol (HDL-C).
Atorvastatin reduces the concentration of cholesterol and lipoproteins in the blood plasma by inhibiting HMG-CoA reductase and cholesterol synthesis in the liver and, by increasing the number of “liver” LDL receptors on the cell surface, leads to increased uptake and catabolism of LDL-C.
Atorvastatin reduces the formation of LDL-C and the number of LDL particles, causes a pronounced and persistent increase in the activity of LDL receptors in combination with favorable qualitative changes in LDL particles, and also reduces the concentration of LDL-C in patients with homozygous hereditary familial hypercholesterolemia, resistant to therapy with other lipid-lowering drugs.
Atorvastatin in doses from 10 to 80 mg reduces the concentration of total cholesterol by 30-46%, LDL-C by 41-61%, apo-B by 34-50% and TG by 14-33%. The results of therapy are similar in patients with heterozygous familial hypercholesterolemia, non-familial forms of hypercholesterolemia and mixed hyperlipidemia, incl. in patients with type 2 diabetes mellitus.
In patients with isolated hypertriglyceridemia, atorvastatin reduces the concentration of total cholesterol, LDL-C, VLDL-C, apo-B and TG and increases the concentration of HDL-C. In patients with dysbetalipoproteinemia, it reduces the concentration of intermediate-density lipoprotein cholesterol (IDL-C).
In patients with type IIa and IIb hyperlipoproteinemia according to the Fredrickson classification, the average increase in HDL-C concentration during treatment with atorvastatin (10-80 mg) compared to baseline is 5.1-8.7% and is independent of dose. There is a significant dose-dependent decrease in the ratios: total cholesterol/HDL-C and LDL-C/HDL-C by 29-44% and 37-55%, respectively.
Atorvastatin at a dose of 80 mg significantly reduces the risk of ischemic complications and mortality by 16% after a 16-week course, and the risk of readmission for angina pectoris accompanied by signs of myocardial ischemia by 26%. In patients with different baseline LDL-C concentrations (with non-Q wave myocardial infarction and unstable angina, men and women, in patients younger and older than 65 years), atorvastatin causes a reduction in the risk of ischemic complications and mortality.
The decrease in plasma LDL-C concentration correlates better with the dose of atorvastatin than with its plasma concentration. The dose is selected taking into account the therapeutic effect (see section “Method of administration and dosage”).
The therapeutic effect is achieved 2 weeks after the start of therapy, reaches a maximum after 4 weeks and persists throughout the entire period of therapy.
Special instructions
Special instructions
Before starting therapy with Atorvastatin, the patient must be prescribed a standard cholesterol-lowering diet, which he must follow during the entire treatment period.
If severe adverse effects occur, use of Atorvastatin should be discontinued.
Effect on the liver
As with the use of other lipid-lowering drugs of this class, after treatment with atorvastatin, a moderate (more than 3 times compared to the upper limit of normal) increase in the serum activity of “liver” transaminases AST and ALT was noted. Increased activity of liver transaminases was usually not accompanied by jaundice or other clinical manifestations. When the dose of atorvastatin was reduced, or the drug was temporarily or completely discontinued, the activity of “liver” transaminases returned to the initial level. Most patients continued to take atorvastatin at a reduced dose without any clinical consequences.
Before starting therapy, 6 weeks and 12 weeks after starting the use of Atorvastatin or after increasing its dose, as well as during the entire course of treatment, liver function tests should be monitored. Liver function should also be examined if clinical signs of liver damage appear. If the activity of “liver” transaminases increases, their activity should be monitored until it returns to normal. If an increase in AST or ALT activity by more than 3 times compared to the upper limit of normal persists, a dose reduction or discontinuation of the drug is recommended.
Atorvastatin should be used with caution in patients who consume significant amounts of alcohol and/or have a history of liver disease. Active liver disease or persistently increased activity of hepatic transaminases in the blood plasma of unknown origin is a contraindication to the use of Atorvastatin.
Effect on skeletal muscles
Myalgia has been reported in patients receiving atorvastatin. The diagnosis of myopathy (muscle pain and weakness in combination with an increase in creatine phosphokinase activity more than 10 times the upper limit of normal) should be considered in patients with diffuse myalgia, muscle soreness or weakness, and/or a marked increase in CPK activity. Therapy with Atorvastatin should be discontinued in the event of a marked increase in CPK activity or in the presence of confirmed or suspected myopathy. The risk of myopathy during treatment with other drugs of this class increased with simultaneous use of cyclosporine, fibrates, erythromycin, nicotinic acid in lipid-lowering doses (more than 1 g / day), nefazodone, some antibiotics, azole antifungals, HIV protease inhibitors.
Many of these drugs inhibit CYP3A4-mediated metabolism and/or drug transport. It is known that the CYP3A4 isoenzyme is the main liver isoenzyme involved in the biotransformation of atorvastatin. When prescribing Atorvastatin in combination with fibrates, erythromycin, immunosuppressants, azole antifungals or nicotinic acid in lipid-lowering doses, you should carefully weigh the expected benefits and possible risks. Patients should be monitored regularly for muscle pain or weakness, especially during the first months of treatment and during periods of increasing dosage of any of these drugs. If combination therapy is necessary, the use of these drugs in lower initial and maintenance doses should be considered. In such situations, periodic determination of CPK activity can be recommended, although such monitoring does not prevent the development of severe myopathy.
When using atorvastatin, like other statins, rare cases of rhabdomyolysis with acute renal failure caused by myoglobinuria have been described. If symptoms of possible myopathy occur or there is a risk factor for renal failure secondary to rhabdomyolysis (eg, severe acute infection, hypotension, major surgery, trauma, metabolic, endocrine and fluid disturbances, and uncontrolled seizures), therapy with Atorvastatin should be temporarily discontinued or completely discontinued.
In the differential diagnosis of chest pain, one should take into account the possibility of an increase in serum CPK activity when using the drug Atorvastatin.
Attention! Patients should be warned to seek immediate medical attention if they experience unexplained pain or muscle weakness, especially if accompanied by malaise or fever.
The drug Atorvastatin contains lactose, and therefore its use in patients with lactase deficiency, lactose intolerance and glucose-galactose malabsorption syndrome is contraindicated.
Impact on the ability to drive vehicles and machinery
Caution should be exercised when driving vehicles and other technical devices that require increased concentration and speed of psychomotor reactions (risk of dizziness).
Active ingredient
Active ingredient
Atorvastatin
Composition
Composition
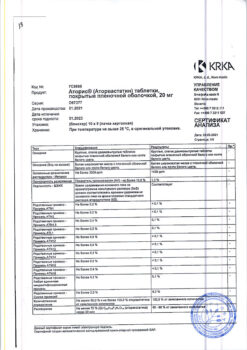
1 tablet contains:
active substance:
atorvastatin calcium trihydrate (in terms of atorvastatin) – 10.00 mg;
excipients:
microcrystalline cellulose – 49.68 mg,
lactose monohydrate – 40.00 mg,
calcium carbonate – 33.00 mg,
crospovidone – 7.50 mg,
sodium carboxymethyl starch (sodium starch glycolate) – 4.50 mg,
hyprolose (hydroxypropylcellulose) – 3.00 mg,
magnesium stearate – 1.50 mg;
film cover:
[hypromellose – 2.250 mg, talc – 0.882 mg, hyprolose (hydroxypropylcellulose) – 0.873 mg, titanium dioxide – 0.495 mg] or [dry mixture for film coating containing hypromellose (50.0%), talc (19.6%), hyprolose (hydroxypropylcellulose) (19.4%), titanium dioxide (11.0%)] – 4,500 mg.
Contraindications
Contraindications
hypersensitivity to any of the components of the drug;
active liver disease;
an increase in the activity of “liver” transaminases in the blood plasma of unknown origin by more than 3 times compared to the upper limit of normal;
skeletal muscle diseases;
lactase deficiency, lactose intolerance, glucose-galactose malabsorption syndrome;
pregnancy and breastfeeding;
age under 18 years (insufficient clinical data on effectiveness and safety for this age group).
With caution
Use in patients who abuse alcohol or in patients with a history of liver disease.
Side Effects
Side Effects
World Health Organization (WHO) classification of the incidence of side effects: very often – ≥1/10, often – from ≥1/100 to <1/10, infrequently - from ≥1/1000 to <1/100, rarely - from ≥1/10000 to <1/1000, very rarely - <1/10000, including isolated reports, frequency unknown - by It was not possible to determine the frequency of occurrence using the available data.
From the nervous system:
often – insomnia, headache, dizziness, paresthesia, asthenic syndrome;
infrequently – peripheral neuropathy, amnesia, hypoesthesia.
From the senses:
infrequently – tinnitus;
rarely – nasopharyngitis, nosebleeds.
From the cardiovascular system:
palpitations, symptoms of vasodilation, migraine, postural hypotension, increased blood pressure, phlebitis, arrhythmia.
From the hematopoietic system:
infrequently – thrombocytopenia.
From the respiratory system:
often – chest pain.
From the digestive system:
often – nausea, diarrhea, abdominal pain, dyspepsia, constipation, flatulence (bloating);
infrequently – impaired taste perception, vomiting, pancreatitis;
rarely – hepatitis, cholestatic jaundice.
From the musculoskeletal system and connective tissue:
often – myalgia, arthralgia, back pain, swelling of the joints;
uncommon – myopathy, muscle cramps;
rarely – myositis, rhabdomyolysis, tendonopathy (in some cases with tendon rupture).
From the genitourinary system:
infrequently – sexual dysfunction, secondary renal failure.
From the skin:
often – skin rash, itching;
infrequently – urticaria;
very rarely – angioedema, alopecia, bullous rash, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis.
Allergic reactions:
often – allergic reactions;
very rarely – anaphylaxis.
Laboratory indicators:
infrequently – increased activity of aminotransferases (AST, ALT), increased activity of serum creatine phosphokinase (CPK);
very rarely – hypoglycemia, hyperglycemia.
Other:
often – peripheral edema;
uncommon – weakness, fatigue, fever, anorexia, weight gain.
During post-marketing use of statins, including atorvastatin, the following side effects have been reported: memory loss or decrease, depression, sleep disturbances, including insomnia and nightmares, sexual dysfunction, gynecomastia, hyperglycemia, increased concentrations of glycosylated hemoglobin, isolated cases of interstitial lung disease (especially with long-term use), cases of immune-mediated necrotizing myopathy, thrombocytopenia.
Interaction
Interaction
The risk of developing myopathy with rhabdomyolysis and renal failure during treatment with HMG-CoA reductase inhibitors increases with simultaneous use with cyclosporine, antibiotics (erythromycin, clarithromycin, quinupristin/dalfopristin), HIV protease inhibitors (indinavir, ritonavir), antifungal drugs (fluconazole, itraconazole, ketoconazole), nefazodone. All of these drugs inhibit the CYP3A4 isoenzyme, which is involved in the metabolism of atorvastatin in the liver.
A similar interaction is possible with the simultaneous use of atorvastatin with fibrates and nicotinic acid in lipid-lowering doses (more than 1 g per day).
When used concomitantly with HIV protease inhibitors, hepatitis C inhibitors, clarithromycin and itraconazole, caution should be exercised and the lowest effective dose of atorvastatin should be used.
CYP3A4 isoenzyme inhibitors
Since atorvastatin is metabolized by the CYP3A4 isoenzyme, co-administration of atorvastatin with inhibitors of the CYP3A4 isoenzyme may lead to increased plasma concentrations of atorvastatin. The degree of interaction and potentiation effect is determined by the variability of the effect on the CYP3A4 isoenzyme.
Inhibitors of the transport protein OATP1B1
Atorvastatin and its metabolites are substrates of the transport protein OATP1B1. OATP1B1 inhibitors (eg, cyclosporine) may increase the bioavailability of atorvastatin.
Erythromycin/clarithromycin
With simultaneous use of atorvastatin and erythromycin or clarithromycin, which inhibit the CYP3A4 isoenzyme, an increase in the concentration of atorvastatin in the blood plasma was observed.
Protease inhibitors
The simultaneous use of atorvastatin with protease inhibitors, known as inhibitors of the CYP3A4 isoenzyme, is accompanied by an increase in the concentration of atorvastatin in the blood plasma.
Diltiazem
Co-administration of atorvastatin at a dose of 40 mg with diltiazem at a dose of 240 mg leads to an increase in the concentration of atorvastatin in the blood plasma.
Itraconazole
The simultaneous use of atorvastatin and itraconazole led to an increase in the concentration of atorvastatin in the blood plasma.
Grapefruit juice
Since grapefruit juice contains one or more components that inhibit the CYP3A4 isoenzyme, excessive consumption (more than 1.2 L per day) may cause an increase in plasma concentrations of atorvastatin.
Inducers of the CYP3A4 isoenzyme
Concomitant use of atorvastatin with inducers of the CYP3A4 isoenzyme (for example, efavirenz, phenytoin or rifampicin) may lead to a decrease in the concentration of atorvastatin in the blood plasma. Due to the dual mechanism of interaction with rifampicin (an inducer of the CYP3A4 isoenzyme and an inhibitor of the hepatocyte transport protein OATP1B1), the simultaneous use of atorvastatin and rifampicin is recommended, since delayed administration of atorvastatin after taking rifampicin leads to a significant decrease in the concentration of atorvastatin in the blood plasma.
Antacids
With simultaneous oral administration of atorvastatin and a suspension containing magnesium and aluminum hydroxides, the concentration of atorvastatin in the blood plasma decreases.
Phenazon
Atorvastatin does not affect the pharmacokinetics of phenazone, so interaction with other drugs metabolized by the same cytochrome enzymes is not expected.
Colestipol
With simultaneous use of colestipol, the concentration of atorvastatin in the blood plasma decreased by approximately 25%, however, the lipid-lowering effect of the combination of atorvastatin and colestipol was superior to that of each drug separately.
Digoxin
When digoxin was used in combination with atorvastatin at a dose of 80 mg/day, digoxin concentrations increased by approximately 20%, so such patients should be monitored.
Oral contraceptives
With the simultaneous use of atorvastatin and an oral contraceptive containing norethisterone and ethinyl estradiol, it is possible to increase the absorption of contraceptives and increase their concentration in the blood plasma. This effect should be taken into account when choosing an oral contraceptive for a woman taking atorvastatin.
Terfenadine
Atorvastatin, when used concomitantly, did not have a clinically significant effect on the pharmacokinetics of terfenadine.
Warfarin
Concomitant use of atorvastatin with warfarin may increase the effect of warfarin on blood coagulation parameters (decreased prothrombin time) in the first days. This effect disappears after 15 days of simultaneous use of these drugs.
Amlodipine
With simultaneous use of atorvastatin at a dose of 80 mg and amlodipine at a dose of 10 mg, the pharmacokinetics of atorvastatin at steady state did not change.
Fusidic acid
There have been cases of rhabdomyolysis in patients using atorvastatin and fusidic acid.
Colchicine
Cases of myopathy have been reported with concomitant use of atorvastatin and colchicine. Caution should be exercised during combination therapy with these drugs.
Cimetidine
When studying the interaction of atorvastatin with cimetidine, no signs of clinically significant interaction were found.
Other concomitant therapy
Concomitant use of atorvastatin with drugs that reduce the concentration of endogenous steroid hormones (including cimetidine, ketoconazole, spironolactone) increases the risk of a decrease in endogenous steroid hormones (caution should be exercised).
In clinical studies, atorvastatin was used in combination with antihypertensive agents and estrogens, which were prescribed as replacement therapy; no symptoms of clinically significant adverse interaction were noted. Interaction studies with specific drugs have not been conducted.
Overdose
Overdose
Cases of overdose have not been described.
In case of overdose, the following general measures are necessary: monitoring and maintaining vital functions of the body, as well as preventing further absorption of the drug (gastric lavage, taking activated charcoal or laxatives).
If myopathy develops with subsequent rhabdomyolysis and acute renal failure, the drug should be immediately discontinued and an infusion of a diuretic and sodium bicarbonate should be started.
Rhabdomyolysis can lead to hyperkalemia, which requires intravenous administration of calcium chloride solution or calcium gluconate solution, infusion.
5% dextrose (glucose) solution with insulin, use of potassium exchange resins.
Since the drug actively binds to plasma proteins, hemodialysis is not effective.
Manufacturer
Manufacturer
Vertex, Russia
Additional information
| Manufacturer | Vertex, Russia |
|---|---|
| Medication form | pills |
| Brand | Vertex |
Other forms…
Related products
Buy Atorvastatin-Vertex, 10 mg 90 pcs with delivery to USA, UK, Europe and over 120 other countries.